Abstract
Synopsis
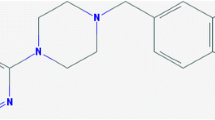
The semisynthetic ergotine dopamine agonist pergolide has demonstrated activity at pre- and postsynaptic dopamine D2 receptors in vitro and in vivo animal studies. However, unlike other dopamine agonists such as bromocriptine, pergolide also has agonist activity at dopamine D1 receptors. Certain other pharmacological effects of pergolide, such as reduction of dopamine turnover and effects on free radical scavenging enzymes, may be relevant in the early treatment of Parkinson’s disease but this has not been conclusively determined.
Short and long term noncomparative studies show that pergolide is an effective adjunct to levodopa therapy in patients with advancing Parkinson’s disease, reducing the adverse effects of long term levodopa monotherapy and often enabling a reduction in levodopa dosage. In placebo comparisons pergolide was generally more effective than placebo and was associated with benefits similar to those seen in noncomparative studies.
Longitudinal comparisons in individual patients indicate that the antiparkinsonian efficacy of pergolide is similar to that of mesulergine, lergotrile and lisuride, and may be superior to that of bromocriptine. Controlled comparisons with bromocriptine tend to support this latter finding.
Studies evaluating the efficacy of pergolide as monotherapy early in the course of Parkinson’s disease have shown the drug to be effective, but opinion is divided as to the value of early treatment with dopamine agonists (as opposed to levodopa monotherapy).
Thus, pergolide is an effective adjunct to levodopa therapy in patients with advanced Parkinson’s disease and may have a role in the treatment of early disease if its postulated beneficial effects on disease progression are proven.
Pharmacodynamic Properties
Pergolide is a semisynthetic ergoline dopamine agonist used in the treatment of Parkinson’s disease. It has potent activity at presynaptic dopamine D2 receptors but is also active at postsynaptic D2 and dopamine D1 receptors.
In vitro, pergolide suppressed D2-mediated prolactin release from rat anterior pituitary fragments and inhibited potassium-mediated dopamine or acetylcholine release from rat caudate slices. Pergolide-induced activation of rat striatal D1 receptors has been shown to stimulate adenylate cyclase activity which, in turn, increased production of cyclic AMP.
The majority of receptor binding studies indicate that pergolide is considerably more selective for D2 than for D1 receptors.
In vivo, pergolide has been shown to induce contralateral turning in rats with right-side nigrostriatal lesions; it also induced climbing in rats selected on the basis of a climbing response to apomorphine.
Pergolide had similar actions to those of selective D2 agonists in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced hemiparkinsonian monkeys but was more potent than selective D1 agonists. Pergolide improved parkinsonian symptoms in another study in this model. Its effects were more marked, but of shorter duration, than those of bromocriptine or cabergoline.
One theory regarding the cause of Parkinson’s disease is that metabolism of dopamine produces free radicals which damage nigral neurons. Its effects on oxygen radical scavenging enzymes are unclear; the drug induced Superoxide dismutase in one in vivo animal study but had no effect in another (but did induce catalase and glutathione peroxidase).
Pharmacokinetic Properties
Single 1, 2, 5 and 10mg doses of pergolide produced mean peak plasma concentrations (Cmax) of 2.09, 4.57, 20.3 and 26 μg/L, respectively, in rhesus monkeys (administration of therapeutic doses to volunteers was considered unethical). The time to Cmax ranged between 2.4 and 2.7 hours at all dose levels.
Mean steady-state pergolide plasma concentrations of 0.0275 to 1.167 μg/L were recorded during treatment with pergolide 2.25 to 9 mg/day in patients with Parkinson’s disease; extensive interpatient variability was noted.
55% of a 0.138mg radiolabelled oral dose of pergolide was excreted in the urine of volunteers; a further 40 to 50% of radioactivity appeared in the faeces and approximately 3% appeared in expired air.
Analysis of urine and faecal extracts indicated the formation of 10 or more metabolites.
Therapeutic Use
A large noncomparative Japanese study has evaluated the short term efficacy of pergolide in combination with levodopa ± carbidopa (n = 314) or as monotherapy (n = 86). Addition of pergolide allowed a significant reduction in levodopa dosage and about 65% of patients experienced at least a mild improvement in wearing off and on-off phenomena. 45.3% of monotherapy recipients experienced at least moderate improvement according to a final global rating scale (vs 52.9% of combination therapy recipients).
