Renal Cell Carcinoma with Level II Inferior Vena Cava Thrombi: Operative Steps
A B S T R A C T
The incidence of venous tumor thrombi extension to the inferior vena cava (IVC) in renal cell carcinoma (RCC) has markedly increased recently due to the advances in diagnostic modalities. Such vascular invasion implies a heightened biologic behaviour and a surgical challenge during the course of treatment. Several studies have examined the prognostic significance of the level of venous extension. It has been suggested recently that long-term survival may be significantly better in patients with renal vein involvement than IVC involvement. We describe the operative steps in the treatment of level II IVC thrombus in this report.
Keywords
Renal cell carcinoma, inferior vena cava thrombus, magnetic resonance imaging
Introduction
Renal cell carcinoma (RCC) has a unique feature of venous migration and thrombus formation, with significant therapeutic and prognostic implications [1-4]. This intraluminal growth can extend into the inferior vena cava (IVC) with cephalad migration as far as the right atrium or beyond. Venous/IVC thrombus is known to occur in 4%-10% of patients with renal cell carcinoma, and 2%-16% of these have tumors extending into the right atrium [2, 3, 5]. It is rather intriguing in respect to this cancer’s behaviour, that in-spite of vena caval extension, many patients are free of metastases [6, 7]. Aggressive surgical approach including radical nephrectomy and IVC thrombectomy can cure 45-70% of patients [8].
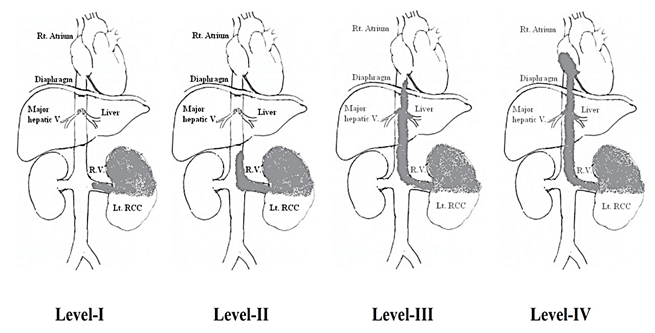
Staging of the level of IVC thrombus is as follows: I, adjacent to the ostium of the renal vein; II, extending up to the lower aspect of the liver; III, involving the intrahepatic portion of the IVC but below the diaphragm; and IV, extending above the diaphragm (Figure 1) [8]. Traditionally, venacavography has been used to detect and diagnose IVC involvement and was considered as the gold standard [9]. Computed tomography (CT) has been extremely useful in demonstrating the cephalad extent of the thrombus and also in diagnosing occult metastasis in the majority of cases [5]. When contrast enhancement of the renal vein is at its peak, venous extension is optimally visualized during the corticomedullary phase of enhancement, as a low density-filling defect within the vein. Enhancement pattern of thrombi helps to distinguish tumor thrombi from the bland ones. However, conventional CT has a lower sensitivity in delineating the thrombus’s superior margin compared to MRI (76% and 100% respectively) [5]. Currently, magnetic resonance imaging (MRI) is considered as the gold standard for delineating the extent and level of tumor thrombi in the IVC and staging of RCC with a sensitivity of 96-100% and it can also rule out caval wall invasion so that the exact surgical procedure can be planned [10]. Invasive contrast-enhanced imaging is reserved for patients in whom MRI and CT findings are equivocal or for whom MRI and CT are contraindicated [8].
Figure 1: Shows levels of renal vein and IVC thrombus.
Surgical Approach
The surgical objectives include, (i) complete resection of tumor and its caval thrombi, (ii) prevention of tumor embolism by temporary placement of an IVC filter or plication of the IVC in its suprahepatic/retrohepatic segment, (iii) minimizing blood loss, (iv) maintenance of hemodynamic stability, and (v) prevention of vital organ ischaemia [11]. The surgical incision for an infra-hepatic IVC thrombi is a midline transperitoneal incision that provides a generous access to the IVC. Bilateral subcostal approach can also be used for equivalent exposure.
The surgical approach is tailored to the level of IVC thrombus, but uniformly begins with careful mobilization of the kidney and early ligation of the arterial blood supply. In general, level I thrombi are isolated by a Satinsky clamp and are thus readily addressed. Level II thrombi require sequential clamping of the caudal IVC, contralateral renal vasculature, and cephalad IVC along with mobilization of the relevant segment of the IVC and occlusion of lumbar veins. The renal ostium is then opened, and the thrombus is removed, all in a bloodless field. When tumor thrombus invades the wall of the vena cava, aggressive resection of the involved cava and attainment of negative surgical margins are required to minimize the risk of recurrence.
