Abstract
The aim of this review is to present the clinical data on the efficacy and safety of cilomilast in patients with chronic obstructive pulmonary disease (COPD). Over 6000 COPD patients received cilomilast during an extensive clinical development programme performed by GlaxoSmithKline (GSK).
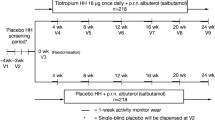
Five phase III randomized, double-blind, placebo-controlled, parallel-group pivotal studies were conducted in poorly reversible patients (<15% or <200 mL improvement over baseline in forced expiratory volume in 1 second (FEV1) after salbutamol). Patients were randomized to receive oral cilomilast 15 mg (n = 2088) or placebo (n = 1408) twice daily for 24 weeks. The co-primary efficacy variables were changes from baseline in trough (predose) FEV1 and in total score of the St George’s Respiratory Questionnaire (SGRQ).
Additional studies were performed to investigate the anti-inflammatory actions of cilomilast by measuring inflammatory cells and mediators in biopsies and induced sputum; to assess the long-term effects of cilomilast; to assess the cardiac safety of cilomilast; and to assess the efficacy of cilomilast on hyperinflation. Results from one of the phase III and from one supportive study have been previously published.
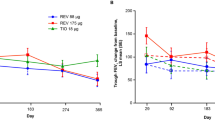
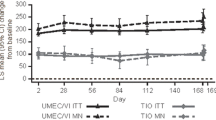
In the phase III pivotal studies, when averaged over 24 weeks, the mean change from baseline in FEV1 in the cilomilast group showed improvement compared with placebo in all studies (range 24–44 mL treatment difference). When averaged over 24 weeks, there was a similar improvement in the mean total SGRQ score in both treatment groups with a decrease ranging from −1.8 to −4.2 units in the cilomilast group and 0.4 to −4.9 units in the placebo group. Only one study, however, showed both a statistically and clinically meaningful difference between the two treatment groups (treatment difference −4.1 units; p < 0.001). Although cilomilast was shown to reduce COPD exacerbations in some of these studies, there was no effect on the incidence of COPD exacerbations in a study specifically powered to detect a difference compared with placebo.
No significant change was found in the primary endpoints of the anti-inflammatory studies, although some anti-inflammatory activity was detected, including a reduction in tissue CD8+ T lymphocytes and CD68+ macrophages in airway biopsies. In addition, studies did not demonstrate a consistent significant effect of cilomilast on hyperinflation.
In all studies, adverse events associated with the gastrointestinal body system were reported more frequently in the cilomilast group than the placebo group and predominantly occurred within the first 2 weeks of initiating cilomilast therapy.
During the cilomilast development programme a number of different endpoints were investigated to characterize the efficacy and safety of this second-generation phosphodiesterase 4 inhibitor. Safety assessments throughout the late-phase programme did not reveal any evidence of serious safety concerns with the use of cilomilast. Previous studies in phase II and early phase III had shown improvements in efficacy endpoints and some evidence of an anti-inflammatory mechanism of action. However, subsequent phase III studies failed to definitively confirm the earlier programme results, which led to termination of the development of cilomilast.

















































