Abstract
Background: Selective serotonin reuptake inhibitors (SSRIs) and serotoninnoradrenaline reuptake inhibitors (SNRIs) are approved for the treatment of major depressive disorder (MDD). The allosteric SSRI escitalopram has been shown to be at least as clinically effective as the SNRIs venlafaxine and duloxetine in MDD, with a better tolerability profile. In addition, escitalopram has been shown to be cost saving compared with venlafaxine.
Objective: To evaluate the cost effectiveness of escitalopram versus duloxetine in the treatment of MDD, and to identify key cost drivers.
Methods: The pharmacoeconomic evaluation was conducted alongside a 24-week, double-blind, multinational randomized study (escitalopram 20 mg/day and duloxetine 60 mg/day) in outpatients with MDD, aged 18–65 years, with Montgomery-Åsberg Depression Rating Scale (MADRS) score ≥26 and Clinical Global Impression Severity (CGI-S) score ≥4, and baseline duration of the current depressive episode of 12 weeks to 1 year.
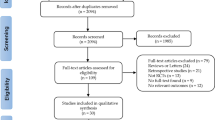
The analysis was conducted on the full analysis set (FAS), which included all patients with ≥1 valid post-baseline health economic assessment. Effectiveness outcomes of the cost-effectiveness analyses (CEA) included the change in Sheehan Disability Scale (SDS) score (primary CEA), treatment response (MADRS score decrease ≥50%) and remission (MADRS score ≤12) rates at week 24. Cost outcomes were assessed from the societal perspective. Healthcare resource use and sick leave were evaluated using a health economic assessment questionnaire. Unit costs of healthcare services were obtained from standard UK sources (£, year 2006 values).
Results: Over the total 24-week study period, escitalopram was associated with significant cost savings compared with duloxetine (total per-patient monthly cost £188 vs £334, respectively). In the primary CEA, escitalopram dominated duloxetine (i.e. was more effective on the disability scale and less costly). Treatment with escitalopram resulted in significantly lower mean sick leave duration per patient over 24 weeks than duloxetine (30.7 days vs 62.2 days).
In multivariate analyses, escitalopram as a treatment choice was associated with a 54% reduction in sick leave duration (p < 0.001). Treatment with escitalopram also resulted in 49% lower total costs than treatment with duloxetine (p = 0.002). Absenteeism accounted for about two-thirds of the overall cost. Early clinical improvement (mean change in MADRS total score, response and remission) had an independent significant impact on the sick leave duration, after controlling for key co-variates.
Conclusions: Escitalopram was associated with significantly lower duration of sick leave and significant savings in the total cost compared with duloxetine; it dominated duloxetine when effectiveness was assessed on the SDS scale. Indirect costs due to sick leave accounted for the most substantial portion of the total cost and should, therefore, be an important consideration when pharmacoeconomic comparisons between treatments are made from the societal perspective. The link between decrease in absenteeism and early (8-week) clinical improvement suggested in the additional analyses may explain the reduced sick leave observed with escitalopram, given its superior short-term efficacy compared with duloxetine (demonstrated in the underlying clinical trial).










Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
For a visit to a psychiatrist, the unit cost was lowered to £123 excluding qualification considerations. For other specialists, unit costs of visits were lowered to estimates corresponding to follow-up visits (vs first-attendance unit cost applied in the base case) and amounted to £103 (cardiologist), £64 (dermatologist), £69 (ENT specialist) and £96 (gastroenterologist).
Although the numerical difference between treatment groups is high, it did not reach statistical significance. This is probably due to the small number of patients in comparison groups (e.g. at week 24, only seven patients with sick leave were identified in the escitalopram group).
