Exploring the Role of Adult Wrist Circumference as a Potential Indicator of Obesity
By Mozaffer Rahim Hingorjo1, Anisun Nisa2Affiliations
doi: 10.29271/jcpsp.2024.02.135ABSTRACT
Objective: To explore the correlation of wrist circumference (WrC) with various obesity indices and to determine gender-specific optimal cut-off points of WrC for obesity.
Study Design: Cross-sectional study.
Place and Duration of the Study: Dow University of Health Sciences, Karachi, Pakistan, from December 2021 to December 2022.
Methodology: Two hundred and eighty residents of Karachi, aged 30–60 years, participated in this research. Established methods were used to measure body mass index (BMI), waist circumference, hip circumference, neck circumference, WrC, visceral fat level, waist-hip ratio, abdominal volume index, and body roundness index. Correlation of WrC with all obesity markers was done and scatterplots were obtained. Receiver Operating Characteristic curves were plotted to find the gender-specific cut-off value of WrC.
Results: Of the total 280 subjects, 191 (68%) were females and 89 (32%) were males. The overall mean age was 42.04 ± 9.12 years (range: 28-65 years). The mean WrC in males and females were 16.32 ± 1.01 cm and 14.82 ± 1.03 cm, respectively. The WrC correlated best with neck circumference in males (r = 0.758; p<0.001) and BMI in females (r=0.615; p<0.001). The scatterplots obtained showed positive linear relationships between WrC and anthropometric variables. The cut-off values of WrC for adult males and females when compared to waist circumference were 15.45 cm and 13.95 cm, respectively.
Conclusion: Measurement of the WrC can be a helpful indicator to identify excess weight in the general population. Its ease of measurement makes it applicable in both routine clinical practice and extensive epidemiological research.
Key Words: Wrist circumference, BMI, Waist circumference, Obesity.
INTRODUCTION
Obesity is a global epidemic, with Pakistan ranking ninth in obesity rates worldwide.1 Identifying reliable and accessible markers for obesity has become an area of intense research interest. Researchers are exploring wrist circumference (WrC) as a potential indicator of obesity due to its correlation with body fat distribution and overall adiposity, addressing the need for reliable and accessible markers.2
Multiple methods exist to assess body fat accumulation, but consensus on the best method for measuring obesity is lacking. Each method has pros and cons and may be more suitable in specific cases.3 For instance, the body mass index (BMI), a popular indicator, only indicates general obesity and cannot differentiate between fat, muscle, and bone weight.4 Consequently, a bodybuilder and a person with excess fat could have the same BMI.5
In busy clinical settings, accurately measuring waist circumference (WC) in obese individuals becomes challenging due to interference caused by clothing and poor visibility of landmarks. This compromised accuracy is further exacerbated by operator variability, which can impact the results.6 Despite these challenges, WC is still used as a primary criterion in diagnosing disorders like metabolic syndrome.
Multiple studies have investigated the association between WrC and obesity, aiming to determine its usefulness as a proxy measure for body fat content.2 WrC is considered to be an easily measurable anthropometric parameter, and its potential to predict obesity has drawn attention due to its simplicity and non-invasive nature.
Extensive research conducted on a population of Turkish children and young adults unveiled a significant correlation between WrC and body frame size. The findings indicated that WrC could serve as a valuable indicator for assessing obesity and metabolic risk.7 in a systematic review and meta-analysis, an increase in WrC increased the risk for cardiometabolic risk factors.8
Moreover, other research studies have highlighted the potential of WrC in specific populations. For instance, in a recent study conducted in South Indian young people and teens, WrC was identified as an important indicator of obesity, particularly larger WrC being associated with higher risk of metabolic syndrome, a risk factor for cardiovascular disease.9
While WrC shows promise as an indicator for obesity, it should not be employed in isolation for obesity diagnosis. Incorporating it alongside other obesity measures allows for a more comprehensive evaluation of adiposity. Research is needed to set standardised WrC cut-offs and validate its use in diverse populations. Incorporating WrC as an additional tool in obesity assessment can improve accuracy, accessibility, and effectiveness of screening, monitoring, and preventive interventions. The objective of this study was to investigate the relationship of WrC with various obesity indices and to determine gender-specific optimal cut-off points giving healthcare clinicians a useful tool to reliably assess obesity risk.