Additional noncomparative studies in Australian, Thai, Chinese and Italian patients also reported adjunctive pergolide therapy to be effective.
Early noncomparative long term studies reported an initial response to pergolide but the rate of clinical improvement tended to peak after 2 to 12 months, then decline. However, it does appear that the efficacy of pergolide, despite waning, can be maintained at a satisfactory level for several years.
A long term continuation of the Japanese study discussed above reported a final global improvement rate that was at least moderate in 51.4% of adjunctive pergolide therapy recipients treated for at least 1 year, although the drug tended to become less effective after this time. 62 monotherapy recipients were included in this long term continuation; final global improvement rates were similar (moderate or greater in 61.3% of monotherapy recipients vs 51.4% in the combination therapy group).
Results from a large 6-month multicentre double-blind placebo comparison have confirmed the result of earlier, smaller placebo comparisons. Pergolide recipients (n = 189) experienced a significantly greater improvement in many subjective measures of disease severity than placebo recipients. Pergolide allowed a 24.7% reduction in levodopa dosage compared with an approximate 5% reduction with placebo.
On the basis of longitudinal sequential comparisons in individual patients, pergolide was considered to have similar utility to mesulergine, lergotrile and lisuride and appeared to be more effective than bromocriptine. In addition, a number of controlled studies reported that although both drugs were useful, pergolide tended to allow a greater reduction in levodopa dosage than bromocriptine. The sole available comparison of pergolide and bromocriptine as monotherapy reported the 2 drugs to be similarly effective.
Tolerability
Postural hypotension occurs quite frequently in patients starting pergolide therapy but usually diminishes over time.
In a recent placebo comparison, adverse events occurring significantly more frequently in pergolide recipients included dyskinesia (62% in the pergolide group vs 25% in placebo recipients), nausea (24 vs 13%), hallucinations (14 vs 3%), drowsiness (10 vs 3%), insomnia (8 vs 3%), nasal congestion (7 vs 1%), dyspepsia (6 vs 2%) and dyspnoea (5 vs 1%).
ECG changes and palpitations have been noted in some patients receiving pergolide during clinical trials and close observation may be needed in patients with concomitant heart disease; limited data indicate that addition of domperidone attenuates these cardiac adverse events.
Rarely, abrupt withdrawal of pergolide therapy can cause confusion or hallucinations; thus, when required, cessation of pergolide therapy should be gradual.
Dosage and Administration
To avoid first dose hypotension and other adverse effects such as nausea and vomiting, pergolide therapy must be initiated at a low dosage (often 0.05 mg/day for 2 days). The dose should be slowly increased until maximum clinical benefit is achieved with no or minimal adverse effects.
The drug is administered in divided doses, usually 3 or 4 times per day, and the most frequent effective total daily dose is 3 to 4mg; however, mean effective dosages were somewhat lower in Japanese studies.
Similar content being viewed by others
References
Langtry HD, Clissold SP. Pergolide: a review of its pharmacological properties and therapeutic potential in Parkinson’s disease. Drugs 1990 Mar; 39: 491–506
Gingrich JA, Caron MG. Recent advances in the molecular biology of dopamine receptors. Annu Rev Neurosci 1993; 16: 299–321
Stamford JA, Kruk ZL, Millar J. Differential effects of dopamine agonists upon stimulated limbic and striatal dopamine release: in vivo voltammetric data. Br J Pharmacol 1991 Jan; 102: 45–50