Similar content being viewed by others
References
Gamble E, Grootendorst DC, Brightling CE, et al. Antiinflammatory effects of the phosphodiesterase-4 inhibitor cilomilast (Ariflo) in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2003; 168: 976–82
Rennard SI, Schachter N, Strek M, et al. Cilomilast for COPD: results of a 6-month, placebo-controlled study of a potent, selective inhibitor of phosphodiesterase 4. Chest 2006; 129: 56–66
Rabe KF, Hurd S, Anzueto A, et al. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2007; 176: 532–55
Hogg JC. Pathophysiology of airflow limitation in chronic obstructive pulmonary disease. Lancet 2004; 364: 709–21
Hogg JC, Chu F, Utokaparch S, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med 2004; 350: 2645–53
Barnes PJ. Mechanisms in COPD: differences from asthma. Chest 2000; 117 Suppl. 2: 10S–4S
Sutherland ER, Martin RJ. Airway inflammation in chronic obstructive pulmonary disease: comparisons with asthma. J Allergy Clin Immunol 2003; 112: 819–27
Turato G, Zuin R, Miniati M, et al. Airway inflammation in severe chronic obstructive pulmonary disease: relationship with lung function and radiologic emphysema. Am J Respir Crit Care Med 2002; 166: 105–10
Di Stefano A, Capelli A, Lusuardi M, et al. Severity of airflow limitation is associated with severity of airway inflammation in smokers. Am J Respir Crit Care Med 1998; 158: 1277–85
O’Shaughnessy TC, Ansari TW, Barnes NC, et al. Inflammation in bronchial biopsies of subjects with chronic bronchitis: inverse relationship of CD8+ T lymphocytes with FEV 1. Am J Respir Crit Care Med 1997; 155: 852–7
Jeffery PK. Investigation and assessment of airway and lung inflammation: we now have the tools, what are the questions? Eur Respir J 1998; 11: 524–8
Daffern PJ, Jagels MA, Hugli TF. Multiple epithelial cell-derived factors enhance neutrophil survival. Regulation by glucocorticoids and tumour necrosis factor-alpha. Am J Respir Cell Mol Biol 1999; 21: 259–67
Cox G. Glucocorticoid treatment inhibits apoptosis in human neutrophils. J Immunol 1995; 154: 4719–25
Kroegel C, Foerster M. Phosphodiesterase-4 inhibitors as a novel approach for the treatment of respiratory disease: cilomilast. Expert Opin Investig Drugs 2007; 16(1): 109–24
Torphy TJ, Undem BJ. Phosphodiesterase inhibitors: new opportunities for the treatment of asthma. Thorax 1991; 46: 512–23
Sutherland EW, Rall TW. Fractionation and characterization of a cyclic adenine ribonucleotide formed by tissue particles. J Biol Chem 1958; 232: 1077–91
Essayan DM. Cyclic nucleotide phosphodiesterases. J Allergy Clin Immunol 2001; 108: 671–80
Maurice DH, Palmer D, Tilley DG, et al. Cyclic nucleotide phosphodiesterase activity, expression, and targeting in cells of the cardiovascular system. Mol Pharmacol 2003; 64: 533–46
Torphy TJ, Livi GP. Phosphodiesterase isozymes in airways. In: Lenfant C, editor. Lung biology in health and disease. In: Chung KF, Barnes PJ, series editors. Pharmacology of the respiratory tract: clinical and experimental. New York (NY): Marcel Dekker, 1993: 177–221
Torphy TJ, Barnette MS, Underwood DC, et al. Ariflo (SB 207499), a second generation phosphodiesterase 4 inhibitor for the treatment of asthma and COPD: from concept to clinic. Pulm Pharmacol Ther 1999; 12: 131–5
Keatings VM, Collins PD, Scott DM, et al. Differences in interleukin-8 and tumor necrosis factor-alpha in induced sputum from patients with chronic obstructive pulmonary disease or asthma. Am J Respir Crit Care Med 1996; 153: 530–4
Vlahos R, Bozinovski S, Hamilton JA, et al. Therapeutic potential of treating chronic obstructive pulmonary disease (COPD) by neutralising granulocyte macrophage-colony stimulating factor (GM-CSF). Pharmacol Ther 2006; 112(1): 106–15
Barnes PJ. Theophylline for COPD. Thorax 2006; 61: 742–4
Griswold DE, Webb EF, Breton J, et al. Effect of selective phosphodiesterase type IV inhibitor, rolipram, on fluid and cellular phases of inflammatory response. Inflammation 1993; 17: 333–44
Prabhakar U, Lipshutz D, Bartus JO, et al. Characterization of cAMP-dependent inhibition of LPS-induced TNF alpha production by rolipram, a specific phosphodiesterase IV (PDEIV) inhibitor. Int J Immunopharmacol 1994; 16: 805–16