Case Report
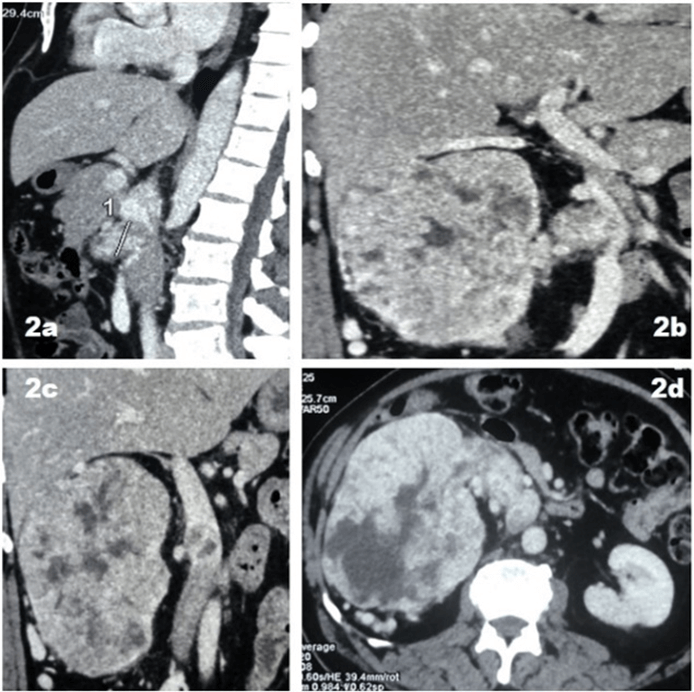
A 56-year-old man presented to the neuro-physician with complaints of pain in the neck and one episode of painless total haematuria. Right upper abdominal mass and Grade III right varicocele was found on clinical examination. Ultrasonography of abdomen revealed right renal mass. Contrast enhanced CT Abdomen and Pelvis (Figure 2) revealed a right renal mass measuring 13.1 x 12.4 x 14.6 cm. The lesion was seen to extend medially into right renal vein and infra-hepatic portion of IVC (3 cms from ostium of renal vein). Multiple dilated and tortuous veins draining into right iliac vein were noted. Biochemical and haematological parameters were within normal limits except hypercalcemia (11.6 mg/dL).
Figure 2: a-d) Contrast enhanced CT shows IVC thrombus below the level of liver, extending upto 3cm from the renal vein ostia.
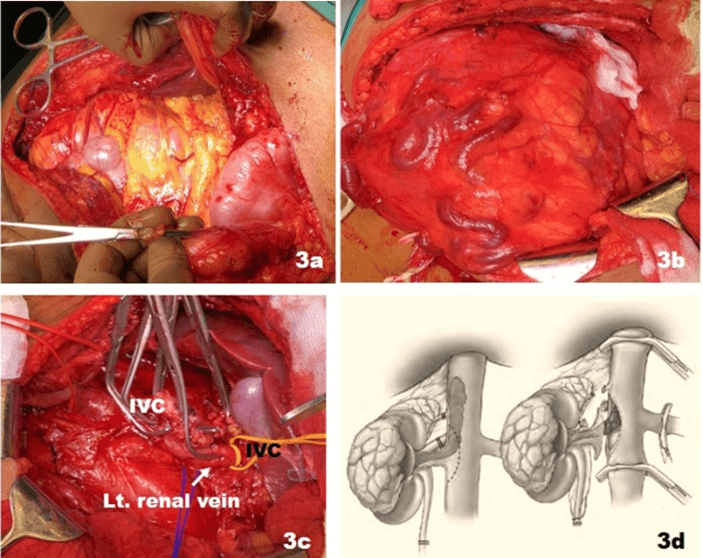
A diagnosis of right renal mass with renal vein invasion extending up to the infra-hepatic IVC (Level II) was made. Patient was counselled regarding the complications of the procedure and the prognosis of the disease. He was surgically explored using a bilateral Chevron incision (Figure 3). The right colon was reflected medially, and the anterior surface of tumor visualized. The tumor was separated from the surrounding tissue using blunt and sharp dissection. The right gonadal vein was identified and traced up to the IVC.
Figure 3: a) Bilateral Chevron incision. b) Huge Rt renal mass visualized with prominent veins on the surface. c) The three-clamp technique used to achieve vascular control. d) Diagrammatic representation of the three-clamp technique.
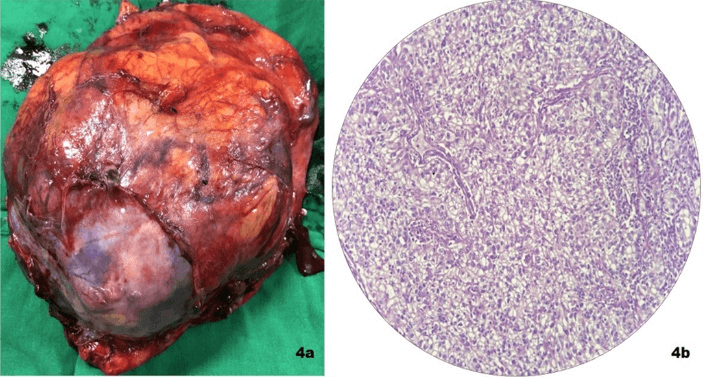
Gonadal vein was clipped and divided at the level of IVC. The right renal artery was identified postero-superior to the right renal vein. It was ligated and cut. The IVC was mobilized both above and below the level of right renal vein. Similarly, the left renal vein was mobilized at its entry level with IVC. Clamps were applied sequentially over the distal IVC, at the left renal vein and proximal IVC above the level of thrombus. Cavotomy was performed and thrombus extracted from the IVC. The rest of the kidney along with the thrombus was delivered. The cavotomy was closed with 5-0 polypropylene sutures. Haemostasis was achieved and abdomen closed in layers. Histopathological examination revealed a clear cell renal cell carcinoma, Fuhrman Grade III (Figure 4).
