Abstract
Background: Given the number of antidepressants available and their rising costs, healthcare payers have initiated restrictive reimbursement policies for newer antidepressants, without consideration for differences in their effectiveness or tolerability.
Objective: The objective of this study was to comprehensively compare medication adherence rates and associated healthcare utilization costs for patients using later-generation versus earlier-generation antidepressants in a managed care setting. Antidepressants launched after 2002 were deemed third-generation antidepressants, while antidepressants available prior to 2002 were deemed first-generation (TCAs and MAOIs) and second-generation (serotonin and noradrena-line [norepinephrine]-dopamine reuptake inhibitors).
Study design: Retrospective database analysis using medical and pharmacy data from over 75 managed care plans covering 55 million lives.
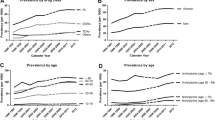
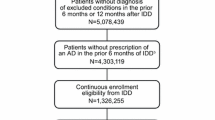
Setting/patients: All patients receiving an antidepressant between 1 January 2002 and 30 September 2004 were identified. The index date for patients was the date of their first antidepressant prescription within this time period. Patients had to (i) have a diagnosis of depression or anxiety disorder, or depression and anxiety disorder within 6 months prior to or 30 days after their index prescription; (ii) be at least 18 years of age, without having taken antidepressant therapy for 6 months prior to their index date; and (iii) be continuously eligible for 6 months prior to their index date and during their 6-month follow-up period. Patients were excluded if they had a diagnosis of psychosis-related disease, Alzheimer’s or Parkinson’s disease, or were initiated on psychosis-related medications.
Intervention/main outcome measure: Patients meeting selection criteria were followed for 6 months to assess rates of antidepressant adherence, therapy change rates and medical healthcare costs.
Results: Study population: A total of 266 665 patients met the study criteria. Approximately 66% were female, with a mean age of 39 years. About 63% had a diagnosis of depression, 31% had an anxiety disorder diagnosis and 6% had diagnoses for both an anxiety disorder and depression. Therapy change: Therapy change within 6 months occurred in 18% of patients receiving third-generation agents compared with 21% and 40% for second- and first-generation agents, respectively. The odds of a therapy change were significantly lower with third-generation antidepressants compared with both older agent cohorts.
Adherence: Of patients receiving third-generation antidepressants, 33.6% were adherent compared with 29.3% and 12.4% of patients receiving second- and first-generation antidepressants, respectively. Newer agents also had better adherence rates across all diagnostic cohorts. After adjusting for baseline differences, the odds of being adherent to therapy were significantly lower for those taking second- and first-generation agents versus newer antidepressants. Among the newer agents, the proportion of patients adherent to their therapy was: venlafaxine extended release 38%, paroxetine controlled release (CR) 35%, escitalopram 34%, duloxetine 32% and bupropion extended release (XL) 31%.
Healthcare utilization: Of the patients taking older antidepressants, 13% (second generation) and 21% (first generation) were hospitalized at least once for any reason compared with 12% of patients taking newer agents. Overall, the odds of all-cause hospitalization within 6 months of therapy initiation were significantly higher for patients taking older antidepressants. Among the newer agents, hospitalization rates ranged from 15.9% for duloxetine to 12.5% for paroxetine CR and bupropion XL. The unadjusted 6-month total medical costs (not including pharmacy costs) per patient were $US3514 for second-generation, $US5744 forfirst-generation and $US3284 for newer antidepressants. After controlling for baseline differences, patients receiving second- and first-generation antidepressants incurred 12% and 44% higher costs, respectively. The unadjusted 6-month medical costs for the newer agents ranged from $US2715 for paroxetine CR to SUS6042 for duloxetine.
Conclusion: The results of this study provide essential information for healthcare decision makers about the potential advantages of newer generation antidepressants versus older generation antidepressants, as well as the differences between the specific newer agents, with respect to improved rates of adherence and therapy change, reduced hospitalizations and healthcare costs.