METHODOLOGY
It was a cross-sectional study conducted at the Physiology Department of Dow Medical College, Dow University of Health Sciences (DUHS) in Karachi, from December 2021 to December 2022. Individuals aged 30 to 60 years were selected from the general population of Karachi using non-probability purposive sampling. To encourage participation, pamphlets were distributed at DUHS, and the chief investigator provided guidance. The study was approved by the DUHS Institutional Review Board (IRB) committee dated on 30 December, 2021 (No. 2238/DUHS/Approval/2021/646). All participants received detailed explanations of the study's goals, procedures, and potential outcomes, and provided written and verbal consent.
The study's sample size of 280 individuals was established using Power Analysis and Sample Size (PASS) software, version 11. This calculation was grounded in a correlation coefficient of 0.239, representing the relationship between WrC and fasting insulin levels.10 The test's parameters included an 80% power and a 95% confidence interval.
Participants who were excluded from the study included pregnant or lactating women, individuals with skeletal deformities or bilateral wrist fractures, bodybuilders or labourers, as well as those with a history of diabetes, chronic liver disease, renal dysfunction, or heart failure.
Trained assistants collected anthropometric measurement data for this study. Weight (kg) was divided by height (m2) to determine BMI. Visceral fat (VF) was measured with bioelectrical impedance analysis, which assessed VF by passing a low electrical current through the body. Muscular individuals exhibited lower impedance due to their higher water content in muscles. The assessment of WC was conducted at the anatomical midpoint of the iliac crest and the very last rib. Hip circumference (HC) was taken around the fullest part of buttocks, just below iliac crest. Waist-hip ratio (WHR) was obtained by dividing WC by HC. Neck circumference (NC) was measured with 0.1 cm (1 mm) precision inferior to thyroid cartilage in the larynx, at right-angle to midline of the neck. These measurements provide valuable insights into body composition and help evaluate health-related risks. WrC was measured with 0.1 cm precision as participants sat with hands facing up. The wrist size was determined with an open hand, measuring the farthest points of the radius and ulna. The superior border was read over the Lister tubercle for accuracy. Abdominal Volume Index (AVI) quantifies abdominal adiposity by calculating the volume between WC and HC, providing a measure of abdominal fat accumulation. It was calculated as AVI = [2WC2 + 0.7(WC – HC)2] / 1000.11
Body Roundness Index (BRI) for predicting central obesity was measured with the equation:
BRI = 364.2−365.5×√1−{[(WC/(2π))2]/[(0.5 × height)2]}.12
Data analysis was performed using SPSS version 21. Descriptive statistics were utilised to summarise subject characteristics in terms of counts and percentages, where required. To explore gender differences, an independent sample t-test was employed. Pearson's correlation coefficients were computed to explore the association between WrC and other markers of obesity. Scatterplots were generated to visualise the relationship between obesity variables. The data were divided into tertiles based on WrC, and a one-way ANOVA was conducted to investigate associations among various anthropometric variables. All statistical tests were considered significant at a threshold of p<0.05. Receiver operating characteristic (ROC) curves were generated to establish the cut-off value for WrC.
RESULTS
The study consisted of 280 participants, with 89 males (making up 32%) and 191 females (constituting 68%) of the total sample. The participants' average age was 42.04 ± 9.12 years. The range for the BMI was from 17.40 to 40.00 kg/m2, with the average being 28.37 ± 5.14 kg/m2. Males were younger than females (38.64 ± 8.22 and 42.83 ± 9.15 years, respectively, p<0.001). However, they were comparable in terms of BMI, HC, and BRI. All other adiposity variables showed significant gender differences (all p-values <0.001). A Pearson correlation coefficient was generated in order to analyse the correlation between WrC and other indices of obesity (Table I). The strongest correlation in men was with NC (r=0.758; p<0.001) and in women, it was with BMI (r=0.615; p<0.001); WC (r=0.604; p<0.001); HC (r=0.606; p<0.001); and NC (r=0.600; p<0.001). In general, correlations with WrC were stronger among women than men.
Figure 1 shows scatterplots between WrC, BMI, and WC in both genders. There was a moderate, positive, linear relationship seen in males between WrC against both BMI (r=0.425; p<0.001) and WC (r = 0.531; p<0.001). In females, the relation was found stronger between WrC against both BMI (r = 0.615; p<0.001) and WC (r = 0.604; p<0.001).