References
Sonawalla SB, Fava M. Severe depression: is there a best approach? CNS Drugs 2001; 15 (10): 765–76
Thase ME. Treatment of severe depression. J Clin Psychiatry 2000; 61 Suppl. 1: 17–25
Murray CJ, Lopez AD. Evidence-based health policy: lessons from the Global Burden of Disease Study. Science 1996 Nov 1; 274 (5288): 740–3
Lepine JP, Gastpar M, Mendlewicz J, et al. Depression in the community: the first pan-European study DEPRES (Depression Research in European Society). Int Clin Psychopharmacol 1997 Jan; 12 (1): 19–29
Kessler RC, Akiskal HS, Ames M, et al. Prevalence and effects of mood disorders on work performance in a nationally representative sample of US workers. Am J Psychiatry 2006 Sep; 163 (9): 1561–8
Ferrier IN. Treatment of major depression: is improvement enough? J Clin Psychiatry 1999; 60 Suppl. 6: 10–4
Frampton JE, Plosker GL. Duloxetine: a review of its use in the treatment of major depressive disorder. CNS Drugs 2007; 21 (7): 581–609
Sir A, D’Souza RF, Uguz S, et al. Randomized trial of sertraline versus venlafaxine XR in major depression: efficacy and discontinuation symptoms. J Clin Psychiatry 2005 Oct; 66 (10): 1312–20
Owens MJ, Knight DL, Nemeroff CB. Second-generation SSRIs: human monoamine transporter binding profile of escitalopram and R-fluoxetine. Biol Psychiatry 2001 Sep 1; 50 (5): 345–50
Azorin JM, Llorca PM, Despiegel N, et al. Escitalopram is more effective than citalopram for the treatment of severe major depressive disorder [in French]. Encephale 2004 Mar-Apr; 30 (2): 158–66
Murdoch D, Keam SJ. Escitalopram: a review of its use in the management of major depressive disorder. Drugs 2005; 65 (16): 2379–404
Sanchez C. The pharmacology of citalopram enantiomers: the antagonism by R-citalopram on the effect of S-citalopram. Basic Clin Pharmacol Toxicol 2006 Aug; 99 (2): 91–5
Moore N, Verdoux H, Fantino B. Prospective, multicentre, randomized, double-blind study of the efficacy of escitalopram versus citalopram in outpatient treatment of major depressive disorder. Int Clin Psychopharmacol 2005 May; 20 (3): 131–7
Boulenger JP, Huusom AK, Florea I, et al. A comparative study of the efficacy of long-term treatment with escitalopram and paroxetine in severely depressed patients. Curr Med Res Opin 2006 Jul; 22 (7): 1331–41
Yevtushenko VY, Belous AI, Yevtushenko YG, et al. Efficacy and tolerability of escitalopram versus citalopram in major depressive disorder: a 6-week, multicenter, prospective, randomized, double-blind, active-controlled study in adult outpatients. Clin Ther 2007 Nov; 29 (11): 2319–32
Montgomery SA, Huusom AK, Bothmer J. A randomised study comparing escitalopram with venlafaxine XR in primary care patients with major depressive disorder. Neuropsychobiology 2004; 50 (1): 57–64
Khan A, Bose A, Alexopoulos GS, et al. Double-blind comparison of escitalopram and duloxetine in the acute treatment of major depressive disorder. Clin Drug Investig 2007; 27 (7): 481–92
Wade A, Gembert K, Florea I. A comparative study of the efficacy of acute and continuation treatment with escitalopram versus duloxetine in patients with major depressive disorder. Curr Med Res Opin 2007 Jul; 23 (7): 1605–14
Montgomery SA, Andersen HF. Escitalopram versus venlafaxine XR in the treatment of depression. Int Clin Psychopharmacol 2006 Sep; 21 (5): 297–309
Bielski RJ, Ventura D, Chang CC. A double-blind comparison of escitalopram and venlafaxine extended release in the treatment of major depressive disorder. J Clin Psychiatry 2004 Sep; 65 (9): 1190–6
Llorca PM, Fernandez JL. Escitalopram in the treatment of major depressive disorder: clinical efficacy, tolerability and cost-effectiveness vs venlafaxine extended-release formulation. Int J Clin Pract 2007 Apr; 61 (4): 702–10
Croom KF, Plosker GL. Escitalopram: a pharmacoeconomic review of its use in depression. Pharmacoeconomics 2003; 21 (16): 1185–209
Fernandez JL, Montgomery S, Francois C. Evaluation of the cost effectiveness of escitalopram versus venlafaxine XR in major depressive disorder. Pharmacoeconomics 2005; 23 (2): 155–67
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed [text revision] (DSM-IV-TR). Washington, DC: American Psychiatric Publishing, Inc., 1994
Sobocki P, Ekman M, Agren H, et al. Health-related quality of life measured with EQ-5D in patients treated for depression in primary care. Value Health 2007 Mar-Apr; 10 (2): 153–60
Steel RGD, Torrie JH. Principles and procedures of statistics: a biometrical approach. 2nd ed. New York: McGraw-Hill Book Company, 1980
Personal Social Services Research Unit (PSSRU). Unit costs of health and social care. Canterbury (UK): University of Kent, 2006
UK Department of Health; National Health Service. Reference costs 2006 collection: guidance[online]. Available from URL: http://www.dh.gov.uk [Accessed 2007 Feb 23]
