Abstract
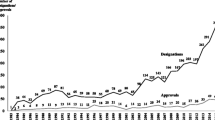
An orphan disease is a disease with a very low prevalence. Although there are 5000–7000 orphan diseases, only 50 orphan drugs (i.e. drugs developed to treat orphan diseases) were marketed in the EU by the end of 2008. In 2000, the EU implemented policies specifically designed to stimulate the development of orphan drugs. While decisions on orphan designation and the marketing authorization of orphan drugs are made at the EU level, decisions on drug reimbursement are made at the member state level. The specific features of orphan diseases and orphan drugs make them a high-priority issue for policy makers.
The aim of this article is to identify and discuss several issues surrounding orphan disease and drug policies in Europe.
The present system of orphan designation allows for drugs for non-orphan diseases to be designated as orphan drugs. The economic factors underlying orphan designation can be questioned in some cases, as a low prevalence of a certain indication does not equal a low return on investment for the drug across its indications. High-quality evidence about the clinical added value of orphan drugs is rarely available at the time of marketing authorization, due to the low number of patients. A balance must be struck between ethical and economic concerns. To this effect, there is a need to initiate a societal dialogue on this issue, to clarify what society wants and accepts in terms of ethical and economic consequences. The growing budgetary impact of orphan drugs puts pressure on drug expenditure. Indications can be extended for an orphan drug and the total prevalence across indications is not considered. Finally, cooperation needs to be fostered in the EU, particularly through a standardized approach to the creation and use of registries.
These issues require further attention from researchers, policy makers, health professionals, patients, pharmaceutical companies and other stakeholders with a view to optimizing orphan disease and drug policies in Europe.
Similar content being viewed by others
Notes
Orphan designation refers to the award of orphan status to a drug, while marketing authorization refers to the approval to market the drug.[1]
References
European Commission. European Commission Regulation (EC) no. 141/2000 of the European Parliament and the Council of 16 December 1999 on orphan medicinal products. Official Journal of the European Communities 2000; L18/1 [online]. Available from URL: http://ec.europa.eu/health/files/eudralex/vol-1/reg_2000_141/reg_2000_141_en.pdf [Accessed 2010 Jun 30]
European Medicines Agency. Annual report of the European Medicines Agency 2007. London: European Medicines Agency, 2008
Denis A, Simoens S, Fostier C, et al. Health technology assessment policy governing orphan diseases and orphan medicines. Brussels: Belgian Health Care Knowledge Centre, 2009
Yin W. R&D policy, agency costs and innovation in personalized medicine. J Health Econ 2009; 28: 950–62
European Medicines Agency. COMP report to the Commission in relation to article 10 of regulation 141 /2000 on orphan medicinal products. London: European Medicines Agency, 2007
Dear JW, Lilitkarntakul P, Webb DJ. Are rare diseases still orphans or happily adopted? The challenges of developing and using orphan medicinal products. Br J Clin Pharmacol 2006; 62: 264–71
European Medicines Evaluation Agency. Committee for Orphan Medicinal Products (COMP) [online]. Available from URL: http://www.ema.europa.eu/htms/general/contacts/COMP/COMP.html [Accessed 2009 Nov 24]
Sheridan C. EU to review rare disease drugs market exclusivity [letter]. Nat Biotechnol 2004; 22(9): 1061
European Medicines Agency. Committee for Medicinal Products for Human Use post-authorisation summary of positive opinion for Revatio. London: European Medicines Agency, 2009
European Medicines Agency. Committee for Medicinal Products for Human Use (CHMP). Guideline on clinical trials in small populations [online]. Available from URL: http://www.ema.europa.eu/pdfs/human/ewp/8356105en.pdf [Accessed 2009 Nov 24]
European Organisation for Rare Diseases. EURORDIS position paper on the ‘centralised procedure for the scientific assessment of the therapeutic added value of orphan drugs’ [online]. Available from URL: http://www.eurordis.org/IMG/pdf/position-paper-EURORDIS-therapeutic-added-value-ODFeb08.pdf [Accessed 2009 Nov 23]
The Pharmaceutical Forum. Improving access to orphan medicines for all affected EU citizens [online]. Available from URL: http://ec.europa.eu/pharmaforum/docs/pricing_orphans_en.pdf [Accessed 2009 Nov 16]
Cleemput I, Neyt M, Thiry N, et al. Cost-effectiveness thresholds in health care. Brussels: Belgian Healthcare Knowledge Centre, 2008
Drummond M, Evans B, LeLorier J, et al. Evidence and values: requirements for public reimbursement of drugs for rare diseases — a case study in oncology. Can J Clin Pharmacol 2009; 16: e273–81
Gericke CA, Riesberg A, Busse R. Ethical issues in funding orphan drug research and development. J Med Ethics 2005; 31: 164–8
Littlejohns P, Garner S, Doyle N, et al. 10 years of NICE: still growing and still controversial. Lancet Oncol 2009; 10: 417–24
Connock M, Juarez-Garcia A, Frew E, et al. A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1. Health Technol Assess 2006; 10: iii–113
Heemstra HE, de Vrueh RL, van WS, et al. Orphan drug development across Europe: bottlenecks and opportunities. Drug Discov Today 2008; 13: 670–6
Schlander M, Beck M. Expensive drugs for rare disorders: to treat or not to treat? The case of enzyme replacement therapy for mucopolysaccharidosis VI. Curr Med Res Opin 2009; 25: 1285–93
Cook JP, Vernon JA, Manning R. Pharmaceutical risk-sharing agreements. Pharmacoeconomics 2008; 26(7): 551–6
Orofino J, Soto J, Casado MA, et al. Global spending on orphan drugs in France, Germany, the UK, Italy and Spain during 2007. Appl Health Econ Health Policy 2010; 8(5): 301–15
McCabe C, Tsuchiya A, Claxton K, et al. Orphan drugs revisited. QJM 2006; 99: 341–5
Rinaldi A. Adopting an orphan. EMBO Rep 2005; 6(6): 507–10
Owen A, Sprinks J, Meehan A, et al. A new model to evaluate the long-term cost effectiveness of orphan and highly specialised drugs following listing on the Australian Pharmaceutical Benefits Scheme: the Bosentan Patient Registry. J Med Econ 2008; 11: 235–43
Italian Medicines Agency. Post-marketing surveillance programme [online]. Available from URL: http://monitoraggio-farmaci.agenziafarmaco.it [Accessed 2010 Feb 16]
Acknowledgements
Financial support for this research was received from the Belgian Health Care Knowledge Centre, a state-funded research institution. The authors have no conflicts of interest that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Denis, A., Mergaert, L., Fostier, C. et al. Issues surrounding orphan disease and orphan drug policies in Europe. Appl Health Econ Health Policy 8, 343–350 (2010). https://doi.org/10.2165/11536990-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11536990-000000000-00000