More Information
Submitted: 23 September 2020 | Approved: 12 October 2020 | Published: 14 October 2020
How to cite this article: Mahalakshmi S, Sakthi A, Saravanan L, Nidhi S. Effect of sperm DNA fragmentation on ICSI outcome: A prospective study. Clin J Obstet Gynecol. 2020; 3: 132-135.
DOI: 10.29328/journal.cjog.1001066
ORCiD: orcid.org/0000-0003-1468-8996
Copyright License: © 2020 Mahalakshmi S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Endometrium; in vitro fertilisation; Implantation, Embryo
Endometrial thickness and frozen thaw embryo transfer: A prospective study
Mahalakshmi S1, Sakthi A1, Saravanan L1 and Sharma Nidhi2*
1ARC International Fertility Center, 947, Avinashi Road, Puliakulam, Coimbatore-641037, Tamil Nadu, India
2Department of Obstetrics and Gynecology, Saveetha University,Kuthambaakam, Chennai-600124, Tamil Nadu, India
*Address for Correspondence: Sharma Nidhi, ARC International Fertility Center, 947, Avinashi Road, Puliakulam, Coimbatore-641037, Tamil Nadu, India, Tel: +91 9445560392; Email: drbonuramkumar@yahoo.co.in; drbonuramkumar@gmail.com
Aim and objectives: Endometrial Window of Implantation (WOI) is open in the midsecretory phase wherein the markers of invasion and cell adhesion are manifested .The primary objective was to find out the predictive value of Endometrial thickness and profile as a prognostic factors for embryo transfers during ART.
Materials and Methods: Endometrial thickness assessment was performed with grey scale ultrasound on the day of transfer just before thawing the embryos in patients undergoing Frozen embryo transfer cycle after endometrial preparation.
Results: The mean age and standard deviation of study population was is 33.26+5.95.Out of 69 patients there was clinical pregnancy in 33 patients , miscarriage in 10 patients and ongoing pregnacy in 23 patients. So the implantation rate was 47.83% (33/69), early miscarriage rate (pregnancy ending before 12 weeks) was 14.49%(10/69) and the ongoing pregnancy rate was 33.33% (23/69). Endometrial thickness < 6 mm had comparable implantation rates but low ongoing pregnancy rates.
Conclusion: The ultrasound morphological and vascular grading of endometrial thickness and vascularity is useful to synchronise Day 5 embryo transfer and window and implantation thereby minimizing the loss of good embryos in nonreceptive endometrium.
Endometrial Window of Implantation (WOI) is open in the midsecretory phase wherein the markers of invasion and cell adhesion are manifested [1]. The human endometrium has a functional layer and basal layer each consisting of stroma and epitheium [2]. In the functional layer, the epithelium is involved in embryo adhesion and stroma is involved in embryo nurturing [3]. The basal layer epithelium and stroma mainly helps in regeneration [3]. Though several advances have been made in genomics, transcriptomics and the various other interactomes like proteomics and lipidomics of endometrial receptivity, the biophysical markers of endometrial thickness and vascularity are economic and feasible in clinical settings.The classical Noye’s histological grading using the LH peak takes into account the seven characteristic histological attributes of mid secretory endometrium that predict its implant ability [3].
The definition of receptive endometrium that is after 7 days of LH surge and after 5 days of progesterone includes eight histological featues. Epithelial features are the fraction glandular cells in mitosis, the visualization of nuclear pseudostratification, the presence of secreting basal vacuoles. The stromal features are edema, pseudodecidualization, stromal mitosis and leucocyte infiltration. The assessment of receptive endometrium by ultrasound needs to be assessed as compared to this gold standard of window of implantation [4].
Endometrial Receptivity is integral to implantation so identification of an accurate marker of implantation would be highly beneficial in assisted reproductive technology (ART). Despite enormous research in the field of human embryo implantation, the ideal marker of Endometrial Receptivity remains unidentified [5-7].
On ultrasound monitering in IVF cycle the endometrial thickness increases in the follicular phase and endometrial character changes from a hypoechoic trilaminar one to a compact hyperechoic look post ovulation [8]. A tri laminar endometrium on the day of ovulation trigger is associated with an increased probability of pregnancy while a hyperechoic character signals failure [9].