Zhang X-X, Jin G-Z, Wei Y-F. Agonistic actions of pergolide on firing activity of dopamine neurons in substantia nigra compacta area. Acta Pharmacol Sin 1995 Sep; 16: 423–7
Jenner P. The rationale for the use of dopamine agonists in Parkinson’s disease. Neurology 1995 Mar; 45 Suppl. 3: S6–S12
Montastruc JL, Rascol O, Senard JM. Current status of dopamine agonists in Parkinson’s disease management. Drugs 1993 Sep; 46: 384–93
Robin DW. Pergolide in the treatment of Parkinson’s disease. Am J Med Sci 1991 Apr; 301: 277–80
Schaus JM, Clemens JA. Dopamine receptors and dopaminergic agents. Ann Rep Med Chem 1985; 21: 41–50
Foreman MM, Fuller RW, Hynes MD, et al. Preclinical studies on quinelorane, a potent and highly selective D2-dopaminergic agonist. J Pharmacol Exp Ther 1989 Jul; 250: 227–35
Boissier JR, Euvrard C, Oberlander C, et al. Comparative study of central dopaminergic properties of RU 29717 (N-propyl-9-oxaergoline) and pergolide. Eur J Pharmacol 1983 Feb 18; 87: 183–9
Fuller RW, Clemens JA. Pergolide: a dopamine agonist at both D1-receptors and D2-receptors. Life Sci 1991; 49(13): 925–30
Wong DT, Threlkeld PG, Bymaster FP. Dopamine receptor affinities in vitro and neurochemical effects in vivo of pergolide and its metabolites. Arzneimittel Forschung 1993 Apr; 43: 409–12
Uitti RJ, Ahlskog JE. Comparative review of dopamine receptor agonists in Parkinson’s disease. CNS Drugs 1996 May; 5: 369–88
Clemens JA, Okimura T, Smalstig EB. Dopamine agonist activities of pergolide, its metabolites, and bromocriptine as measured by prolactin inhibition, compulsive turning, and Stereotypic behavior. Arzneimittel Forschung 1993 Mar; 43: 281–6
Davis A, Jenner P, Marsden CD. Differential ability of selective and non-selective dopamine agonists to induce climbing in the rat indicates the involvement of both D-1 and D-2 receptors in this behaviour. Psychopharmacology Berl 1990; 100: 19–26
Domino EF, Sheng J. Relative potency and efficacy of some dopamine agonists with varying selectivities for D1 and D2 receptors in MPTP-induced hemiparkinsonian monkeys. J Pharmacol Exp Ther 1993 Jun; 265: 1387–91
Arai N, Isaji M, Miyata H, et al. Differential effects of three dopamine receptor agonists in MPTP-treated monkeys. J Neural Transm Park Dis Dement Sect 1995; 10(1): 55–62
Feiten DL, Feiten SY, Fuller RW, et al. Chronic dietary pergolide preserves nigrostriatal neuronal integrity in aged-Fischer-344 rats. Neurobiol Aging 1992 Mar–Apr; 13: 339–51
DiMauro S. Mitochondrial involvement in Parkinson’s disease: the controversy continues. Neurology 1993; 43: 2170–2
Clow A, Freestone C, Lewis E, et al. The effect of pergolide and MDL 72974 on rat brain CuZn Superoxide dismutase. Neurosci Lett 1993 Dec 24; 164: 41–3
Pattichis K, Louca LL, Clow A, et al. Effects of pergolide, (-)-deprenyl and thioridazine on soluble SOD, catalase and glutathione peroxidase in rat striata. Med Sci Res 1995 Nov; 23: 733–5
Iwasaki Y, Ikeda K, Shiojima T, et al. The effect of pergolide and deprenyl on axotomy-induced cell death in the spinal motor neuron of the rat [abstract]. Ann Neurol 1994 Aug; 36: 282–3
Rubin A, Lemberger L, Dhahir P. Physiologic disposition of pergolide. Clin Pharmacol Ther 1981 Aug; 30: 258–65
Bowsher RR, Apathy JM, Compton JA, et al. Sensitive, specific radioimmunoassay for quantifying pergolide in plasma. Clin Chem 1992 Oct; 38: 1975–80
Lang AE, Quinn N, Brincat S, et al. Pergolide in late-stage Parkinson disease. Ann Neurol 1982 Sep; 12: 243–7
Mear JY, Barroche G, de-Smet Y, et al. Pergolide in the treatment of Parkinson’s disease. Neurology 1984 Jul; 34: 983–6
Lieberman A, Goldstein M, Leibowitz M, et al. Treatment of advanced Parkinson disease with pergolide. Neurology 1981 Jun; 31: 675–82
Narabayashi H, Ando K, Kowa H, et al. Phase II study of pergolide mesylate (LY127809) in Parkinson’s disease — multicenter open study [in Japanese]. Rinsho Iyaku 1991; 7(1): 151–90
