- Department of Neurosurgery, Tokyo Women’s Medical University, Shinjuku, Tokyo,
- Department of Spinal Surgery, Kameda Medical Center, Kamogawa, Chiba, Japan.
Correspondence Address:
Isamu Miura, Department of Neurosurgery, Tokyo Women’s Medical University, Shinjuku, Tokyo, Japan.
DOI:10.25259/SNI_870_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Isamu Miura1, Kubota Motoo2, Takakazu Kawamata1, Masahito Yuzurihara2. C6 nerve root palsy after double-door cervical laminoplasty. 06-Oct-2021;12:502
How to cite this URL: Isamu Miura1, Kubota Motoo2, Takakazu Kawamata1, Masahito Yuzurihara2. C6 nerve root palsy after double-door cervical laminoplasty. 06-Oct-2021;12:502. Available from: https://surgicalneurologyint.com/surgicalint-articles/11158/
Abstract
Background: This study correlated the relationship between postoperative C6 nerve root palsies and various patient-related clinical, radiographic, and surgical parameters.
Methods: The medical records of 318 patients undergoing double-door cervical laminoplasty for myelopathy were reviewed. Twelve (3.8%) had postoperative C6 nerve root palsies. Their clinical, radiographic, and surgical procedures were analyzed looking for a correlation/explanation for these new C6 root deficits.
Results: The following factors correlated with patients’ developing new postoperative C6 nerve root deficit following double-door cervical laminoplasty; a high correlation with additional C5 palsies, narrower C6 intervertebral foraminal widths, greater anterior protrusions of the C6 articular process, and larger posterior shifts of the spinal cord on magnetic resonance (MR) between the C4/C5-C6/C7 levels.
Conclusion: Factors correlating with the new onset of C6 nerve root palsies following double-door cervical laminoplasty included; a high correlation with new C5 palsies, more severe foraminal stenosis, greater anterior protrusions of the C6 articular process, and more extensive dorsal spinal cord migration.
Keywords: C5 palsy, C6 nerve root palsy, Double-door laminoplasty, Foraminal stenosis, Postoperative complication
INTRODUCTION
Studies focusing on the new onset of C6 root palsies following posterior cervical decompression are rare.[
MATERIALS AND METHODS
Clinical presentation
We retrospectively reviewed the records of 318 consecutive patients undergoing double-door cervical laminoplasty (i.e. with sagittal splitting of the spinal process without foraminotomies) [
Definition of C6 nerve root palsy
In our study, C6 nerve root palsy was defined by a loss of motor and/or sensory function in the C6 distribution within 2 weeks of surgery/laminoplasty. We additionally compared the C6 palsy group with 40 control patients selected randomly from among the 306 patients without C6 palsy.
Radiological evaluation
Patients in both groups underwent preoperative plain radiography, computed tomography (CT), and magnetic resonance imaging (MRI). Postoperative CT’s were performed on the day of or within days of the surgery, while postoperative MRI’s were performed on postoperative day 7 [
Figure 3:
Measurement of the gutter position by drawing two vertical lines on postoperative computed tomography images, one at the most lateral point of the spinal canal (dotted line), and the other at the most medial position of the gutter (white line). The gutter position is defined as the distance between these two lines. If the gutter line is medial to the canal line, the distance is expressed as a negative number.
Figure 4:
Posterior shift of the spinal cord at the C3/C4, C4/C5, C5/ C6, and C6/C7 levels, measured from the posterior compressive mass to the preoperative and postoperative midpoints of the spinal cord on T2-weighted midsagittal magnetic resonance images. For measurement of the spinal cord shift, the preoperative values are subtracted from the postoperative values (a and b). Representative image of the high-intensity area in the spinal cord on the preoperative T2-weighted images (c).
Statistics
Statistical analysis was performed using the R statistical software. Results are reported as mean ± standard deviation. The Student t-test, Pearson Chi-square test, and Fisher exact test were used, as appropriate. Any P < 0.05 was considered significant. Approval was obtained from the institutional review board of Kameda Medical Center.