Underwood DC, Kotzer CJ, Bochnowicz S, et al. Comparison of phosphodiesterase III, IV and dual III/IV inhibitors on bronchospasm and pulmonary eosinophil influx in guinea pigs. J Pharmacol Exp Ther 1994; 270: 250–9
Kohyama T, Liu X, Wen FQ, et al. PDE4 inhibitors attenuate fibroblast chemotaxis and contraction of native collagen gels. Am J Respir Cell Mol Biol 2002; 26: 694–701
Barnette MS, Christensen SB, Essayan DM, et al. SB 207499 (Ariflo), a potent and selective second-generation phosphodi-esterase4 inhibitor: in vitro anti-inflammatory actions. J Pharmacol Exp Ther 1998; 284: 420–6
Profita M, Chiappara G, Mirabella F, et al. Effect of cilomilast (Ariflo) on TNF-alpha, IL-8, and GM-CSF release by airway cells of patients with COPD. Thorax 2003; 58: 573–9
Underwood DC, Bochnowicz S, Osborn RR, et al. Antiasthmatic activity of the second generation phosphodiesterase 4 (PDE4) inhibitor SB 207499 (Ariflo) in the guinea pig. J Pharmacol Exp Ther 1998; 287: 988–95
Compton CH, Gubb J, Nieman R, et al. Cilomilast, a selective phosphodiesterase-4 inhibitor for treatment of patients with chronic obstructive pulmonary disease: a randomised, dose-ranging study. Lancet 2001; 358: 265–70
Nieman RB, Taneja DT, Armit O, et al. The effects of low dose SB207499, a second generation, oral PDE4 inhibitor, in patients with COPD. Eur Respir J. 199; 14 Suppl 30: 331S
A 12-week, multicenter, double-blind, placebo-controlled, parallel-group study to evaluate the anti-inflammatory activity of cilomilast 15 mg twice daily in patients with chronic obstructive pulmonary disease (COPD) (SB207499/110) [GSK Clinical Trial Registry; online]. Available from URL: http://www.gsk-clinicalstudyregister.com [Accessed 2008 Nov 17]
A 13-week randomised, double-blind, parallel group, multicentre study to compare the bronchial anti-inflammatory activity of oral cilomilast (15 mg bd) with placebo twice daily in subjects with chronic obstructive pulmonary disease (COPD) (SB207499/181) [GSK Clinical Trial Registry; online]. Available from URL: http://www.gsk-clinicalstudyregister.com [Accessed 2008 Nov 17]
A randomised, double-blind, placebo-controlled, parallel-group study to evaluate the efficacy, safety and tolerability of oral cilomilast (15 mg bd) when given as maintenance treatment for 12 months to subjects with chronic obstructive pulmonary disease (COPD) (SB207499/156) [GSK Clinical Trial Registry; online]. Available from URL: http://www.gsk-clinical-studyregister.com [Accessed 2008 Nov 17]
A randomized, 24-week, double-blind, placebo-controlled, parallel-group study to evaluate the efficacy, safety and tolerability of ARIFLO® (15mg BID) in patients with chronic obstructive pulmonary disease (COPD) (CIL103657) [ClinicalTrials.gov identifier NTC 00103922], ClinicalTrials.gov [online]. Available from URL: http://www.gsk-clinicalstudyregister.com [Accessed 2008 Nov 17]
A randomized, 24-week, double-blind, placebo-controlled, parallel-group study followed by a 2-week, randomized, double-blind, run-out phase to evaluate the efficacy, safety, tolerability and discontinuation of SB207499 (15mg twice daily) in patients with chronic obstructive pulmonary disease (COPD) (SB207499/091) [GSK Clinical Trial Registry; online]. Available from URL: http://www.gsk-clinicalstudyregister.com [Accessed 2008 Nov 17]
A randomized, 24-week, double-blind, placebo-controlled, parallel-group study to evaluate the efficacy, safety and tolerability of cilomilast (15mg twice daily) in patients with chronic obstructive pulmonary disease (COPD) (SB207499/042) [GSK Clinical Trial Registry; online]. Available from URL: http://www.gsk-clinicalstudyregister.com [Accessed 2008 Nov 17]
Borg G. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982; 14: 377–81
A multicentre open-label extension study to evaluate the safety, tolerability and efficacy of oral SB-207499 (15 mg twice daily) in patients with chronic obstructive pulmonary disease (COPD). (SB207499/040) [GSK Clinical Trial Registry; online]. Available from URL: http://www.gsk-clinicalstudyregister.com [Accessed 2008 Nov 17]
