Abstract
Background: Cytomegalovirus (CMV) disease may occur following renal transplantation and has been shown to have health and cost consequences in this setting.
Objective: To compare the cost effectiveness of different CMV management strategies for renal transplant patients: prophylaxis with (i) oral valaciclovir or (ii) intravenous ganciclovir; viral testing for CMV followed by (iii) pre-emptive therapy with intravenous ganciclovir or (iv) adjustment of immunosuppression and intensive monitoring; or (v) waiting to treat when CMV disease develops.
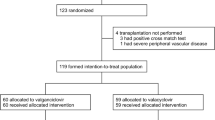
Methods: A decision-tree model was constructed that included the different management strategies for the donor seropositive/recipient seronegative (D+R−) population. Clinical outcomes for the D+R− population came from clinical trials. Treatment algorithms and costs for CMV syndrome and tissue invasive disease were developed from published literature and UK physician interviews. One- and 2-way sensitivity analyses were performed.
Study Perspective: UK National Health Service.
Results: Prophylaxis with either oral valaciclovir or intravenous ganciclovir dominated (lower costs and fewer cases of CMV disease) the pre-emptive treatment and wait-and-treat strategies. The cost per patient was from £157 to £438 higher with oral valaciclovir prophylaxis compared with intravenous ganciclovir prophylaxis and the incremental cost per case of CMV disease avoided with valaciclovir prophylaxis ranged from £2243 to £8111 (1996 values). These results are sensitive to the efficacy of intravenous ganciclovir prophylaxis and CMV management costs.
Conclusions: For D+R− renal transplant patients, prophylaxis is the dominant (more effective and less costly) management strategy compared with pre-emptive and wait-and-treat strategies. The cost per patient with oral valaciclovir prophylaxis compared with intravenous ganciclovir prophylaxis is slightly higher in our base case scenario, but may be lower under reasonable alternative assumptions.











Similar content being viewed by others
References
Hibberd P, Snydman D. Cytomegalovirus infection in organ transplant recipients. Infect Transplant 1995; 9: 863–77
Snydman D, Rubin R, Werner B. New developments in cytomegalovirus prevention and management. Am J Kidney Dis 1993; 21: 217–28
Griffiths P. Current management of cytomegalovirus disease. J Med Virol Suppl 1993; 1: 106–11
Conti D, Freed B, Gruber S, et al. Prophylaxis of primary cytomegalovirus disease in renal transplant recipients: a trial of ganciclovir vs immunoglobulin. Arch Surg 1994; 129: 443–7
Conti D, Freed B, Singh T, et al. Preemptive ganciclovir therapy in cytomegalovirus-seropositive renal transplant recipients. Arch Surg 1995; 130: 1217–22
Reusser P. Human cytomegalovirus infection and disease after bone marrow and solid organ transplantation. Baillieres Clin Infect Dis 1996; 3: 357–71
Ljungman P. Cytomegalovirus pneumonia: presentation, diagnosis, and treatment. Semin Respir Infect 1995; 10: 209–15
Rubin R. Impact of cytomegalovirus infection on organ transplant recipients. Rev Infect Dis 1990; 12 Suppl. 7: S754-S766
Tenschert W, Dittmer R, Harfmann P, et al. Vascular rejection of renal allografts is linked to CMV IgG, positive organ donor. Transplant Proc 1991; 23: 2641–2
Pouteil-Noble C, Ecochard R, Landrivon G, et al. Cytomegalovirus infection - an etiological factor for rejection? A prospective study in 242 renal transplant patients. Transplantation 1993; 55: 851–7
Gulanikar A, MacDonald A, Sungurtekin U, et al. The incidence and impact of early rejection episodes on graft outcome in recipients of first cadaver transplants. Transplantation 1992; 53 (2): 323–8
Almond P, Matas A, Gillingham K, et al. Risk factors for chronic rejection in renal allograft recipients. Transplantation 1993; 55: 752–7
Matas A, Gillingham K, Payne W, et al. The impact of an acute rejection episode on long-term renal allograft survival. Transplantation 1994; 57 Suppl. 6: 857–9
Lehtonen S, Isoniemi H, Salmela K, et al. Long-term graft outcome is not necessarily affected by delayed onset of graft function and early acute rejection. Transplantation 1994; 64: 103–7
Ho M. Virus infections after transplantation in man: brief review. Arch Virol 1997; 55: 1–24
Kontoyiannis D, Rubin R. Infection in the organ transplant recipient: an overview. Infect Dis Clin North Am 1995; 9: 811–22
Arend S, Westendorp R, Kroon F, et al. Rejection treatment and cytomegalovirus infection as risk factors for Pneumocystis carinii pneumonia in renal transplant recipients. Clin Infect Dis 1996; 22: 920–5
Tsevat J, Snydman D, Pauker S, et al. Which renal transplant patients should receive cytomegalovirus immune globulin? Transplantation 1991; 52: 259–65
