Abstract
Background and objective: Recent reports have described cases of telithromycin-related hepatotoxicity. The objective of this study is to quantify the effect of telithromycin use on the risk of hepatotoxicity.
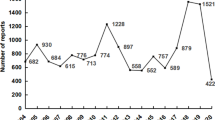
Methods: We conducted a spontaneous-report case-control study of hepatotoxicity in telithromycin recipients using reports from the US FDA Adverse Event Reporting System. Reports from between 1 January 2005 and 30 June 2005 were examined. Cases included reports of patients with abnormal liver function tests, hepatocellular damage and hepatic impairment, while patients with reported conditions with similar reporting probabilities were considered as controls. The primary outcome measure of the analysis was the reporting odds ratio (ROR) evaluating the a priori hypothesis that telithromycin use confers an elevated risk of hepatotoxicity relative to other agents.
Results: A total of 2219 cases and 20 667 controls were identified. We estimated an ROR for hepatotoxicity associated with telithromycin compared with other agents of 1.82 (95% CI 1.12, 2.96) after controlling for age and gender, approximating an 82% excess risk in users of telithromycin relative to users of other agents.
Conclusions: This analysis is the first to specifically quantify the effect of telithromycin on the risk of hepatotoxicity. Telithromycin use may increase the risk of hepatotoxicity by >80%. Biases inherent in spontaneous reports include under-reporting of events and differential or time-varying reporting due to enhanced clinician awareness. Future studies should employ alternative data sources because of the inherent limitations of passive surveillance systems.


Similar content being viewed by others
References
Ketek (telithromycin) [product information]. Kansas City (MO): Aventis Pharmaceuticals, Inc., 2006 Jun
File TM. Telithromycin new product overview. J Allergy Clin Immunol 2005 Feb; 115(2): 361–70
US Food and Drug Administration. FDA completes safety assessment of Ketek new safety information to be added to product labeling, 2006 [online]. Available from URL: http://www.fda.gov/bbs/topics/NEWS/2006/NEW01401.html [Accessed 2006 Jul 10]
Clay KD, Hanson JS, Pope SD, et al. Brief Communication: severe hepatotoxicity of telithromycin: three case reports and literature review. Ann Intern Med 2006 Mar; 144(6): 415–20
Westphal JF, Vetter D, Brogard JM. Hepatic side-effects of antibiotics. J Antimicrob Chemother 1994; 33(3): 387–401
Rothman KJ, Lanes S, Sacks ST. The reporting odds ratio and its advantages over the proportional reporting ratio. Pharmacoepidemiol Drug Saf 2004 Aug; 13(8): 519–23
Tellier G, Brunton SA, Nusrat R. Telithromycin for the treatment of acute bacterial maxillary sinusitis: a review of a new antibacterial agent. South Med J 2005 Sep; 98(9): 863–7
Buchanan PP, Stephens TA, Leroy B. A comparison of the efficacy of telithromycin versus cefuroxime axetil in the treatment of acute bacterial maxillary sinusitis. Am J Rhinol 2003; 17: 369–77
Ferguson BL, Guzzetta RV, Spector S, et al. Efficacy and safety of oral telithromycin once daily for 5 days versus moxifloxacin once daily for 10 days in the treatment of acute bacterial rhinosinusitis. Otolaryngol Head Neck Surg 2004; 131(3): 207–14
Fogarty C, de Wet R, Mandell L, et al. Five-day telithromycin once daily is as effective as 10-day clarithromycin twice daily for the treatment of acute exacerbations of chronic bronchitis and is associated with reduced health-care resource utilization. Chest 2005 Oct; 128(4): 1980–8
Hagberg L, Torres A, van Rensburg D, et al. Efficacy and tolerability of once-daily telithromycin compared with high-dose amoxicillin for treatment of community-acquired pneumonia. Infection 2002; 30(6): 378–86
Johnston SL, Blasi F, Black PN, et al. The effect of telithromycin in acute exacerbations of asthma. N Engl J Med 2006 Apr; 354(15): 1589–600