A multicenter open-label extension study to evaluate the safety, tolerability and efficacy of oral cilomilast (15 mg twice daily) in patients with chronic obstructive pulmonary disease (COPD) (SB207499/041) [GSK Clinical Trial Registry; online]. Available from URL: http://www.gsk-clinicalstudyregister.com [Accessed 2008 Nov 17]
A randomised, double-blind, placebo-controlled, parallel-group study to evaluate the efficacy, safety and tolerability of oral cilomilast (15 mg bd) when given as maintenance treatment for 12 months to subjects with chronic obstructive pulmonary disease (COPD) (SB207499/157) [GSK Clinical Trial Registry; online]. Available from URL: http://www.gsk-clinical-studyregister.com [Accessed 2008 Nov 17]
A randomized, 12-week, double-blind, placebo-controlled, parallel-group study to evaluate the safety and tolerability of cilomilast 15mg twice daily in patients with chronic obstructive pulmonary disease (COPD) (SB207499/168) [GSK Clinical Trial Registry; online], Available from URL: http://www.gsk-clinicalstudyregister.com [Accessed 2008 Nov 17]
A randomized, 12-week, double-blind, placebo-controlled, parallel-group pilot study to evaluate the safety and additional efficacy of adding a new chemical entity (NCE) to treatment with ADVAIR 250/50 twice daily in patients with chronic obstructive pulmonary disease (COPD) (SB207499/125) [GSK Clinical Trial Registry; online]. Available from URL: http://www.gsk-clinicalstudyregister.com [Accessed 2008 Nov 17]
A 12-week, randomized, double-blind, placebo-controlled, parallel-group study to investigate the effect of cilomilast (15 mg twice daily) on trapped gas volume in patients with chronic obstructive pulmonary disease (SB207499/111) [GSK Clinical Trial Registry; online]. Available from URL: http://www.gskclinicalstudyregister.com [Accessed 2008 Nov 17]
An 18-week randomized, double-blind, placebo-controlled, multicenter study designed to compare treatment with cilomilast to that with placebo for changes in ventilatory mechanics and function (both at rest and during exercise), as well as related exertional dyspnea and exercise performance, in hyperinflated patients with stable COPD (SB207499/180) [GSK Clinical Trial Registry; online]. Available from URL: http://www.gsk-clinicalstudyregister.com [Accessed 2008 Nov 17]
Blonshine S, Foss C, Mottram C, et al. AARC clinical practice guideline. Body plethysmography: 2001 revision and update. Respir Care 2001; 46: 506–13
O’Donnell DE, Webb KA. Exertional breathlessness in patients with chronic airflow limitation: the role of hyperinflation. Am Rev Respir Dis 1993; 148: 1351–7
O’Donnell DE, Lam M, Webb KA. Measurement of symptoms, lung hyperinflation and endurance during exercise in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998(b); 158:1557–65
A randomized, 24-week, double-blind, placebo-controlled, parallel-group study to evaluate the efficacy, safety and tolerability of cilomilast (15mg BID) in patients with chronic obstructive pulmonary disease (COPD). (SB207499/121) [GSK Clinical Trial Registry; online]. Available from URL: http://www.gsk-clinicalstudyregister.com [Accessed 2008 Nov 17]
Anthonisen NR. Connett JE. Muruay RP. Smoking and lung function of lung health study participants. Am J Respir Crit Care Med 2002; 66(3): 675–9
Barnes NC, Qiu YS, Pavord ID, et al. Anti-inflammatory effects of salmeterol/fluticasone propionate in chronic obstructive lung disease. Am J Respir Crit Care Med 2006; 173: 736–43
Decramer M, Rutten-van Molken M, Dekhuijzen PN, et al. Effects of N-acetylcysteine on outcomes in chronic obstructive pulmonary disease (Bronchitis Randomized on NAC Cost-Utility Study, BRONCUS): a randomised placebo-controlled trial. Lancet 2005; 365: 1552–60
Saetta M. Airway inflammation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1999; 160: S17–20
Anthonisen NR, Wright EC, Hodgkin JE, et al. Prognosis in chronic obstructive pulmonary disease. Am Rev Respir Dis 1986; 133: 14–20
Postma DS, Sluiter HJ. Prognosis of chronic obstructive pulmonary disease: the Dutch experience. Am Rev Respir Dis 1989; 140: S100–5
O’Donnell DE, Revill SM, Webb KA. Dynamic hyperinflation and exercise intolerance in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2001; 164: 770–7