In proliferative endometrium there is cell proliferation and cell differentiation and vascularization in response to estrogen. The secretory phase can be classified as early secretory, midseretory and late secretory [10]. The early secretory endometrium shows increased intracellular transport and cell metabolism. The midsecretory endometrium or the “Window of implantation” shows immune system signaling and intracellular communication and cell adhesion [11,12]. The late secretory endometrium is mostly inflammatory mediators and apoptosis. The first half of the sectretory phase is characterized by expression of soluble ligands and their recetors coded by progesterone related genes. The second half of the secretory phase is characterized by vasoconstriction and inflammatory response. Decidual reaction of endometrium happens soon after the closure of window of implantation and this change does not depend on the presence or absence of blastocyst. The activation of innate and humaral immunity characteristic of decasualization are interpreted as 5 line pattern and zonal vascularisation of endometrium [13-15).This study was done to find the role of endometrial patterns and thickness in predicting and optimizing ART outcome in Frozen Embryo transfer.
This prospective study examined 69 infertile women who underwent embryo replacement from Jan 2019 to Nov 2019 at the ARC Fertility centre, Saveetha Medical College and Hospital. Ethical committee approval and institutional review board approval was obtained (SMC/IEC/2019/11/008). Inclusion criterium was Age group 25-45, two or more blastocyst (grade 3/4) available for replacement and normal uterine cavity in hysteroscopy. Exclusion criteria was presence of endometrial polyp, congenital uterine Anamolies, adenomyosis, endometriosis, hydrosalphinx and fibroid uterus.Written informed consent was obtained from all participants in local language.
The endometrial thickness and pattern was visulised on the day 18 of previous cycle before Frozen Embryo Transfer cycle (Mock cycle). Endometrium was prepared with estrogen started from day 1 of cycle (2 mg/day from cycle days 1 to 4, 4 mg/day from days 5 to 8, and 6 mg/day from days 9 to 12).
Progesterone was added after endometrium reched a thickness of 8 mm to initiate the secretory changes (40 mg intramuscular administration of progesterone was provided and maintained for the following 5 days).
Low dose Aspirin (75 mg once daily) was administrated for improving endometrial receptivity. Day 3 Embryos were thawed and embryo replacement was done on day 4 after 3 days of progesterone administration.
From day 8 of cycle 150 IU of HCG was given intramuscularly to promote endometrial thickness reaches at least 7 mm. HCG has been shown to associated with decasualization process signaling via Vascular Endothelial Growth Factor (VEGF), Leukemia Inhibiting Factor (LIF), Insulin like growth factor like Binding protein 1. It also signals the secretion of Matrix mettaloproteinases from NK cells and secretion of Monocyte Colony Stimulating Factor. HCG also inhibits apoptosis promotes differentiation of stromal cells.
Descriptive and inferential statistics were used to analyse the data. Odd’s ratio was used to analyse categorical variables. Predictive values of Endometrium > 6 mm was calculated for Biochemical pregnancy, Clinical pregnancy and ongoing pregnancy. Statistical Analysis was done using MEDCALC (Belgium).
A total of 69 patients with history of thin endometrium who underwent frozen ET after treatment in ARC Fertility centre, Saveetha Medical College over a period for one year were analyzed in this study. The mean age and standard deviation of study population was is 33.26 + 5.95. Out of 69 patients there was clinical pregnancy in 33 patients , miscarriage in 10 patients and ongoing pregnacy in 23 patients. So the implantation rate was 47.83% (33/69), early miscarriage rate (pregnancy ending before 12 weeks) was 14.49%(10/69) and the ongoing pregnancy rate was 33.33% (23/69).
Table 1a shows the clinical pregnancy (fetal pole and cardiac activity) diagnosed by ultrasound in group 1 and group 2. There were no significant differences in implantation rates in thin and thick endometrium. Table 1b shows the ongoing pregnancy (till second trimester) diagnosed by ultrasound in group 1 and group 2. Table 1b shows that there are fewer ongoing pregnancy in thin endometrium as compared to thick endometrium.This implies that though there are implantations in thin endometrium there are more chances of miscarriage and there is less chance of ongoing pregnancy if endometrium is less than 6 mm.
