Case Report
Inducible Laryngeal Obstruction/Vocal Cord Dysfunction and the Role It Plays in Refractory Asthma

Jorge Villalpando, Jay I Peters* and Sandra G Adams
UT Health San Antonio and the South Texas Veterans Health Care System, San Antonio, TX, USA
*Address for Correspondence: Jay I Peters, UT Health San Antonio and The South Texas Veterans Health Care System, San Antonio, TX, USA, Email: PETERS@uthscsa.edu
Dates: Submitted: 01 August 2017; Approved: 22 August 2017; Published: 23 August 2017
How to cite this article: Villalpando J, Peters JI, Adams SG. Inducible Laryngeal Obstruction/Vocal Cord Dysfunction and the Role It Plays in Refractory Asthma. Arch Asthma Allergy Immunol. 2017; 1: 036-039. DOI: 10.29328/journal.aaai.1001005
Copyright License: © 2017 Villalpando J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Chronic asthma accounts for a significant amount of unscheduled office and emergency department (ED) visits. According to the latest World Health Organization statistics, asthma worldwide affects 300 million individuals and creates a substantial health burden by restricting the patient’s lifetime activities. Data estimate that asthma causes a loss of disability-adjusted life years over 150,000/year [1]. While most individuals with asthma can be controlled with current therapies, 5-10% of patients have difficult-to-control/refractory asthma. Severe or refractory asthma places a significant burden on the patient and often requires treatment with systemic glucocorticoids, which have significant side effects. The American Thoracic Society and the European Respiratory Society define refractory asthma as asthma that requires treatment with high-dose inhaled corticosteroids (ICS) plus a second controller and/or systemic corticosteroids to prevent it from becoming ‘‘uncontrolled’’ or asthma that remains ‘‘uncontrolled’’ despite this aggressive therapy. To fully meet this definition the diagnosis of asthma needs to be confirmed and comorbidities addressed as well. The above are considered major criteria for severe asthma and only one needs to be present for considering the diagnosis of refractory asthma [2]. For these reasons, clinicians must learn to identify and formulate additional diagnoses of “asthma imitators” [3]. One of the more common disorders associated with difficult-to-control asthma is vocal cord dysfunction (VCD) [4]. This disorder is known by many names, but current nomenclature endorsed by European and American societies correctly refers it as “Inducible Laryngeal Obstruction” (ILO) [5]. The following case demonstrates the importance of recognizing the clinical and spirometric features of ILO when asthma remains “refractory” to multiple therapies.
Case Presentation
History