Figure 4: a) Nephrectomy specimen measuring 13.1 x 12.4 x 14.6 cm. b) Histo-pathological examination high power 100x, H & E staining shows clear cells with hyper chromatic nuclei.
Discussion
The prognosis of these patients with IVC tumor thrombi is difficult to predict due to a wide range of variations in clinical behaviour [12]. Although involvement of the IVC in renal cancer is generally not a vascular invasion by the neoplastic process but mostly an intraluminal extension of the tumor mass, such intravascular growth implies a heightened biologic behaviour of the tumor. Total resection of tumor affords the best chance of cure and long-term survival when no distant metastases are present [5]. Surgical treatment even in the presence of distant metastases is the best option in these patients due to absence of effective alternative treatment. Advances in immunotherapy may help in increasing the survival of these patients if aggressive surgery is combined with targeted therapy [11].
Conflicts of Interest
None.
Funding
None.
Article Info
Article Type
Case ReportPublication history
Received: Wed 17, Feb 2021Accepted: Mon 05, Apr 2021
Published: Fri 23, Apr 2021
Copyright
© 2023 R. B. Nerli . This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2021.03.12
Author Info
R. B. Nerli Priyeshkumar Patel Shridhar C. Ghagane Shashank Patil Adarsh Sanikop Shoubhik Chandra
Corresponding Author
R. B. NerliDepartment of Urology, JN Medical College, KLE Academy of Higher Education & Research (Deemed-to-be-University), JNMC Campus, Belagavi, Karnataka, India
Figures & Tables
References
1.
Ciancio G,
Soloway M (2005) Resection of the abdominal IVC for complicated renal cell
carcinoma with tumor thrombus. BJU Int 96: 815-818. [Crossref]
2.
Nerli RB, Hiremath MB, Prabha V, Malur P,
Borges A (2010) Primitive neuroectodermal tumor (PNET) of the kidney with level
IV inferior vena caval thrombus: a case report. Recent Res Sci Technol 2.
3.
Nerli RB, Dixit MD, Mohan G, Prabha V,
Devaraju S et al. (2010) Renal Cell Carcinoma with Vena Caval Thrombus
Extending into the Right Atrium: Our Experience. Int J Nephrol Urol 2: 497-503.
4.
Zisman A, Wieder
JA, Pantuck AJ, Chao DH, Dorey F et al. (2003) Renal cell carcinoma with tumor
thrombus extension: biology, role of nephrectomy and response to immunotherapy.
J Urol 169: 909-916. [Crossref]
5.
Nouh MAAM, Inui
M, Kakehi Y (2008) Renal cell carcinoma with IVC thrombi; current concepts and
future perspectives. Clin Med Oncol
2: 247-256. [Crossref]
6.
Gettman MT, Blute
ML (2002) Update on pathologic staging of renal cell carcinoma. Urology 60: 209-217. [Crossref]
7.
Wotkowicz C,
Wszolek MF, Libertino JA (2008) Resection of renal tumors invading the vena
cava. Urol Clin North Am 35: 657-671.
[Crossref]
8.
Campbell SC and
Lane BR (2016) Malignant
renal tumors. In Wein AJ, Kavoussi LR, Partin AW and Peters CA, Eds, Campbell-Walsh Urology, 11th
edition, Elsevier-Saunders, Philadelphia 1314.
9.
Kallmann DA, King
BF, Hattery RR, Charboneau JW, Ehman RL et al. (1992) Renal vein and inferior
vena cava tumor thrombus in renal cell carcinoma: CT, US, MRI and
venacavography. J Comput Assist Tomogr 16: 240-247. [Crossref]
10.
Lawrentschuk N,
Gani J, Riordan R, Esler S, Bolton DM (2005) Multidetector computed tomography
vs magnetic resonance imaging for defining the upper limit of tumour thrombus
in renal cell carcinoma: a study and review. BJU Int 96: 291-295. [Crossref]
11.
Jibiki M, Iwai T,
Inoue Y, Sugano N, Kihara K et al. (2004) Surgical strategy for treating renal
cell carcinoma with thrombus extending into the inferior vena cava. J Vasc
Surg 39: 829-835. [Crossref]
12.
Kaplan S, Ekici
S, Dogan R, Demircin M, Ozen H et al. (2002) Surgical management of renal cell
carcinoma with inferior vena cava tumor thrombus. Am J Surg 183: 292-299.
[Crossref]