| Table 1a: Endometrial Thickness and Ultrasound imaging of fetal pole and cardiac activity. | |||
| Characteristic | Clinical Pregnancy | No Pregnancy | Total |
| Endometrium>6mm | 28 | 33 | 61 |
| Endometrium<6 mm | 5 | 3 | 8 |
| Total (n) | 33 | 36 | 69 |
| Table 1b: Endometrial thickness and ongoing pregnancy till second trimester. | |||
| Characteristic | Ongoing Pregnancy | No Pregnancy | Total |
| Endometrium>6mm | 22 | 39 | 61 |
| Endometrium<6mm | 1 | 7 | 8 |
| Total | 23 | 46 | 69 |
Table 2 tells us the sensitivity, (specificity, likelyhood ratio positive and negetive and positive and negetive prognostic value of Endometrium thickness > 6 mm in predicting the ongoing pregnancy rates (Table 2).
| Table 2: Predictive Value Of Endometrial Thickness>6mm For Clinical And Ongoing Pregnancy In Frozen Embryo Transfer Cycles (N = 69).(Logistic regression was used to obtain the Odd’s ratio (OR) and 95% CI. Statistical analysis was done using MEDCALC). | ||||||
| Endometrial Thickness > 6 mm Test Statistic (95% CI) |
Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | LR+ | LR- |
| Clinical Pregnancy | 84.85(68.10-94.89) | 8.33(1.75-22.47) | 45.90(41.61-50.26) | 37.50(13.45-69.85) | 0.93(0.78-1.10) | 1.82(0.47-7.02) |
| Ongoing Pregnancy | 95.65(78.05-99.89) | 15.22(6.34-28.87) | 36.07(32.68-39.60) | 87.50(47.78-98.17) | 1.13(0.97-1.31) | 0.29(0.04-2.19) |
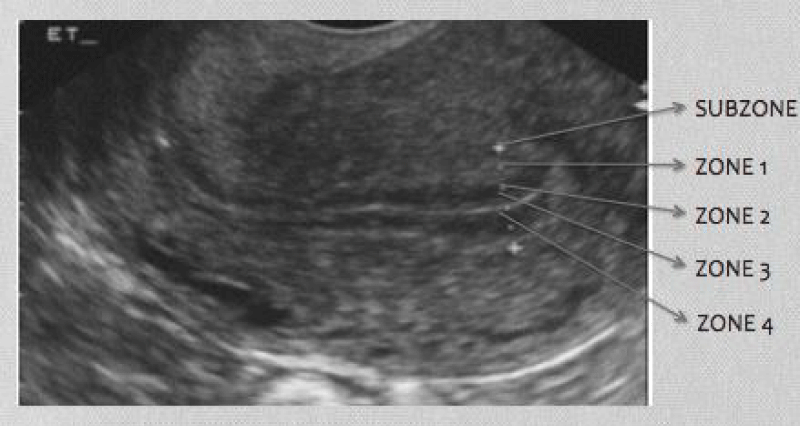
Figure 1: Ultrasound 2 Dimensional Grey scale measurement of Endometrial thickness.
Endometrial thickness assessment is done routinely before embryo transfer and thin endometrium is considered as poor predictor and embryo transfer is deferred. However one must remember that there are isolated case reports of successful implantation in very thin endometriums also [16-18]. In 2 D ultrasound the endometrium is classified as Grade A, B and C. The Grade A endometrium the 5 layered endometrium and the intervenning area between the outer and inner echogenic areas is more echogenic than the surrounding endometrium. In Grade 2 endometrium the intervening is less echogenic than the surrounding endpmetrium. In Grade 3 endometrium the enometrium is homogenously isoechoic. This changes successively represent the rise and release of glycogen containing vacuoles up to the endometrial surface [19].
On Colour Doppler the vascularity can reach to varius zones as characterised by Applebaum’s [20]. The outermost vascularity zone is subzonal vascularity. Blood vessels reaching the 2 mm thick area surrounding the the hyperechoic outer layer of the endometrium. Zone 1 is the outermost myometrial endometrial junction. Zone 2 is the hyperechoic outer endometrium. Zone 3 is the inner hypoechoic endometrium. Zone 4 is the endometrial cavity. The reasons for low implantation could be a high impedance blood flow of the radial arteries leading to poor endometrial glandular growth in thin endometrium. Poor angiogenesis subsequent to decreased VEGF secretion can also affect endometrial vascularity. This in turn increases chances of poor placentation and inappropriate vascularization leading to early abortions even if pregnancy is established. Transfer of embryos to an endometrium prepared by HRT seems to yield better results than fresh embryo transfers [21-23]. The other parameters included assessing uterine biophysical profile for implantation are summerised in table 3.