29-year-old female physician was referred by a community pulmonologist to our medical center for “difficult-to-control asthma”. Her past medical history included childhood asthma between ages 8-10 years old with nocturnal awakenings due to dyspnea. Around the age of 19 years old, she described episodic “bronchitis and wheezing” during the week before her menses. At the time of assessment, the patient had recently had an ED visit (one-month ago) for a “severe asthma exacerbation”. She had recurrent wheezing and shortness of breath along with chest tightness lasting up to 2 hours. Her symptoms had been getting worse during the past eight months. Her known triggers were cold air, perfume, dust and environmental tobacco smoke (ETS). The patient was a competitive athlete in college, but was now unable to walk up one flight of stairs due to profound dyspnea. She was a lifetime non-smoker and had allergies to sulfa, aspirin and ibuprofen. She was currently optimized on appropriate asthma controller inhalers and a leukotriene modifier and was considered to have refractory asthma.
Examination and investigations
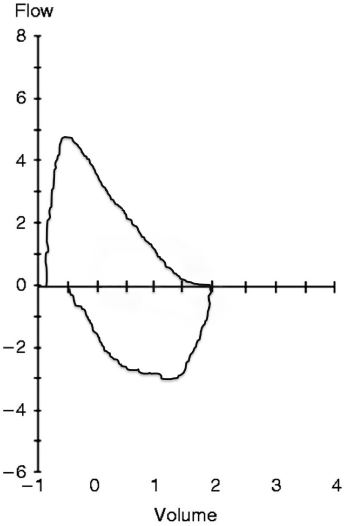
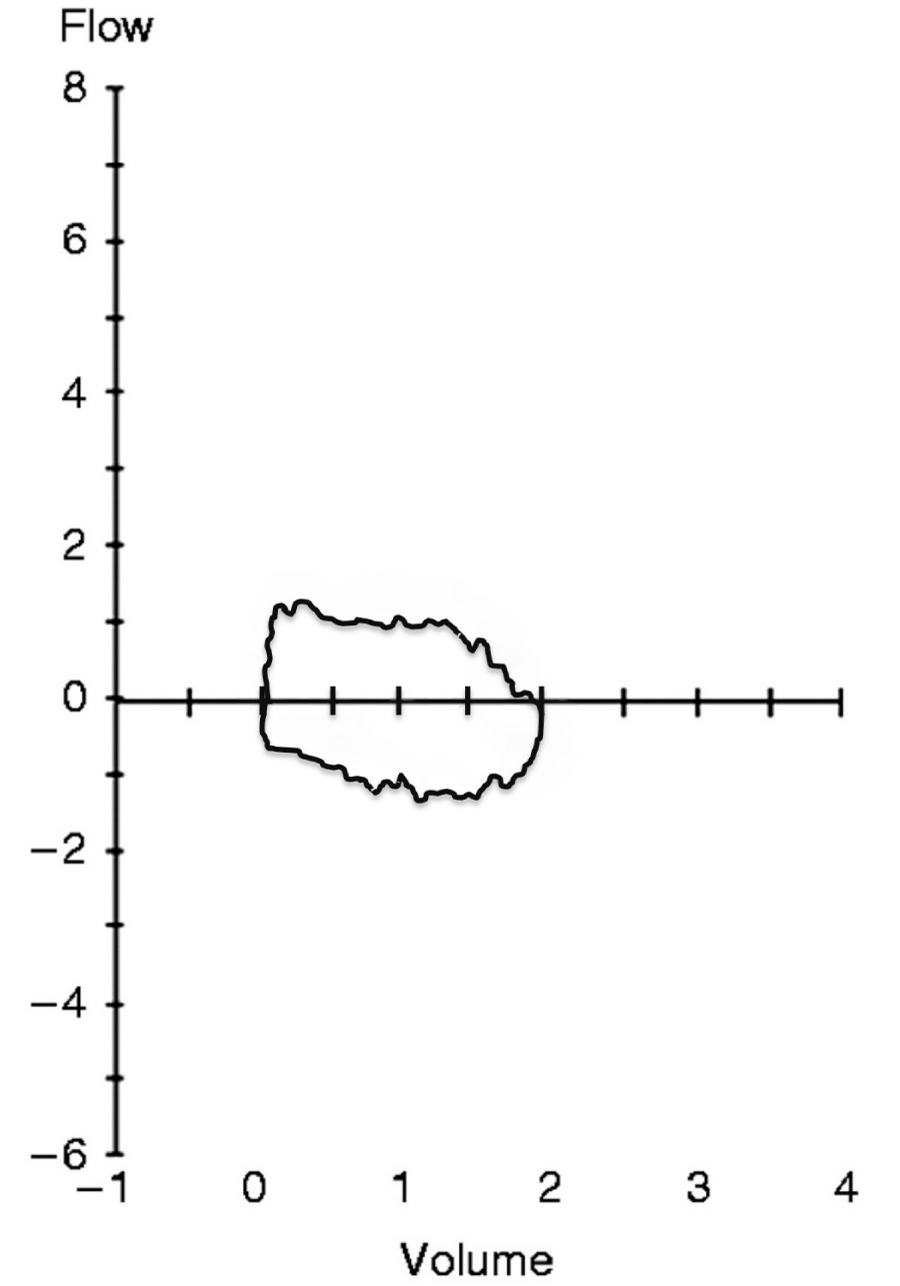
On physical examination, her vital signs and lung and heart examinations were unremarkable. Her prior workup included (1) a cardiac echocardiogram with normal left ventricular function and a normal pulmonary arterial systolic pressure, (2) a negative cardiac stress test and (3) pulmonary function tests (PFTs) that were completely normal: FEV1 3.04L (98%), FEV1/FVC 91% and DLCO 102%. Basic laboratory studies were all normal: including complete blood count, brain natriuretic peptide (BNP), D-dimer, total eosinophil count and Ig-E level. Chest radiograph and high-resolution chest CT scan were normal without signs of obvious pleural or parenchymal disease. Because her symptoms were markedly exacerbated and were severe during exertion, we then performed spirometry before (Figure 1) and after exercise (Figure 2). Her pre-exercise flow volume loop was normal (Figure 1), but post-exercise, her inspiratory and expiratory flow volume loops were markedly flattened (Figure 2), consistent with severe paradoxical vocal fold motion (PVFM). The patient underwent bronchoscopy, which demonstrated sustained adduction of her vocal cords during inspiration and expiration and a posterior “chink” (accounting for her atypical flow-volume loop). Her bronchoalveolar lavage (BAL) revealed 4% eosinophils and her bronchial biopsies demonstrated mild thickening of the basement membrane.
Management
The patient was referred to a speech therapist and trained to control her breathing and relax her airways. She reported marked improvement in symptoms and disease burden requiring fewer medications to control her symptoms and had no ED visits over the next 18 months.
Case Discussion
A common approach for a patient with refractory asthma includes formulating a broad differential and assessing the patient’s compliance with medications, their environment and their inhaler technique [6]. Patients need to be screened for contributing factors such as gastroesophageal reflux, sinusitis, rhinitis and certain exacerbating medications (e.g., aspirin, non-steroidal anti-inflammatory drugs, beta-blockers, etc.) [7,8].