Hely MA, Morris JGL, Burns RJ, et al. An Australian multicentre open label study of pergolide as an adjunct to levodopa in Parkinson’s disease. J Clin Neuroscience 1996 Jul; 3(3): 234–8
Poungvarin N, Prayoonwiwat N, Devahasatin V, et al. An open label trial of pergolide in Thai patients with Parkinson’s disease. J Med Assoc Thai 1996 Apr; 79: 205–9
Shan D-E, Yeh S-I. Experience of pergolide in the treatment of Chinese parkinsonian patients with dose-related fluctuations. Chung Hua I Hsueh Tsa Chih Taipei 1995 Nov; 56: 312–8
Pezzoli G, Zecchinelli A, Mariani C, et al. Pergolide mesylate in the treatment of Parkinson’s disease resistant to other treatments. First Italian experience [in Italian]. Clin Ter 1991 Jan 15; 136: 39–45
Ahlskog JE, Muenter MD. Pergolide: long-term use in Parkinson’s disease. Mayo Clin Proc 1988 Oct; 63: 979–87
Diamond SG, Markham CH. One-year trial of pergolide as an adjunct to Sinemet in treatment of Parkinson’s disease. Adv Neurol 1984; 40: 537–9
Factor SA, Sanchez-Ramos JR, Weiner WJ. Parkinson’s disease: an open label trial of pergolide in patients failing bromocriptine therapy. J Neurol Neurosurg Psychiatry 1988 Apr; 51: 529–33
Goetz CG, Tanner CM, Glantz R, et al. Pergolide in Parkinson’s disease. Arch Neurol 1983 Dec; 40: 785–7
Goetz CG, Tanner CM, Glantz RH, et al. Chronic agonist therapy for Parkinson’s disease: a 5-year study of bromocriptine and pergolide. Neurology 1985 May; 35: 749–51
Jankovic J. Long-term study of pergolide in Parkinson’s disease. Neurology 1985 Mar; 35: 296–9
Jeanty P, Van-den-Kerchove M, Lowenthal A, et al. Pergolide therapy in Parkinson’s disease. J Neurol 1984; 231: 148–52
Klawans HL, Tanner CM, Glatt S, et al. A 6-month trial of pergolide mesylate in the treatment of idiopathic Parkinson’s disease. Adv Neurol 1983; 37: 75–83
Kurlan R, Miller C, Levy R, et al. Long-term experience with pergolide therapy of advanced parkinsonism. Neurology 1985 May; 35: 738–42
Lieberman AN, Goldstein M, Gopinathan G, et al. Further studies with pergolide in Parkinson disease. Neurology 1982 Oct; 32: 1181–4
Lieberman AN, Goldstein M, Neophytides A, et al. The use of pergolide, a potent dopamine agonist, in Parkinson’s disease. Clin Pharmacol Ther 1982 Jul; 32: 70–5
Lieberman AN, Goldstein M, Leibowitz M, et al. Long-term treatment with pergolide: decreased efficacy with time. Neurology 1984 Feb; 34: 223–6
Lieberman AN, Goldstein M, Gopinathan G, et al. D-1 and D-2 agonists in Parkinson’s disease. Can J Neurol Sci 1987; 14: 466–73
Quinn NP, Lang AE, Thompson C, et al. Pergolide in the treatment of Parkinson’s disease. Adv Neurol 1984; 40: 509–13
Sage JI, Duvoisin RC. Long-term efficacy of pergolide in patients with Parkinson’s disease. Clin Neuropharmacol 1986; 9: 160–4
Lichter D, Kurlan R, Miller C, et al. Does pergolide slow the progression of Parkinsion’s disease? A 7 year follow-up study [abstract]. Neurology 1988; 38(3): 122
Zimmerman T, Sage JI. Comparison of combination pergolide and levodopa to levodopa alone after 63 months of treatment. Clin Neuropharmacol 1991 Apr; 14: 165–9
Narabayashi H, Ando Kal, Kowa H, et al. Long-term study of pergolide mesilate (LY 127809) in Parkinson’s disease -multicenter open study [in Japanese]. Igaku Yakugaku 1992; 27(2): 471–529
Ahlskog JE, Muenter MD. Treatment of Parkinson’s disease with pergolide: a double-blind study. Mayo Clin Proc 1988 Oct; 63: 969–78
Diamond SG, Markham CH, Treciokas LJ. Double-blind trial of pergolide for Parkinson’s disease. Neurology 1985 Mar; 35: 291–5
Grimes JD, Hassan MN, Sitwell LD, et al. Pergolide in the management of advanced Parkinson’s disease. Can J Neurol Sci 1985; 12: 173
Olanow CW, Alberts MJ. Double-blind controlled study of pergolide mesylate in the treatment of Parkinson’s disease. Clin Neuropharmacol 1987 Apr; 10: 178–85