Gender-wise adiposity indices were examined based on Tertiles of WrC (Table II). One-way ANOVA was conducted to compare means among the Tertiles. The findings revealed a significant increase in all obesity indices except for WHR in both genders as WrC Tertiles increased.
Table I: Correlation of wrist circumference with anthropometric indices of obesity.
|
|
Males (89) |
Females (191) |
||
|
Correlation (r) |
p-value |
Correlation (r) |
p-value |
|
|
Body Mass Index (kg/m2) |
0.425 |
<0.001*** |
0.615 |
<0.001*** |
|
Visceral Fat Level |
0.500 |
<0.001*** |
0.524 |
<0.001*** |
|
Waist Circumference (cm) |
0.531 |
<0.001*** |
0.604 |
<0.001*** |
|
Hip Circumference (cm) |
0.310 |
0.003** |
0.606 |
<0.001*** |
|
Waist Hip Ratio |
0.408 |
<0.001*** |
0.234 |
<0.001*** |
|
Neck Circumference (cm) |
0.758 |
<0.001*** |
0.600 |
<0.001*** |
|
Abdominal Volume Index |
0.510 |
<0.001*** |
0.587 |
<0.001*** |
|
Body Roundness Index |
0.385 |
<0.001*** |
0.449 |
<0.001*** |
|
Note: Pearson’s Correlation (r) between wrist circumference and other anthropometric variables. *p<0.05; **p<0.01; ***p<0.001. |
||||
Table II: Anthropometric Indices of males and females across Tertiles of wrist circumference.
|
Males |
||||
|
|
Tertile 1 (<16.1 cm) |
Tertile 2 (16.1-16.8 cm) |
Tertile 3 (>16.8 cm) |
p for trend |
|
WrC (cm) |
15.38±0.61 |
16.44±0.20 |
17.31±0.79 |
<0.001*** |
|
BMI (kg/m2) |
26.08±3.63 |
27.76±4.32 |
31.09±4.50 |
<0.001*** |
|
VF level |
9.91±3.62 |
11.23±4.18 |
14.93±4.19 |
<0.001*** |
|
WC (cm) |
94.21±8.43 |
97.92±9.60 |
106.19±9.88 |
<0.001*** |
|
HC (cm) |
102.11±8.36 |
103.02±8.81 |
108.75±7.18 |
0.004** |
|
WHR |
0.92±0.07 |
0.95±0.05 |
0.97±0.05 |