Marin JM, Carrizo SJ, Gascon M, et al. Inspiratory capacity, dynamic hyperinflation, breathlessness, and exercise performance during the 6-minute-walk test in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2001; 163: 1395–9
Wijkstra PJ, Ten Vergert EM, van der Mark TW, et al. Relation of lung function, maximal inspiratory pressure, dyspnoea, and quality of life with exercise capacity in patients with chronic obstructive pulmonary disease. Thorax 1994; 49: 468–72
Osman LM, Godden DJ, Friend JAR, et al. Quality of life and hospital re-admission in patients with chronic obstructive pulmonary disease. Thorax 1997; 52: 67–71
Jones PW, Quirk FH, Baveystock CM, et al. A self-complete measure of health status for chronic airflow limitation, the St. George’s Respiratory Questionnaire. Am Rev Respir Dis 1992; 145: 1321–7
Braunholtz DA, Edwards SJ, Lilford RJ. Are randomized clinical trials good for us (in the short term)? Evidence for a “trial effect”. J Clin Epidemiol 2001; 54: 217–24
Stevenson NJ, Walker PP, Costello RW, et al. Lung mechanics and dyspnea during exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2006; 172:1510–6
Papi A, Bellettato CM, Braccioni F, et al. Infections and airway inflammation in chronic obstructive pulmonary disease severe exacerbations. Am J Respir Crit Care Med 2006; 173: 1114–21
Sethi S, Maloney J, Grove L, et al. Airway inflammation and bronchial bacterial colonization in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2006; 173: 991–8
Seemungal TA, Donaldson GC, Paul EA, et al. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998; 157: 1418–22
Spencer S, Calverley PM, Burge PS, et al. Impact of preventing exacerbations on deterioration of health status in COPD. Eur Respir J 2004; 23: 698–702
Andersson F, Borg S, Jannson SA, et al. The costs of exacerbations in chronic obstructive pulmonary disease. Respir Med 2002; 96: 700–8
Soler-Cataluna JJ, Martinez-Garcia MA, Roman Sanchez P, et al. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 2005; 60: 925–31
Seemungal TA, Donaldson GC, Bhowmik A, et al. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2000; 161(5): 1608–13
Acknowledgements
The authors acknowledge technical support from Diana Jones, a professional medical writer, who was compensated by GlaxoSmithKline (GSK), in the preparation of this manuscript.
SR has had or currently has a number of relationships with companies who provide products and/or services relevant to outpatient management of chronic obstructive pulmonary disease. These relationships include serving as a consultant, advising regarding clinical trials, speaking at continuing medical education programmes and performing funded research both at basic and clinical levels. He does not own stock in any pharmaceutical companies. In the last 3 years, SR has received laboratory and industry grants from Almirall, Altana, Astellas, Centocor, GSK, Nabi, Novartis and Pfizer; has served on consultancy and advisory boards for Adams, Almirall, Altana, AstraZeneca, Bend, Biolipox, Centocor, Critical Therapeutics, Dey, GSK, ICOS, Johnson & Johnson, Novartis, Ono Pharma, Parengenix, Pfizer, Roche, Sankyo, Sanofi, Schering-Plough and Talecris; and has received speakers fees from AstraZeneca, Boehringer Ingelheim, GSK, Osuka and Pfizer. AM is an employee of GSK (clinical) and owns stock and stock options in GSK. FB is an employee of GSK (clinical) and holds stock options with GSK. KR has been consulting, participated in Advisory Board meetings and received lecture fees from AstraZenica, Boehringer, Chiesi Pharmaceuticals, Pfizer, Novartis, AltanaPharma, MSD and GSK. The Department of Pulmonology, and thereby Professor Rabe as head of the department, has received grants from Novartis, AstraZeneca, Boehrigner Ingelheim, Roche and GSK between 2005 and 2008 and has a grant pending from Polen. NL has been an employee of GSK (statistician) since 2003. KK is an employee of GSK (clinical) and holds stock options in GSK. NS, WGC and YZ have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rennard, S., Knobil, K., Rabe, K.F. et al. The Efficacy and Safety of Cilomilast in COPD. Drugs 68 (Suppl 2), 3–57 (2008). https://doi.org/10.2165/0003495-200868002-00002
Published:
Issue Date:
DOI: https://doi.org/10.2165/0003495-200868002-00002