Wonderling D, Vickers AJ, Grieve R, et al. Cost effectiveness analysis of a randomised trial of acupuncture for chronic headache in primary care. BMJ 2004 Mar 27; 328 (7442): 747
National Statistics. First release: 2006 annual survey of hours and earnings. 2006 Oct 26[online]. Available from URL: http://www.statistics.gov.uk/pdfdir/ashe1006.pdf [Accessed 2008 Jan 30]
Ramsey S, Willke R, Briggs A, et al. Good research practices for cost-effectiveness analysis alongside clinical trials: the ISPOR RCT-CEA Task Force report. Value Health 2005 Sep-Oct; 8 (5): 521–33
Netten A, Rees T, Harrison G. Unit costs of health and social care 2001[online]. Available from URL: http://www.pssru.ac.uk/pdf/UC2001/UnitCosts2001ALL.pdf [Accessed 2008 Mar 5]
Wang PS, Simon G, Kessler RC. The economic burden of depression and the cost-effectiveness of treatment. Int J Methods Psychiatr Res 2003; 12 (1): 22–33
Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ 2001 Jul; 20 (4): 461–94
Briggs A, Fenn P. Confidence intervals or surfaces? Uncertainty on the cost-effectiveness plane. Health Econ 1998 Dec; 7 (8): 723–40
van Hout BA, Al MJ, Gordon GS, et al. Costs, effects and C/E-ratios alongside a clinical trial. Health Econ 1994 Sep-Oct; 3 (5): 309–19
Efron B, Tibshirani RJ. An introduction to the bootstrap. New York: Hall & Chapman, 1993
Greenberg PE, Stiglin LE, Finkelstein SN, et al. The economic burden of depression in 1990. J Clin Psychiatry 1993 Nov; 54 (11): 405–18
Winkler D, Pjrek E, Moser U, et al. Escitalopram in a working population: results from an observational study of 2378 outpatients in Austria. Hum Psychopharmacol 2007 Jun; 22 (4): 245–51
Wittchen HU, Kessler RC, Beesdo K, et al. Generalized anxiety and depression in primary care: prevalence, recognition, and management. J Clin Psychiatry 2002; 63 Suppl. 8: 24–34
Moller H-J, Langer S, Schmauß M. Escitalopram in clinical practice: results of an open-label trial in outpatients with depression in a naturalistic setting in Germany. Pharmacopsychiatry 2007; 40: 53–7
Wimo A, Winblad B, Engedal K, et al. An economic evaluation of donepezil in mild to moderate Alzheimer’s disease: results of a 1-year, double-blind, randomized trial. Dement Geriatr Cogn Disord 2003; 15 (1): 44–54
Sculpher MJ, Poole L, Cleland J, et al. Low doses vs high doses of the angiotensin converting-enzyme inhibitor lisinopril in chronic heart failure: a cost-effectiveness analysis based on the Assessment of Treatment with Lisinopril and Survival (ATLAS) study. The ATLAS Study Group. Eur J Heart Fail 2000 Dec; 2 (4): 447–54
Caro JJ, Getsios D, Raggio G, et al. Treatment of migraine in Canada with naratriptan: a cost-effectiveness analysis. Headache 2001 May; 41 (5): 456–64
Drummond MF, Becker DL, Hux M, et al. An economic evaluation of sequential i.v./po moxifloxacin therapy compared to i.v./po co-amoxiclav with or without clarithromycin in the treatment of community-acquired pneumonia. Chest 2003 Aug; 124 (2): 526–35
Legendre CM, Norman DJ, Keating MR, et al. Valaciclovir prophylaxis of cytomegalovirus infection and disease in renal transplantation: an economic evaluation. Transplantation 2000 Nov 27; 70 (10): 1463–8
Ekman M, Zethraeus N, Jonsson B. Cost effectiveness of bisoprolol in the treatment of chronic congestive heart failure in Sweden: analysis using data from the Cardiac Insufficiency Bisoprolol Study II trial. Pharmacoeconomics 2001; 19 (9): 901–16
Manca A, Willan AR. ‘Lost in translation’: accounting for between-country differences in the analysis of multinational cost-effectiveness data. Pharmacoeconomics 2006; 24 (11): 1101–19
Greenberg PE, Kessler RC, Birnbaum HG, et al. The economic burden of depression in the United States: how did it change between 1990 and 2000. J Clin Psychiatry 2003; 64 (12): 1465–75
Acknowledgements
This study was supported by funding from H. Lundbeck A/S.
The authors would like to thank Natalie Barker of Wolters Kluwer Health for her assistance with writing the manuscript.
Alan G. Wade has received honoraria from H. Lundbeck A/S and grants from H. Lundbeck A/S for clinical trial participation. He has also acted for H. Lundbeck A/S and Eli Lilly as a researcher and member of advisory boards.
José-Luis Fernández has received consultancy fees from H. Lundbeck A/S for pharmaceutical research.
Clément François, Karina Hansen, Natalya Danchenko and Nicolas Despiegel are employees of H. Lundbeck A/S.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Wade, A.G., Fernández, JL., François, C. et al. Escitalopram and Duloxetine in Major Depressive Disorder. Pharmacoeconomics 26, 969–981 (2008). https://doi.org/10.2165/00019053-200826110-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-200826110-00008