0.008** |
|
NC (cm) |
35.75±2.24 |
37.46±1.80 |
39.31±2.80 |
<0.001*** |
|
AVI |
18.48±2.60 |
19.38±3.87 |
22.87±3.99 |
<0.001*** |
|
BRI |
4.95±1.17 |
5.10±1.30 |
6.27±1.63 |
0.001** |
|
Females |
||||
|
|
Tertile 1 (<14.1 cm) |
Tertile 2 (14.1-15.4 cm) |
Tertile 3 (>15.4 cm) |
p for trend |
|
WrC (cm) |
13.67±0.47 |
14.76±0.31 |
15.96±0.50 |
<0.001*** |
|
BMI (kg/m2) |
24.55±3.92 |
28.58±4.04 |
31.94±4.71 |
<0.001*** |
|
VF level |
6.58±2.25 |
8.51±2.21 |
9.43±1.75 |
<0.001*** |
|
WC (cm) |
83.84±11.53 |
93.99±9.34 |
101.43±10.38 |
<0.001*** |
|
HC (cm) |
96.76±8.87 |
105.91±8.00 |
111.68±9.45 |
<0.001*** |
|
WHR |
0.86±0.07 |
0.89±0.08 |
0.91±0.07 |
<0.001*** |
|
NC (cm) |
30.93±1.96 |
32.33±1.89 |
34.29±1.73 |
<0.001*** |
|
AVI |
15.50±3.43 |
18.48±2.86 |
21.19±3.79 |
<0.001*** |
|
BRI |
4.85±1.50 |
5.78±1.25 |
6.57±1.55 |
<0.001*** |
|
Note: One-way ANOVA to compare means between Tertiles. Variables are represented as mean±SD. *p<0.05, significant; **p<0.01, very significant; ***p<0.001, extremely significant. Abbreviations: WrC, Wrist circumference; BMI, Body mass index; VF, Visceral fat level; WC, Waist circumference; HC, Hip circumference; WHR, Waist-hip ratio; NC, Neck circumference; AVI, Abdominal volume index; BRI, Body roundness index. |
||||
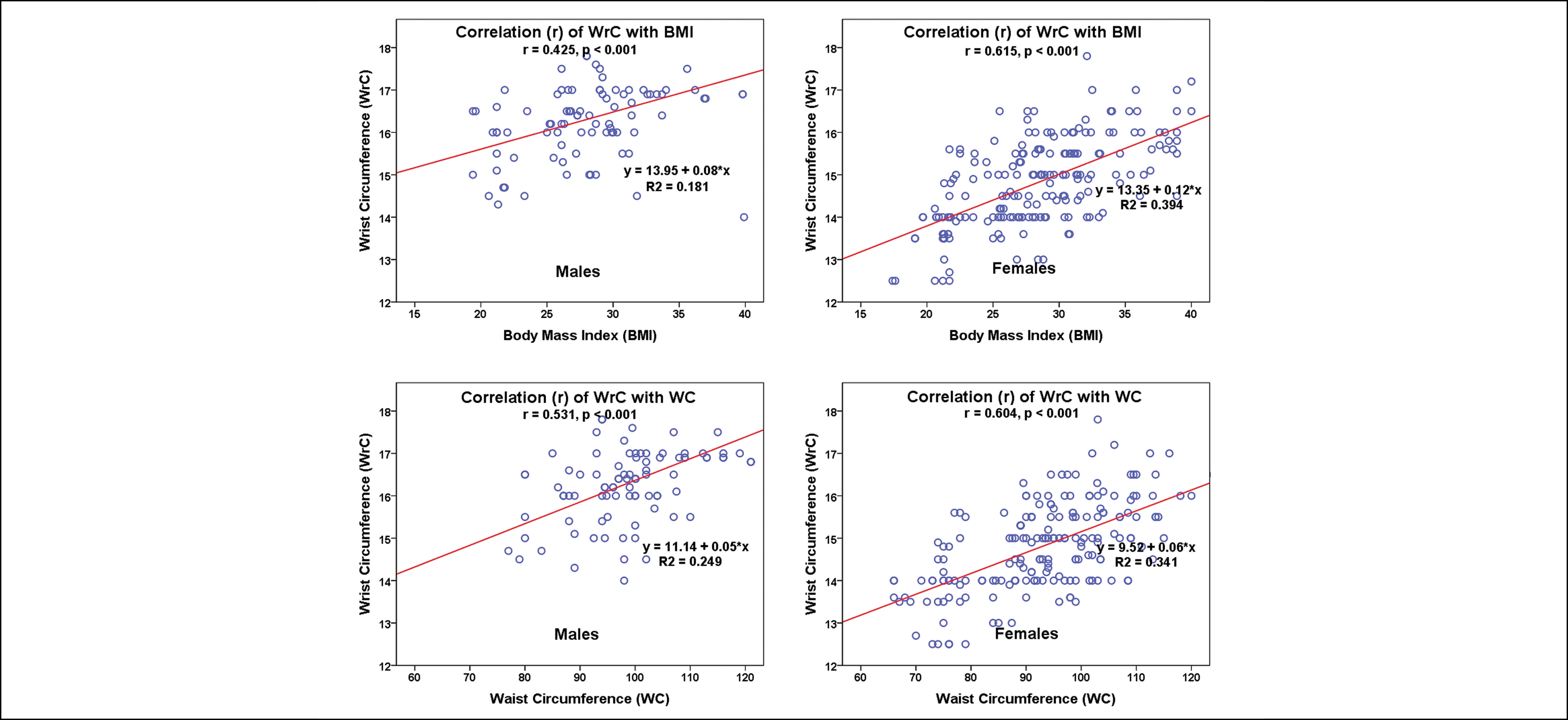 Figure 1: Scatter plot showing correlation (r) of wrist circumference (WrC; cm) with Body Mass Index (BMI: kg/m2) and waist circumference (WC; cm) in male and female subjects.
Figure 1: Scatter plot showing correlation (r) of wrist circumference (WrC; cm) with Body Mass Index (BMI: kg/m2) and waist circumference (WC; cm) in male and female subjects.