Luterman M, Tellier G, Lasko B, et al. Efficacy and tolerability of telithromycin for 5 or 10 days vs amoxicillin/clavulanic acid for 10 days in acute maxillary sinusitis. Ear Nose Throat J 2003 Aug; 82(8): 576–590
Mathers Dunbar L, Hassman J, Tellier G. Efficacy and tolerability of once-daily oral telithromycin compared with clarithromycin for the treatment of community-acquired pneumonia in adults. Clin Ther 2004; 26(1): 48–62
Tellier G, Niederman MS, Nusrat R, et al. Clinical and bacteriological efficacy and safety of 5 and 7 day regimens of telithromycin once daily compared with a 10 day regimen of clarithromycin twice daily in patients with mild to moderate community-acquired pneumonia. J Antimicrob Chemother 2004 Aug; 54(2): 515–23
Brown EG, Wood L, Wood S. The medical dictionary for regulatory activities (MedDRA). Drug Saf 1999 Feb; 20(2): 109–17
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 1959 Apr; 22(4): 719–48
Pringle E [IMS Health]. Scoop Independent News. Lawmakers demand answers about Ketek from FDA, 2006 [online]. Available from URL: http://www.scoop.co.nz/stories/HL0606/S00279.htm [Accessed 2006 Jul 10]
Ostapowicz G, Fontana RJ, Schiodt FV, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med 2002 Dec; 137(12): 947–54
Ruhl CE, Everhart JE. Joint effects of body weight and alcohol on elevated serum alanine aminotransferase in the United States population. Clin Gastroenterol Hepatol 2005 Dec; 3(12): 1260–8
Grant BF, Dawson DA, Stinson FS, et al. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend 2004 Jun; 74(3): 223–34
Moore AA, Gould R, Reuben DB, et al. Longitudinal patterns and predictors of alcohol consumption in the United States. Am J Public Health 2005 Mar; 95(3): 458–65
Cox ER, Frisse M, Behm A, et al. Over-the-counter pain reliever and aspirin use within a sample of long-term cyclooxygenase 2 users. Arch Intern Med 2004 Jun; 164(11): 1243–6
Rehm J, Room R, Graham K, et al. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction 2003 Sep; 98(9): 1209–28
Graham DJ, Drinkard CR, Shatin D, et al. Liver enzyme monitoring in patients treated with troglitazone. JAMA 2001 Aug; 286(7): 831–3
Smalley WD, Shatin D, Wysowski DK, et al. Contraindicated use of cisapride: impact of Food and Drug Administration regulatory action. JAMA 2000 Dec; 284(23): 3036–9
Mazor KM, Andrade SE, Auger J, et al. Communicating safety information to physicians: an examination of dear doctor letters. Pharmacoepidemiol Drug Saf 2005 Dec; 14(12): 869–75
Goldman SA. Limitations and strengths of spontaneous reports data. Clin Ther 1998; 20 Suppl. C: 40–4
Acknowledgements
This work was supported by an institutional postdoctoral training grant (T32) from the Agency for Health Care Research and Quality (Dr Dore). The funding source played no role in the design, conduct or reporting of this study.
Dr Dore receives consultancy fees from Pfizer Inc. for work independent of Brown Medical School. This arrangement with Pfizer played no role in the design, conduct or reporting of this study. Dr Lapane was the principal investigator and has received a grant from Pfizer Inc., which was used entirely to train doctoral students interested in pharmacoepidemiology. Mrs DiBello has no conflicts of interest that are directly relevant to the content of this article. No other individuals contributed to this study.
These data were presented in abstract form (poster) at the International Conference on Pharmacoepidemiology (ICPE), Lisbon, Portugal; August 2006.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dore, D.D., DiBello, J.R. & Lapane, K.L. Telithromycin Use and Spontaneous Reports of Hepatotoxicity. Drug-Safety 30, 697–703 (2007). https://doi.org/10.2165/00002018-200730080-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200730080-00006