Sage JI, Duvoisin RC. Pergolide therapy in Parkinson’s disease: a double-blind, placebo-controlled study. Clin Neuropharmacol 1985; 8: 260–5
Jankovic J, Orman J. Parallel double-blind study of pergolide in Parkinson’s disease. In: Yahr, Bergmann, editors. Advances in neurology. Vol. 45. New York: Raven Press, 1986: 551–4
Olanow CW, Fahn S, Muenter M, et al. A multicenter double-blind placebo-controlled trial of pergolide as an adjunct to Sinemet® in Parkinson’s disease. Mov Disord 1994 Jan; 9: 40–7
Lieberman AN, Leibowitz M, Gopinathan G, et al. The use of pergolide and lisuride, two experimental dopamine agonists, in patients with advanced Parkinson disease. Am J Med Sci 1985 Sep; 290: 102–6
Lieberman AN, Gopinathan G, Neophytides A. Efficacy of pergolide and mesulergine. Eur Neurol 1986; 25: 86–90
Lieberman AN, Goldstein M, Leibowitz M. Comparative efficacy of two dopamine agonists, pergolide and lergotrile, in Parkinson disease. N Y State J Med 1988 Aug; 88: 420–2
Lieberman AN, Neophytides A, Leibowitz M, et al. Comparative efficacy of pergolide and bromocriptine in patients with advanced Parkinson’s disease. Adv Neurol 1983; 37: 95–108
Goetz CG, Shannon KM, Tanner CM, et al. Agonist substitution in advanced Parkinson’s disease. Neurology 1989 Aug; 39: 1121–2
Boas J, Worm-Petersen J, Dupont E, et al. The levodopa dose-sparing capacity of pergolide compared with that of bromocriptine in an open-label crossover study. Eur J Neurol 1996 Jan; 3: 44–9
LeWitt PA, Ward CD, Larsen TA, et al. Comparison of pergolide and bromocriptine therapy in parkinsonism. Neurology 1983 Aug; 33: 1009–14
Narabayashi H et al. Clinical utility of pergolide mesilate (LY 127809) on Parkinson’s disease. Double blind study in comparison with bromocriptine mesilate [in Japanese]. Igaku Yakugaku 1992; 27(1): 147–207
Pezzoli G, Martignoni E, Pacchetti C, et al. A crossover, controlled study comparing pergolide with bromocriptine as an adjunct to levodopa for the treatment of Parkinson’s disease. Neurology 1995 Mar; 45 Suppl. 3: S22–7
Bonnet AM, Serre I, Marconi R, et al. A combined levodopa test as a useful method for evaluating the efficacy of dopamine agonists: application to pergolide and bromocriptine. Mov Disord 1995 Sep; 10: 668–71
Mizuno Y, Mori H, Kondo T. Practical guidelines for the drug treatment of Parkinson’s disease. CNS Drugs 1994 Jun; 1: 410–26
Rinne UK. Dopamine agonists as primary treatment in Parkinson’s disease. Adv Neurol 1986; 45: 519–23
Goetz CG, Diederich NJ. Dopaminergic agonists in the treatment of Parkinson’s disease. Neurol Clin 1992 May; 10: 527–40
Bravi D, Nohria V, Megas LF. Dopamine agonists in the clinical management of Parkinson’s disease: symptomatic or neuroprotective treatment? Eur J Neurol 1996 May; 3 Suppl. 1: 13–8
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: J. Boas, University Department of Neurology, Glostrup Hospital, Glostrup, Denmark; A-M. Bonnet, Fédération de Neurologie, Groupe Hospitalier Pitié-Salpétrière, Paris, France; M.J. Eadie, Department of Medicine, University of Queensland, Herston, Queensland, Australia; P. Jenner, Biomedicai Sciences Division, Pharmacology Group, King’s College London, London, England; C.D. Marsden, University Department of Clinical Neurology, National Hospital, London, England; J-L. Montastruc, Faculté de Médecine, Centre Hospitalier Universitaire, Hôpitaux de Toulouse, Toulouse, France; H. Narabayashi, Neurological Clinic, Tokyo, Japan.
An erratum to this article is available at http://dx.doi.org/10.1007/BF03257356.
Rights and permissions
About this article
Cite this article
Markham, A., Benfield, P. Pergolide. CNS Drugs 7, 328–340 (1997). https://doi.org/10.2165/00023210-199707040-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00023210-199707040-00005