The ROC curve was analysed for both BMI and WC to assess the sensitivity and specificity of WrC as an important marker for obesity. The ROC curve demonstrated a high level of AUC equal to 0.757 in men, while in women, it was above 0.829 indicating a superior accuracy in distinguishing obesity and the potential clinical utility of WrC as an index of obesity. The cut-off points of WrC versus BMI among males and females were 16.05 cm and 14.45 cm, respectively. Similarly, the cut-off points of WrC versus WC among males and females were 15.45 cm and 13.95 cm, respectively.
DISCUSSION
The use of WrC as a marker of obesity has been a subject of interest and debate in recent research. In this study, the association between WrC and various obesity indices was examined to determine its validity and potential as a practical measurement tool. This study has made marked contribution to the existing body of knowledge, as a research was conducted within the general population of Karachi.
The research revealed a substantial frequency of adiposity, with 82.0% of males and 79.6% of females falling into the overweight or obese category, defined by a BMI of 23 kg/m² or higher. This observation underscored the widespread presence of a significant contributor to non-communicable diseases within this population.
The use of WrC as a measurement for assessing obesity is an emerging area of research and clinical practice. Traditionally, BMI, WC, and other anthropometric measurements have been widely used to determine obesity levels. However, recent studies have suggested that WrC may provide additional insights into body composition and health. In this research, notable positive correlation was observed between WrC and the majority of obesity indices.
According to an Indian study, WrC measurement complements obesity assessment in resource-constrained settings, providing insights into generalised and abdominal obesity and indirectly assessing insulin-resistance.10 It serves as a practical alternative when BMI or accurate WC measurement is challenging.13 An extensive long-term study with a follow-up time of 8.8 years found that WrC is a valid marker for metabolic syndrome and diabetes mellitus among 6393 adult volunteers. Regardless of BMI, this study found that a woman's WrC was an accurate identifier of both subcutaneous and visceral fat.14 In another study conducted on the lifestyle behaviour of children and anthropometric indices, it was observed that WrC was more significant than BMI and WC in certain aspects.15
The WrC is an emerging anthropometric measure that reflects skeletal frame size and may provide valuable information about an individual's body composition and health risks. Studies have shown that WrC is associated with bone mineral density and risk of fracture,16 cardiovascular risk factors,17 and metabolic syndrome.8 Wrist bone mineral density measurement holds diagnostic potential for identifying osteoporosis in post-menopausal women.18 Recent scholarly publication shed light on the recognition of the skeletal system as an emerging endocrine organ. It has become evident that bones play a significant role in the metabolism of glucose by influencing insulin levels through the hormone osteocalcin. Produced by osteoblasts, osteocalcin improves insulin sensitivity, thereby contributing to the regulation of glucose balance through endocrine pathways. Studies have established a connection between insulin-resistance and compensatory hyperinsulinaemia, leading to an increase in bone mass. Interestingly, the measurement of wrist circumference offers a simple means to identify this relationship.19
WrC alone does not directly indicate health status or risk of diseases. However, larger WrC may be associated with a higher risk of certain conditions, such as cardiovascular disease or diabetes, when considered in conjunction with other factors.20
Recent research suggested that NC and WrC indicate upper body fat distribution and can identify overweight or obese patients.21 Over the past decade, multiple studies have shown that NC is a better indicator of VF and insulin-resistance than other anthropometric parameters.22,23 In this study, WrC correlated best with NC for men and BMI, WC, HC, and NC for women.
The range of WrC that best-identified individuals at an elevated risk for cardiometabolic conditions was found to be 17.5-17.8 cm for men and 16.0-16.7 cm for women in Ghanaian subjects.20 An Indian study suggested cut-offs of 15.1 cm for males and 13.9 cm for females at 18 years and above.24 Ethnic disparities and the selection of obese participants may explain variations in cut-off values. In the 10-19-year age group, in a Pakistani research, the average WrC was 14.45 cm for males and 13.81 cm for females, closer to the findings of the current study.25 In this study, adult cut-offs were lower when compared to WC than when compared to BMI, especially in males. As upper body obesity is defined to encompass abdominal obesity and includes WrC, NC, and WC, a cut-off value based on WC rather than BMI would be preferable.
This study's limitations included a small sample size, the impact of genetic, cultural, and behavioural factors on generalisability, incomplete analysis of cardiometabolic risks tied to WrC, and the absence of consideration for potential confounding variables like physical activity, diet, and medical conditions.
