Summary
Abstract
The use of combination budesonide/formoterol dry powder inhaler (Symbicort® Turbuhaler®) for both daily maintenance therapy and as-needed relief of breakthrough symptoms using a single inhaler is a new approach to asthma management that is indicated in patients with persistent asthma not adequately controlled by conventional regimens using reliever therapy with a short-acting β2-adrenoceptor agonist alone. The administration of additional corticosteroid with each reliever inhalation in response to symptoms is expected to provide improved control of airway inflammation.
Budesonide/formoterol maintenance and reliever therapy reduced the risk of severe asthma exacerbations compared with conventional regimens using a short-acting β2-adrenoceptor agonist alone as reliever therapy in the majority of trials, while providing similar or better daily asthma control than higher fixed maintenance doses of budesonide or inhaled corticosteroid/long-acting β2-adrenoceptor agonist combination therapy in patients with generally moderate to severe, uncontrolled, persistent asthma. The strategy offers the convenience of a single inhaler and simplifies treatment by providing immediate additional anti-inflammatory medication in response to asthma symptoms and immediate step-down when symptoms abate. The improved efficacy, with respect to exacerbation prevention, observed with budesonide/formoterol maintenance and reliever therapy in all double-blind comparative trials was achieved with a lower mean daily dose of inhaled corticosteroid or with fewer daily inhalations of reliever medication. Budesonide/formoterol maintenance and reliever therapy was well tolerated with an incidence of adverse events similar to that with conventional regimens. Therefore, it offers a new approach to therapy in patients with uncontrolled, persistent asthma; providing improved efficacy with a lower overall drug load.
Pharmacological Properties
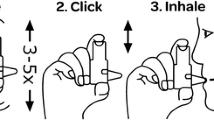
The fixed combination budesonide/formoterol Turbuhaler® delivers the same amounts of budesonide and formoterol per inhalation (80μg/4.5μg or 160μg/ 4.5μg) as the corresponding single-agent inhalers at the same nominal dose. There do not appear to be any pharmacokinetic interactions between budesonide and formoterol when administered in combination.
Budesonide is a corticosteroid with high affinity for the glucocorticoid receptor and a high ratio of topical to systemic activity. It displays anti-inflammatory activity ≈1000-fold greater than cortisol. It dose-dependently protects against bronchial hyperresponsiveness to a variety of agents, attenuates the early and late asthmatic responses to inhaled allergen and reduces other signs of airway inflammation. Budesonide is moderately lipophilic and forms reversible conjugates with intracellular fatty acids, which prolongs its retention within the airways. A mean of 27–44% of the dose delivered by Turbuhaler® is deposited in the lungs. The mean systemic bioavailability of inhaled budesonide was calculated to be 38% of the metered dose. Budesonide is rapidly absorbed after inhalation, undergoes extensive metabolism in the liver, mainly by cytochrome P450 3A4, and is eliminated, almost exclusively as metabolites, in the urine with an elimination half-life (t1/2β) of 2–4 hours. p ]Formoterol is a potent, long-acting, selective β2-adrenoceptor agonist that displays full agonist activity. It has a rapid onset of bronchodilator action (1–3 minutes) that is maintained for ≥12 hours. The mean lung deposition of formoterol after administration by Turbuhaler® is 28–49% of the delivered dose. The systemic bioavailability of inhaled formoterol is ≈61% of the delivered dose. It is extensively metabolised in the liver and eliminated in the urine with a t1/2β of ≈17 hours. Only 8–13% of the delivered dose is eliminated in the urine as unchanged drug.
Therapeutic Efficacy
Inhaled budesonide/formoterol maintenance (160μg/9μg or 320μg/9μg daily) and reliever therapy was superior to maintenance therapy with a 2- to 4-fold higher dosage of budesonide (320μg or 640μg daily) plus terbutaline reliever with respect to the primary endpoints of time to first severe exacerbation or change from baseline in morning peak expiratory flow in three randomised, double-blind trials of 6–12 months’ duration. The risk of experiencing a severe exacerbation was reduced by 39–54% with budesonide/formoterol maintenance and reliever therapy compared with the conventional therapy in these trials.
Budesonide/formoterol maintenance (160μg/9μg or 320μg/9μg daily) and reliever therapy was likewise superior to the same dosage of budesonide/ formoterol maintenance therapy combined with terbutaline or formoterol single-agent reliever therapy for the primary endpoint of time to first severe exacerbation in two randomised, double-blind, 12-month trials. Budesonide/formoterol maintenance and reliever therapy reduced the risk of a severe exacerbation by 45% compared with terbutaline reliever in both trials and by 27% compared with formoterol reliever in one trial.