| Table 3: Uterine Biophysical Profile (Uterine scoring system in Reproduction). | ||
| Parameter | Determination | Score |
| Endometrial Thickness | <7 mm 7-9mm 9-13mm >14mm |
0 2 3 1 |
| Endometrial Layering | No layering Hazy 5 line Distinct 5 line |
0 1 3 |
| Endometrial Motion(No of myometrium contractions in 2 minutes) | <3 >3 |
0 3 |
| Myometrium Echogenicity | Course inhomogeneous Relatively homogenous |
1 2 |
| Uterine artery Doppler Pulsatility Index | >3 2.00-2.99 <2 |
0 1 2 |
Other agents that are used to improve endometrial thickness and vascularity are Filgrastin Intrauterine instillation, Vitamin E, L arginine and sildenfil citrate [24-26].
Since Noyes in 1950’s the endometrium receptivity has been a challenge. Transcriptomics and DNA probes are not full proof as they have probes which carry inbuilt problems of specificity and sensitivity . Decidualizing endometrium can be easily profiled by sonoendocrinology thereby avoiding expensive tests of biochemical hormones and transcriptomics.
The authors are thankful to ARC group of institutions and Saveetha Institute of Medical and Technical sciences for the providing the infrastructure and support for the conduct of study.
- Cha J, Vilella F, Dey SK, Simon C. Molecular interplay in successful implantation in ten crtical topics in reproductive medicine 2013; 44-48.
- Cervello I, Gil-Sancis C, Mas A, Delgado-Rosas F, Martinez-Conjero JA, et al. Human endometrial side population cells exhibit genotypic, phenotypic and functional features of somatic stem cells. PloS One. 2010; 5: e10964. https://pubmed.ncbi.nlm.nih.gov/20585575/
- Gellersen B, Brosens IA, Brosens JJ. Decidualization of human endometrium: mechanisma, functions and clinical perspectives. Semin Reprod Med. 2007; 25: 443-453. https://pubmed.ncbi.nlm.nih.gov/17960529/
- Barker MA, Boehnlein LM, Kovacs P, Lindheim SR. Follicular and luteal phase endometrial thickness and echogenic pattern and pregnancy outcome in oocyte donation cycles. J Assist Reprod Genet. 2009; 26: 243-249. https://pubmed.ncbi.nlm.nih.gov/19548081/
- El-Toukhy T, Coomarasamy A, Khairy M, Sunkara K, Seed P, et al. The relationship between endometrial thickness and outcome of medicated frozen embryo replacement cycles. Fertil Steril. 2008; 89: 832-839. https://pubmed.ncbi.nlm.nih.gov/17681313/
- Kumbak B, Erden HF, Tosun S, Akbas H, Ulug U, et al. Outcome of assisted reproduction treatment in patients with endometrial thickness less than 7 mm. Reprod Biomed Online. 2009; 18: 79-84. https://pubmed.ncbi.nlm.nih.gov/19146773/
- Rinaldi L, Lisi F, Floccari A, Lisi R, Pepe G, Fishel S. Endometrial thickness as a predictor of pregnancy after in-vitro fertilization but not after intracytoplasmic sperm injection. Hum Reprod. 1996; 11: 1538-1541. https://pubmed.ncbi.nlm.nih.gov/8671501/
- Kovacs P, Matyas S, Boda K, Kaali SG. The effect of endometrial thickness on IVF/ICSI outcome. Hum Reprod. 2003; 18: 2337-2341. https://pubmed.ncbi.nlm.nih.gov/14585884/
- Zhang X, Chen CH, Confino E, Barnes R, Milad M, et al. Increased endometrial thickness is associated with improved treatment outcome for selected patients undergoing in vitro fertilization-embryo transfer. Fertil Steril. 2005; 83: 336-340. https://pubmed.ncbi.nlm.nih.gov/15705371/
- Richter KS, Bugge KR, Bromer JG, Levy MJ. Relationship between endometrial thickness and embryo implantation, based on 1,294 cycles of in vitro fertilization with transfer of two blastocyst-stage embryos. Fertil Steril. 2007; 87: 53-59. https://pubmed.ncbi.nlm.nih.gov/17081537/