CONCLUSION
Measurement of WrC has emerged as a promising and predictive tool due to its strong associations with WC, BMI, obesity, and cardiometabolic markers. The establishment of ethnic-specific thresholds for WrC would benefit from further cohort studies. While WrC measurement holds significance, its utility should be considered in conjunction with other factors such as body fat levels, muscle mass, fat distribution, BMI, and WC to provide a comprehensive assessment of obesity risk.
DISCLOSURE:
The content of this article originated from the Physiology Thesis of Dr. Anis-Un-Nisa, an MPhil Scholar.
ETHICAL APPROVAL:
The study received ethical approval from the Institutional Review Board IRB committee of Dow University of Health Sciences, Karachi (IRB # 2238/DUHS/Approval/2021/646, dated 30 December 2021).
COMPETING INTEREST:
The authors did not declare any conflict of interest.
PATIENTS’ CONSENT:
Written informed consents were taken from all the patients participating in this study.
AUTHORS’ CONTRIBUTION:
MRH: Statistical analysis and interpretation of data, drafting the work, and revising it critically for important intellectual content.
AN: Data collection, significant contribution to the manuscript write-up.
All authors approved the final version of the manuscript to be published.
REFERENCES
- Siddiqui M, Hameed R, Nadeem M, Mohammad T, Simbak N, Latif A, et al. Obesity in Pakistan: Current and future perceptions. Curr Trends Biomed Eng & Biosci 2018; 17(2):55958. doi: 10.19080/CTBEB.2018.17.555958.
- Shafiee G, Qorbani M, Heshmat R, Djalalinia S, Motlagh ME, Arefirad T, et al. Wrist circumference as a novel predictor of obesity in children and adolescents: the CASPIAN-IV study. J Pediatr Endocrinol Metab 2018; 31(7):717-25. doi: 10.1515/ jpem-2017-0206.
- Jayawardena R, Ranasinghe P, Ranathunga T, Mathangasinghe Y, Wasalathanththri S, Hills AP. Novel anthropometric parameters to define obesity and obesity-related disease in adults: A systematic review. Nutrition Reviews 2020; 78(6): 498-513.
- Gurunathan U, Myles PS. Limitations of body mass index as an obesity measure of perioperative risk. Br J Anaesth 2016; 116(3):319-21. doi: 10.1093/bja/aev541.
- Tafeit E, Cvirn G, Lamprecht M, Hohensinn M, Moeller R, Hamlin M, et al. Using body mass index ignores the intensive training of elite special force personnel. Exp Biol Med 2019; 244(11):873-9. doi: 10.1177/1535370219848986.
- Sebo P, Herrmann FR, Haller DM. Accuracy of anthropometric measurements by general practitioners in overweight and obese patients. BMC Obes 2017; 4(1):23. doi: 10.1186/s40608-017-0158-0.
- Ozturk A, Cicek B, Mazıcıoğlu MM, Zararsız G, Kurtoglu S. Wrist circumference and frame size percentiles in 6-17-year-old Turkish children and adolescents in Kayseri. J Clin Res Pediatr Endocrinol 2017; 9(4):329. doi: 10.4274/jcrpe. 4265.
- Namazi N, Djalalinia S, Mahdavi-Gorabi A, Asayesh H, Mansourian M, Noroozi M, et al. Association of wrist circumference with cardio-metabolic risk factors: a systematic review and meta-analysis. Eat Weight Disord-St 2020; 25:151-61. doi:10.1007/s40519-018-0534-x.
- Ahilan V, Krishna VG, Prasad HK, Narayanasamy K, Krishnamoorthy N. Utility of wrist circumference in recognition of metabolic syndrome in overweight and obese South Indian children and adolescents. J Pediatr Endocrinol Metab 2022; 35(1):65-71. doi: 10.1515/jpem-2021-0376.
- Tatar BT, Ersoy C, Kacan T, Kirhan E, Sarandol E, Sigirli D, et al. Neck and wrist circumferences propose a reliable approach to qualify obesity and insulin resistance. Med Sci 2014; 3(1):1013-25. doi: 10.5455/medscience.2013.02. 8100.
- Hu X, Appleton AA, Ou Y, Zhang Y, Cai A, Zhou Y, et al. Abdominal volume index trajectories and risk of diabetes mellitus: Results from the China Health and Nutrition Survey. J Diabetes Investig 2022; 13(5):868-77. doi: 10. 1111/jdi.13733.