The differential diagnoses for asthma includes obstructive bronchiolitis, airway tumors, tracheal stenosis, hypersensitivity pneumonitis, sarcoidosis, pulmonary emboli and inducible laryngeal obstruction/vocal cord dysfunction (ILO/VCD). ILO is commonly misdiagnosed as asthma or allergic reactions involving the airways. This misdiagnosis often leads to inappropriate disease management with systemic steroids, frequent clinic visits and overall impairment of the quality of life of the patient. ILO may also be misdiagnosed as exercise-induced asthma and may appear after exposure to inhalational irritants, induced by exercise, and is often associated with gastroesophageal reflux disease (GERD) [9]. What may be surprising to some clinicians is that ILO may coexist with asthma in up to 32% of patients, further complicating the management [10]. ILO is characterized by paradoxical adduction of the anterior 2/3 of the vocal cords typically occurring during inspiration (85%), but may also be noted during expiration, as in our patient. This paradoxical motion of the vocal cords obstructs airflow, producing wheezing, cough, shortness of breath, and chest tightness accounting for the typical clinical presentation. Because ILO is related to subconscious adduction of the vocal cords during inspiration, the paradoxical movement rarely occurs during sleep. Patients with ILO commonly complain of throat tightness, voice changes, and difficulty “getting air in” more than getting air out. Attacks tend to have a diurnal pattern rather than nocturnal in contrast to uncontrolled asthma. Episodes are often preceded by cough and fail to respond to bronchodilators [9]. On physical examination, inspiratory wheezing may be heard during the acute episode and tends not to worsen with cough. Symptoms fail to improve or even worsen rather than improve with inhalers in a subset of patients with isolated ILO, without concomitant asthma component.
Performing pre and post exercise PFTs may be helpful in diagnosing ILO showing a FEV1 out of proportion to airway resistance or an abnormal flow-volume loop. These findings support the diagnosis; however, the gold standard for diagnosing ILO is direct laryngoscopy of the vocal cords while the patient is actively symptomatic [11]. Speech therapy is the definitive long-term treatment for ILO and has been reviewed in detail [12]. It focuses on breathing exercises that train the patient to avoid or reduce paradoxical vocal cord adduction.
Conclusion
Inducible laryngeal obstruction should be considered in patients with difficult-to-control asthma as an alternative or concomitant diagnosis. Effective treatments are available for both conditions, but accurate diagnosis is important because management options differ based on whether the patient has ILO, asthma or both.
Learning points:
1. Severe refractory asthma can mimic a wide spectrum of respiratory diseases.
2. One of the more common disorders associated with difficult-to-control asthma is inducible laryngeal obstruction.
3. When presented with an established diagnosis of “asthma” perform the necessary confirmatory tests (direct laryngoscopy or bronchoscopy).
4. In the patient has concomitant asthma, remove environmental triggers, confirm compliance, maximize anti-inflammatory therapy.
5. Consider an alternative diagnosis and directed therapy when the patient remains symptomatic despite appropriate therapy.
REFERENCES
- World Health Organization. Media Center. Asthma Key Facts. 2017; Ref.: https://goo.gl/T97UX8
- Chung K, Wenzel S, Brozek J, Bush A, Castro M, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014; 43: 343-373. Ref.: https://goo.gl/SrCSCu
- Walsted ES, Hull JH, Sverrild A, Porsbjerg C, Backer V. Bronchial provocation testing does not detect exercise-induced laryngeal obstruction. J Asthma. 2017; 54: 77-83. Ref.: https://goo.gl/PmRDA9
- Balkissoon R, Blager F. Vocal cord dysfunction Often Misdiagnosed and Treated Inappropriately. Medical Scientific. 2002; 19. Ref.: https://goo.gl/HxM7v4
- Christensen PM, Heimdal JH, Christopher KL, Bucca C, Cantarella G, et al. ERS/ELS/ACCP 2013 international consensus conference nomenclature on inducible laryngeal obstructions. Eur Resp Rev. 2015; 24: 445-450. Ref.: https://goo.gl/JkAbxh
- Heaney LG, Brightling CE, Menzies-Gow A, Stevenson M, Niven RM, et al. British Thoracic Society Difficult Asthma Network. Thorax. 2010; 65: 787-94. Ref.: https://goo.gl/sot96d
- Chanez P, Wenzel SE, Anderson GP, Anto JM, Bel EH, et al. Severe asthma in adults: what are the important questions? J Allergy Clin Immunol. 2007; 119: 1337-1348. Ref.: https://goo.gl/BbL4Mi
- Holgate ST. Polosa R. The mechanisms, diagnosis, and management of severe asthma in adults. Lancet. 2006; 368: 780-793. Ref.: https://goo.gl/CTx1Rf
- Morris MJ, Christopher KL. Diagnostic criteria for the classification of vocal cord dysfunction. Chest. 2010; 138: 1213-1223. Ref.: https://goo.gl/R2hNbo
- Yelken K, Yilmaz A, Guven M, Eyibilen A, Aladag I. Paradoxical vocal fold motion dysfunction in asthma patients. Respirology. 2009; 14: 729-733. Ref.: https://goo.gl/pLQ9Td
- McNicholl DM, Megarry J, McGarvey LP, Riley MS, Heaney LG. The utility of cardiopulmonary exercise testing in difficult asthma. Published in Chest. 2011; 139: 1117-1123. Ref.: https://goo.gl/97pYaQ
- Hicks M, Brugman SM, Katial R. Vocal cord dysfunction/paradoxical vocal fold motion. Prim Care. 2008; 35: 81-103. Ref.: https://goo.gl/5AaJeb