RESULTS
Incidence of postoperative C6 palsy
Twelve (3.8%) patients developed unilateral new postoperative C6 nerve root deficits occurring an average of 2.0 ± 1.3 days (0–5 days) postoperatively. Deficits included: 5 with paresis alone, 4 with isolated C6 sensory loss, and 3 with both paresis and sensory deficit. All 12 patients were managed without, additional surgery, and paresis improved at 6 postoperative months in 7 of 8 patients. Notably, seven patients with C6 nerve root palsies also had C5 palsies (58%). A prevalence was significantly higher than in the control group (P < 0.001) [
Radiographic data for the 12 patients with C6 palsies
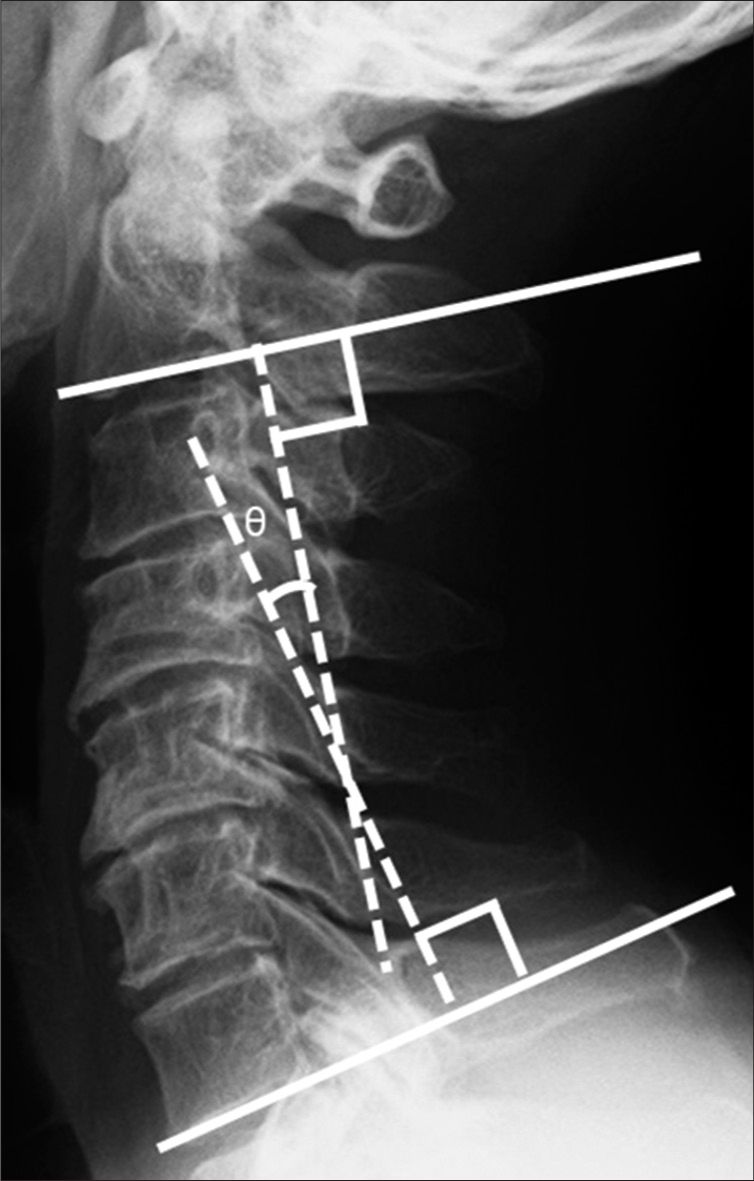
The 12 patients with C6 nerve root palsies showed no significant differences in their C2–C7 lordotic angle (θ) on the plane radiographs, but their CT studies demonstrated significantly narrower C6 intervertebral foramina versus those without C6 palsies [
On the MRI scans, the mean spinal cord shift from C4/C5 to C6/C7 was larger for those with new C6 palsies versus controls, but there were not significant differences in the rate of high cord signals on the preoperative T2-weighted images between the groups (58% vs. 73%, P = 0.351).
DISCUSSION
Several factors are thought to predisposing patients to new C6 palsies following cervical surgery, including laminoplasty. Several studies have suggested that foraminal stenosis is associated with C5 palsies, and here, in our study, we found significantly narrowed C6 intervertebral foramen for those with C6 palsies.[
Ossification of the posterior longitudinal ligament is also thought to be a risk factor for postoperative C5 and C6 nerve root palsies, but in our series, this difference did not reach statistical significance.[
CONCLUSION
Patients experiencing the new onset of a C6 root palsy following a cervical laminoplasty demonstrated: a higher rate of accompanying C5 palsies, greater C6 intervertebral foraminal stenosis, more significant greater anterior protrusion of the C6 articular processes, and more MR-demonstrated extensive dorsal shift of the spinal cord into the laminoplasty defect.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chiba K, Toyama Y, Matsumoto M, Maruiwa H, Watanabe M, Hirabayashi K. Segmental motor paralysis after expansive open-door laminoplasty. Spine (Phila Pa 1976). 2002. 27: 2108-15
2. Hasegawa K, Homma T, Chiba Y. Upper extremity palsy following cervical decompression surgery results from a transient spinal cord lesion. Spine (Phila Pa 1976). 2007. 32: E197-202
3. Hatta Y, Shiraishi T, Hase H, Yato Y, Ueda S, Mikami Y. Is posterior spinal cord shifting by extensive posterior decompression clinically significant for multisegmental cervical spondylotic myelopathy?. Spine (Phila Pa 1976). 2005. 30: 2414-9
4. Ko S, Choi W, Lee J. The prevalence of cervical foraminal stenosis on computed tomography of a selected community-based Korean population. Clin Orthop Surg. 2018. 10: 433-8
5. Liu G, Reyes MR, Riew KD. Why does C5 palsy occur after prophylactic bilateral C4-5 foraminotomy in open-door cervical laminoplasty? A risk factor analysis. Global Spine J. 2017. 7: 696-702
6. Nagoshi N, Yoshii T, Egawa S, Sakai K, Kusano K, Nakagawa Y.editors. Comparison of surgical outcomes after open-and double-door laminoplasties for patients with cervical ossification of the posterior longitudinal ligament: A prospective multicenter study. Spine (Phila Pa 1976). 2021. p.
7. Oya J, Burke JF, Vogel T, Tay B, Chou D, Mummaneni P. The accuracy of multimodality intraoperative neuromonitoring to predict postoperative neurologic deficits following cervical laminoplasty. World Neurosurg. 2017. 106: 17-25
8. Yoshioka N, Takayama M, Kobayashi T, Murai N, Ioroi Y. Neurological disturbance of the upper extremities after cervical laminoplasty: A morphological assessment focused on the intervertebral foramen. Spine (Phila Pa 1976). 2020. 45: E1549-55