McCarthy J, Karim M, Krueger H, et al. The cost impact of cytomegalovirus disease in renal transplant recipients. Transplantation 1993; 55: 1277–82
Snydman D, Werner B, Heinze-Lacey B, et al. Use of cytomegalovirus immune globulin to prevent cytomegalovirus disease in renal-transplant recipients. N Engl J Med 1987; 317: 1049–54
Balfour H, Chace B, Stapleton J, et al. A randomized, placebo controlled trial of oral acyclovir for the prevention of cytomegalovirus disease in recipients of renal allografts. N Engl J Med 1989; 320: 1381–7
Rondeau E, Bourgeon B, Peraldi M, et al. Effect of prophylactic ganciclovir on cytomegalovirus infection in renal transplant recipients. Nephrol Dial Transplant 1993; 8: 858–62
Dunn D, Glillingham K, Kramer M, et al. A prospective randomized study of acyclovir versus ganciclovir plus human immune globulin prophylaxis of cytomegalovirus infection after solid organ transplantation. Transplantation 1994; 57: 876–84
Leray H, Mourad G, Chong G, et al. Prophylactic treatment of cytomegalovirus primary infection with ganciclovir in renal transplant recipients. Transplant Proc 1995; 27: 2448
Kuypers D, Vanrenterghem Y. Prophylaxis of cytomegalovirus infection in renal transplantation. Nephrol Dial Transplant 1998; 13: 3012–6
Nicholson M, Veitch P, Donnelly P, et al. Treatment of renal transplant-associated cytomegalovirus infection with ganciclovir. Transplant Proc 1990; 22: 1811–2
De Koning J, van Dorp W, van Es L, et al. Ganciclovir effectively treats cytomegalovirus disease after solid-organ transplantation, even during rejection treatment. Nephrol Dial Transplant 1992; 7: 350–6
Lowance D, Neumayer HH, Legendre C, et al. Valacyclovir for the prevention of cytomegalovirus disease after renal transplantation. N Engl J Med 1999; 340: 1462–70
British Medical Association and the Royal Pharmaceutical Society of Great Britain. British national formulary. 31st ed. Wallingford: Pharmaceutical Press, 1996
Wakerly L, Craig A, Malek M, et al. Fluconazole versus oral polyenes in the prophylaxis of immunocompromised patients: a cost-minimization analysis. J Hosp Infect 1996; 33: 35–48
Young L, Koda-Kimble A, Kradjan W, et al. Applied therapeutics: the clinical use of drugs. Vancouver (WA): Applied Therapeutics, Inc., 1995
Rondeau E, Farquet C, Ruedin P, et al. Efficacy of early treatment of cytomegalovirus infection by ganciclovir in renal transplant recipients. Transplant Proc 1990; 22: 1813–4
Brennan D, Garlock K, Lippmann B, et al. Control of cytomegalovirus- associated morbidity in renal transplant patients using intensive monitoring and either preemptive or deferred therapy. J Am Soc Nephrol 1997; 8: 118–25
Pouteil-Noble C, Megas F, Chapuis F, et al. Cytomegalovirus prophylaxis by ganciclovir followed by high-dose acyclovir in renal transplantation: a randomized controlled trial. Transplant Proc 1996; 28: 2811
Couchoud C, Cucherat M, Haugh M, et al. Cytomegalovirus prophylaxis with antiviral agents in solid organ transplantation. Transplantation 1998; 65: 641–7
Conti D, Isenberg A, Shen G, et al. Failure of ganciclovir prophylaxis of primary cytomegalovirus disease in immunologic high-risk recipients. Transplant Proc 1998; 30: 1314–5
Johnson E, Sullivan S, Mozaffari E, et al. A utility assessment of oral and intravenous ganciclovir for the maintenance treatment of AIDS-related cytomegalovirus retinitis. Pharmacoeconomics 1996; 10 (6): 623–9
Revicki D, Simpson K, Wu A, et al. Evaluating the quality of life associated with rifabutin prophylaxis for Mycobacterium avium complex in persons with AIDS: combining Q-Twist and multiattribute utility techniques. Qual Life Res 1995; 4: 309–18
Ahsan N, Holman M, Yang H. Efficacy of oral ganciclovir in prevention of cytomegalovirus infection in post-kidney transplant patients. Clin Transplant 1997; 11: 633–9
Ahsan N, Holman M, Sonderbye L, et al. Oral ganciclovir in the prevention of cytomegalovirus infection in post kidney transplant ‘CMV at risk’ recipients: a controlled, comparative study of two regimens (750 mg bid and 500 mg bid). Transplant Proc 1998; 30: 1383–5
Brennan D, Garlock K, Singer G, et al. Prophylactic oral ganciclovir compared with deferred therapy for control of cytomegalovirus in renal transplant recipients. Transplantation 1997; 64: 1843–6
Acknowledgements
Glaxo Wellcome provided funds to Research Triangle Institute and to HEDM Research and Consulting for model development and paper preparation. Dr Maclaine was an employee at Glaxo Wellcome Research & Development, Greenford, England, at the time that the paper was written.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mauskopf, J.A., Richter, A., Annemans, L. et al. Cost-Effectiveness Model of Cytomegalovirus Management Strategies in Renal Transplantation. Pharmacoeconomics 18, 239–251 (2000). https://doi.org/10.2165/00019053-200018030-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-200018030-00004