- Xu J, Zhang L, Wu Q, Zhou Y, Jin Z, Li Z, et al. Body roundness index is a superior indicator to associate with the cardio‐metabolic risk: Evidence from a cross‐sectional study with 17,000 Eastern-China adults. BMC Cardiovasc Disord 2021; 21(1):1-2. doi: 10.1186/s12872-021-01905-x.
- Ajithkumar PV, Manju L, Deepa M. Correlation of wrist circumference with waist circumference and body mass index in adults with early-onset type 2 diabetes mellitus. Int J Res Med Sci 2019; 7(9):3322-8. doi: 10.18203/ 2320-6012.ijrms20193908.
- Jahangiri Noudeh Y, Hadaegh F, Vatankhah N, Momenan AA, Saadat N, Khalili D, et al. Wrist circumference as a novel predictor of diabetes and prediabetes: results of cross-sectional and 8.8-year follow-up studies. J Clin Endocrinol Metab 2013; 98(2):777-84. doi: 10.1210/jc. 2012-2416.
- Puia A, Leucuta DC. Childrens lifestyle behaviors in relation to anthropometric indices: A family practice study. Clujul Med 2017; 90(4):385. doi: 10.15386/cjmed-758.
- Tamehri Zadeh SS, Moazzeni SS, Asgari S, Mirbolouk M, Azizi F, Hadaegh F. Association between wrist circumference and risk of any fracture in adults: Findings from 15 years of follow-up in the Tehran lipid and glucose study. J Clin Med 2022; 11(23):7048. doi: 10.3390/jcm11237048.
- Li Y, Liu Y, He J, Ma P, Yu L, Sun G. The association of wrist circumference with hypertension in northeastern Chinese residents in comparison with other anthropometric obesity indices. Peer J 2019; 7:e7599. doi: 10.7717/peerj.7599.
- Eftekhar-Sadat B, Ghavami M, Toopchizadeh V, Ghahvechi Akbari M. Wrist bone mineral density utility in diagnosing hip osteoporosis in postmenopausal women. Ther Adv Endocrinol Metab 2016; 7(5-6):207-11. doi: 10.1177/20420 18816658164.
- Amisi CA, Ciccozzi M, Pozzilli P. Wrist circumference: A new marker for insulin resistance in African women with polycystic ovary syndrome. World J Diabetes 2020; 11(2):42-51. doi: 10.4239/wjd.v11.i2.42.
- Obirikorang C, Obirikorang Y, Acheampong E, Anto EO, Toboh E, Asamoah EA, et al. Association of wrist circumference and waist-to-height ratio with cardiometabolic risk factors among type II diabetics in a Ghanaian population. J Diabetes Res 2018; 2018. doi: 10.1155/2018/1838162.
- Karki BB, Bhattarai MD, Bajracharya MR, Karki S, Devkota AR. Correlation of neck and wrist circumference with waist circumference. J Adv Intern Med 2014; 3(6):47-51. doi: 10.3126/jaim.v3i2.14063.
- Scovronec A, Provencher A, Iceta S, Pelletier M, Leblanc V, Nadeau M, et al. Neck circumference is a better correlate of insulin resistance markers than other standard anthropometric indices in patients presenting severe obesity. Obes Res Clin Pract 2022; 16(4):307-13. doi: 10.1016/j.orcp. 2022.07.005.
- Anothaisintawee T, Sansanayudh N, Thamakaison S, Lertrattananon D, Thakkinstian A. Neck circumference as an anthropometric indicator of central obesity in patients with prediabetes: a cross-sectional study. Bio Med Res Int 2019; 2019:4808541. doi: 10.1155/2019/4808541.
- Khadilkar V, Chiplonkar S, Ekbote V, Kajale N, Mandlik R, Khadilkar A. Reference centile curves for wrist circumference for Indian children aged 3–18 years. J Pediatr Endo-crinol Metab 2018; 31(2):185-90. doi: 10.1515/jpem- 2017-0161.
- Asif M, Aslam M, Qasim M, Altaf S, Ismail A, Ali H. A dataset about anthropometric measurements of the Pakistani children and adolescents using a cross-sectional multi-ethnic anthropometric survey. Data Br 2021; 34:106642. doi: 10.1016/j.dib.2020.106642.