- Shapiro H, Cowell C, Casper RF. The use of vaginal ultrasound for monitoring endometrial preparation in a donor oocyte program. Fertil Steril. 1993; 59: 1055-1058. https://pubmed.ncbi.nlm.nih.gov/8486173/
- Coulam CB, Bustillo M, Soenksen DM, Britten S. Ultrasonographic predictors of implantation after assisted reproduction. Fertil Steril. 1994; 62: 1004-1010. https://pubmed.ncbi.nlm.nih.gov/7926110/
- Thouas GA, Dominguez F, Green MP, Vilella F, Simon C, Gardener DK. Soluble ligands and their receptors in human enbryo development and implantation. Endocr Rev. 2015; 36: 92-130. https://pubmed.ncbi.nlm.nih.gov/25548832/
- Gingold JA, Lee JA, Rodriguez-Purata J, Whitehouse MC, Sandler B, Grunfeld L, et al. Endometrial pattern, but not endometrial thickness, affects implantation rates in euploid embryo transfers. Fertil Steril. 2015; 104: 620-628.e5. https://pubmed.ncbi.nlm.nih.gov/26079695/
- Bonilla-Musoles F, Raga F, Osborne NG, Castillo JC, Bonilla F Jr. Endometrial receptivity: Evaluation with ultrasound. Ultrasound Q. 2013; 29: 3-20.
- Check JH, Dietterich C, Check ML, Katz Y. Successful delivery despite conception with a maximal endometrial thickness of 4 mm. Clin Exp Obstet Gynecol. 2003; 30: 93-94. https://pubmed.ncbi.nlm.nih.gov/12854850/
- Sundström P. Establishment of a successful pregnancy following in-vitro fertilization with an endometrial thickness of no more than 4 mm. Hum Reprod. 1998; 13: 1550-1552. https://pubmed.ncbi.nlm.nih.gov/9688390/
- Dix E, Check JH. Successful pregnancies following embryo transfer despite very thin late proliferative endometrium. Clin Exp Obstet Gynecol. 2010; 37: 15-16. https://pubmed.ncbi.nlm.nih.gov/20420271/
- Kupesic S, Kurjak A, Bjelos D, et al. Sonographic imaging in infertility. In: Kurjak A, Arenas JB (Eds). Donald school textbook of Transvaginal Ultrasound , First edition. New Delhi, India: Jaypee Brothers and Medical Publishers (P) Ltd; 2005; 357-383.
- Kasius A, Smit JG, Torrance HL, Eijkemans MJ, Mol BW, Opmeer BC, et al. Endometrial thickness and pregnancy rates after IVF: A systematic review and meta-analysis. Hum Reprod Update. 2014; 20: 530-541. https://pubmed.ncbi.nlm.nih.gov/24664156/
- Check JH, Cohen R, Wilson C, Corley D, Dietterich C. Very thin endometria in the late proliferative phase is more associated with poor pregnancy rates following controlled ovarian hyperstimulation than graduated estradiol regimens used for frozen embryo transfer. Fertil Steril. 2014; 101: e21.
- Dain L, Bider D, Levron J, Zinchenko V, Westler S, et al. Thin endometrium in donor oocyte recipients: Enigma or obstacle for implantation? Fertil Steril. 2013; 100: 1289-1295. https://pubmed.ncbi.nlm.nih.gov/23954352/
- Casper RF. Its Time to pay attention to endometrium. Fertil Steril. 2011; 96: 519-521. https://pubmed.ncbi.nlm.nih.gov/21880272/
- Lv H, Li X, Du J, Ling X, Diao F, et al. Effect of endometrial thickness and embryo quality on live-birth rate of fresh IVF/ICSI cycles: a retrospective cohort study. Reprod Biol Endocrinol. 2020; 18: 89. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7441697/
- Huang J, Lin J, Lu X, Gao H, Song N, et al. Association between endometrial thickness and neonatal outcomes in intrauterine insemination cycles: a retrospective analysis of 1,016 live-born singletons. Reprod Biol Endocrinol. 2020; 18: 48. https://pubmed.ncbi.nlm.nih.gov/32410619/
- Hayashi N, Enatsu N, Iwasaki T, Otsuki J, Matsumoto Y, et al. Predictive factors influencing pregnancy rate in frozen embryo transfer. Reprod Med Biol. 2020; 19: 182-188. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7138944/