Similar content being viewed by others
References
Kessler RC, Berglund P, Dernier O, et al. The epidemiology of major depressive disorder: Results from the National Comor-bidity Survey Replication (NCS-R). JAMA 2003; 289: 3095–105
Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51: 8–19
Murray CJ, Jopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global burden of disease study. Lancet 1997; 349(9064): 1498–504
Arikian SR, Gorman JM. A review of the diagnosis, pharmacologic treatment, and economic aspects of anxiety disorders. Prim Care Companion J Clin Psychiatry 2001; 3(3): 110–7
Greenberg PE, Kessler RC, Birnbaum HG, et al. The economic burden of depression in the United States: how did it change between 1990 and 2000? J Clin Psychiatry 2003; 64: 1465–75
National Institute of Mental Health. Anxiety disorders [online]. Available from URL: http://www.nimh.nih.gov [Accessed 2007 Jun 25]
Anderson IM. Selective serotonin reuptake inhibitors versus tricyclic antidepressants: a meta-analysis of efficacy and tolerability. J Affect Disord 2000; 58(1): 19–36
Bandelow B, Zohar J, Hollander E, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive compulsive and posttraumatic stress disorders. World J Biol Psychiatry 2002; 3: 171–99
Sramek JJ, Zarotsky V, Cutler NR. Generalized anxiety disorder. Drugs 2002; 11: 1635–48
Blanco C, Raza MS, Schneier FR, et al. The evidence-based pharmacological treatment of social anxiety disorder. Int J Neuropsychopharmacol 2003; 6(4): 427–42
Zohar J, Keeqstra H, Barrelet L. Fluvoxamine as effective as clomipramine against symptoms of severe depression: results from a multi-center double blind study. Hum Psychopharmacol 2003; 18(2): 113–9
IMS Health. 2004 year-end U.S. prescription and sales information and commentary [online]. Available from URL: http://www.imshealth.com/ims/portal/front/articleC/0,2777,6599_3-665_69890098,00.html [Accessed 2006 Dec 5]
Keene MS, Eaddy MT, Mauch RP, et al. Differences in compliance patterns across the selective serotonin reuptake inhibitors (SSRIs). Curr Med Res Opin 2005; 21(10): 1651–8
Keene MS, Eaddy MT, Nelson WW, et al. Adherence to paroxetine CR compared with paroxetine IR in a Medicare-eligible population with anxiety disorders. Am J Manag Care 2005; 11 Suppl. 12: S362–9
Sheehan DV, Eaddy MT, Shah MB, et al. Differences in total medical costs across the SSRIs for the treatment of depression and anxiety. Am J Manag Care 2005; 11Suppl. 12: S354–61
Eaddy MT, Bramley T, Regan TS. Time to antidepressant discontinuation: a comparison of controlled-release paroxetine and immediate-release selective serotonin reuptake inhibitors. Manag Care Interface 2003; 16: 22–7
Kennedy SH, Andersen HF, Lam RW. Efficacy of escitalopram in the treatment of major depressive disorder compared with conventional serotonin reuptake inhibitors and venlafaxine XR: a meta-analysis. J Psychiatry Neurosci 2006; 31(2): 122–31
Rush AJ, Trivedi MH, Wisniewski SR. Bupropion SR, sertraline, venlafaxine XR after failure of SSRIs for depression. N Engl J Med 2006; 354(12): 1231–42
Baldomero EB, Ubago JG, Cercos CL, et al. Venlafaxine extended-release versus conventional antidepressants in the remission of depressive disorders after previous antidepressant failure: ARGOS study. Depress Anxiety 2005; 22(2): 68–76
Silverstone PH, Ravindran A. Once-daily venlafaxine extended-release (XR) compared with fluoxetine in outpatients with depression and anxiety: Venlafaxine 360 Study Group. J Clin Psychiatry 1999; 60(1): 22–8
Boulenger JP, Huusom AKT, Florea I, et al. A comparative study of the efficacy and tolerability of long-term treatment with escitalopram and paroxetine in severe major depression [poster]. International Conference on Anxiety Disorders; 2006 Feb 24–26; Stellenbosch
International classification of diseases, 9th revision, clinical modification (ICD-9-CM). Geneva: World Health Organization, 2007
Steiner J, Prochazka A. The assessment of refill compliance using pharmacy records: Methods, validity, and applications. J Clin Epidemiol 1997; 50: 105–16
Cantrell CR, Eaddy MT, Shah MB, et al. Methods for evaluating patient adherence to antidepressant therapy: a real-world comparison of adherence and economic outcomes. Med Care 2006; 44(4): 300–3
Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–83
Deyo R, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992; 45: 613–9
Eaddy M, Sarnes M, Regan T, et al. Examining the relationship between length of selective serotonin reuptake inhibitor treatment and the risk of hospitalization in a naturalistic managed care setting [poster]. Academy of Managed Care Pharmacy 2004 Educational Conference; 2004 Oct 13–16; Baltimore (MD)
Claxton AJ, Li Z, McKendrick J. Selective serotonin reuptake inhibitor treatment in the UK: risk of relapse or recurrence of depression. Br J Psychiatry 2000; 177: 163–8
Debonnel G, Saint-André E, Hébert C, et al. Differential physiological effects of a low dose and high doses of venlafaxine in major depression. Int J Neuropsychopharmacol 2007 Feb; 10(1): 51–61.
Acknowledgements
This study was supported by a Collaborative Research Grant from GlaxoSmithKline. Management of the study, data analysis and interpretation were conducted by Dr Sheehan, and Dr Eaddy and his team at Xcenda, independent of the funding source. Mr Krulewicz, Dr Kraus and Dr Carpenter, employees of GlaxoSmithKline, participated in the study design and in the review of the manuscript. Dr Sheehan has worked, on a contractual basis, as a consultant to Xcenda and to GlaxoSmithKline. He received an honorarium from Xcenda for his consulting work on this study. He has received three grants for clinical trials through the University of South Florida from GlaxoSmithKline over the past 5 years. Dr Keene has worked, on a contractual basis, as a consultant to Xcenda. He received an honorarium from Xcenda for his consulting work on this study. Dr Eaddy is an employee of Xcenda. Xcenda provides consulting services to GlaxoSmithKline on a contractual basis. Mr Krulewicz and Dr Carpenter own stock and/or options in GlaxoSmithKline. In addition to Dr Eaddy, the Xcenda team included: Timothy S. Regan, RPh, CPh, research design and manuscript review; Anuprita Patkar, PhD, research design and database analysis; Anna D’Souza, PhD, database analysis and manuscript preparation; and Amy L. Grabowski, study management and manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sheehan, D.V., Keene, M.S., Eaddy, M. et al. Differences in Medication Adherence and Healthcare Resource Utilization Patterns. CNS Drugs 22, 963–973 (2008). https://doi.org/10.2165/00023210-200822110-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00023210-200822110-00005