In a randomised, double-blind, 6-month trial, budesonide/formoterol maintenance (320μg/9μg daily) and reliever therapy was shown to be superior to a 2-fold higher dosage of budesonide/formoterol (640μg/18μg daily) maintenance therapy combined with terbutaline reliever according to the primary endpoint of time to first severe exacerbation, reducing the risk of a severe exacerbation by 26%.
Budesonide/formoterol maintenance (320μg/9μg daily) and reliever therapy also significantly prolonged the time to first severe exacerbation compared with salmeterol/fluticasone propionate 50μg/250μg twice daily maintenance therapy plus terbutaline reliever in the aforementioned trial; budesonide/formoterol maintenance and reliever therapy reduced the risk of a severe exacerbation by 33% compared with salmeterol/fluticasone propionate. However, in another 6-month, randomised, double-blind trial, budesonide/formoterol maintenance (640μg/18μg daily) and reliever therapy displayed similar efficacy to high-dosage salmeterol/ fluticasone propionate 50μg/500μg twice daily maintenance plus terbutaline reliever for the primary endpoint of time to first severe exacerbation.
In a nonblind study in which the maintenance therapy dosages were titrated throughout treatment, budesonide/formoterol maintenance and reliever therapy was superior to salmeterol/fluticasone propionate maintenance plus salbutamol (albuterol) reliever with respect to time to first severe exacerbation and was associated with a 25% lower risk of a severe exacerbation.
In all studies, including two nonblind, real-life comparisons with conventional regimens, budesonide/formoterol maintenance and reliever therapy was consistently associated with either a reduction in daily inhaled corticosteroid dose (descriptive statistics only in some studies) or a significant reduction in the mean number of reliever inhalations per day during treatment, or both. It was also associated with greater improvements in measures of daily asthma control and lung function, and less use of oral corticosteroids than conventional regimens in most double-blind trials.
Pharmacoeconomic Considerations
In each of four cost-effectiveness analyses using clinical and resource utilisation data from one of three randomised, controlled trials and costs from a variety of countries, budesonide/formoterol maintenance and reliever therapy was consistently dominant (greater efficacy at lower cost) over both salmeterol/fluticasone propionate maintenance therapy plus salbutamol or terbutaline reliever and budesonide/formoterol maintenance plus terbutaline reliever from the societal perspective (direct plus indirect costs). When only direct healthcare costs were considered, budesonide/formoterol maintenance and reliever therapy was either dominant over the alternative treatments or delivered the increased efficacy at a relatively small incremental cost.
Tolerability
Budesonide/formoterol maintenance and reliever therapy was well tolerated in randomised, controlled clinical trials. The incidence, type and severity of adverse events were similar to those with the comparator conventional regimens. The most common adverse events were respiratory tract infection, pharyngitis, rhinitis, bronchitis, sinusitis and headache. The incidences of the pharmacologically predictable adverse events of tremor, palpitations, tachycardia, candidiasis, dysphonia and hoarseness were low (≤2%). The incidence of serious adverse events considered related to treatment was ≤0.3%, while treatment discontinuations as a result of asthma were generally numerically lower with budesonide/formoterol maintenance and reliever therapy than with the comparator conventional regimens.




Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention [online]. Available from URL: http://www.ginasthma.com [Accessed 2007 Aug 8]
British Thoracic Society. British guideline on the management of asthma: a national clinical guideline [online]. Available from URL: http://www.sign.ac.uk/pdf/sign63.pdf [Accessed 2007 Aug 8]
National Asthma Education and Prevention Program. Expert panel report 3: guidelines for the diagnosis and management of asthma. Full report 2007 [online]. Available from URL: http://www.nhlbi.nih.govf [Accessed 2007 Sep 20]
Bai TR, Vonk JM, Postma DS, et al. Severe exacerbations predict excess lung function decline in asthma. Eur Respir J 2007 Sep; 30(3): 452–6
van der Molen T, Ostrem A, Stallberg B, et al. International Primary Care Respiratory Group (IPCRG) guidelines: management of asthma. Prim Care Respir J 2006 Feb; 15(1): 35–47
O’Byrne PM, Barnes PJ, Rodriguez-Roisin R, et al. Low dose inhaled budesonide and formoterol in mild persistent asthma: the OPTIMA randomized trial. Am J Respir Crit Care Med 2001 Oct 15; 164(8): 1392–7
Pauwels RA, Löfdahl C-G, Postma DS, et al. Effect of inhaled formoterol and budesonide on exacerbations of asthma. N Engl J Med 1997 Nov 13; 337(20): 1405–11
Barnes PJ. Scientific rationale for using a single inhaler for asthma control. Eur Respir J 2007 Mar; 29(3): 587–95
Pauwels RA, Sears MR, Campbell M, et al. Formoterol as relief medication in asthma: a worldwide safety and effectiveness trial. Eur Respir J 2003 Nov; 22(5): 787–94
D’Urzo AD. Inhaled glucocorticosteroid and long-acting β2-agonist single-inhaler combination for both maintenance and rescue therapy: a paradigm shift in asthma management. Treat Respir Med 2006; 5(6): 385–91
Remington TL, DiGiovine B. Long-acting β-agonists: anti-inflammatory properties and synergy with corticosteroids in asthma. Curr Opin Pulm Med 2005 Jan; 11(1): 74–8
Brogden RN, McTavish D. Budesonide: an updated review of its pharmacological properties, and therapeutic efficacy in asthma and rhinitis. Drugs 1992; 44(3): 375–407
Hvizdos KM, Jarvis B. Budesonide inhalation suspension: a review of its use in infants, children and adults with inflammatory respiratory disorders. Drugs 2000 Nov; 60(5): 1141–78
Braga PC, Culici M, Dal Sasso M. Budesonide reduces superoxide and peroxynitrite chemiluminescence during human neutrophil bursts [abstract no. 268]. Eur Respir J 2004 Sep; 24 Suppl. 48: 21s
Symbicort® (budesonide/formoterol) 200/6 Turbohaler® inhalation powder: summary of product characteristics (UK) [online]. Available from URL: http://emc.medicines.org.uk [Accessed 2007 Jul 24]
The Childhood Asthma Management Program Research Group. Long-term effects of budesonide or nedocromil in children with asthma. N Engl J Med 2000 Oct 12; 343(15): 1054–63
Agertoft L, Pedersen S. Effect of long-term treatment with inhaled budesonide on adult height in children with asthma. N Engl J Med 2000 Oct 12; 343(15): 1064–9
Faulds D, Hollingshead LM, Goa KL. Formoterol: a review of its pharmacological properties and therapeutic potential in reversible obstructive airways disease. Drugs 1991 Jul; 42(1): 115–37
Hospenthal MAC, Peters JI. Long-acting β2-agonists in the management of asthma exacerbations. Curr Opin Pulm Med 2005 Jan; 11(1): 69–73
Goldsmith DR, Keating GM. Budesonide/formoterol: a review of its use in asthma. Drugs 2004; 64(14): 1597–618
Cheer SM, Scott LJ. Formoterol: a review of its use in chronic obstructive pulmonary disease. Am J Respir Med 2002; 1(4): 285–300
Overbeek SE, Mulder PG, Baelemans SM, et al. Formoterol added to low-dose budesonide has no additional antiinflammatory effect in asthmatic patients. Chest 2005 Sep; 128(3): 1121–7
Haahtela T, Tamminen K, Malmberg LP, et al. Formoterol as needed with or without budesonide in patients with intermittent asthma and raised NO levels in exhaled air: a SOMA study. Eur Respir J 2006 Oct; 28(4): 748–55
O’Connor TM, Kelly MM, Leigh R, et al. Additional anti-inflammatory effects of inhaled budesonide/formoterol over inhaled budesonide in subjects with atopic asthma [abstract no. P2570]. Eur Respir J 2006 Sep; 28 Suppl. 50: 441s
Korn SH, Jerre A, Brattsand R. Effects of formoterol and budesonide on GM-CSF and IL-8 secretion by triggered human bronchial epithelial cells. Eur Respir J 2001 Jun; 17(6): 1070–7
Duong M, Gauvreau G, Watson R, et al. The effects of inhaled budesonide and formoterol in combination and alone when given directly after allergen challenge. J Allergy Clin Immunol 2007 Feb; 119(2): 322–7
Wilson SJ, Wallin A, Della-Cioppa G, et al. Effects of budesonide and formoterol on NF-κB, adhesion molecules, and cytokines in asthma. Am J Respir Crit Care Med 2001 Sep 15; 164(6): 1047–52
Wallin A, Sandstrom T, Cioppa GD, et al. The effects of regular inhaled formoterol and budesonide on preformed Th-2 cytokines in mild asthmatics. Respir Med 2002 Dec; 96(12): 1021–5
Maneechotesuwan K, Essilfie-Quaye S, Meah S, et al. Formoterol attenuates neutrophilic airway inflammation in asthma. Chest 2005 Oct 1; 128(4): 1936–42
Capraz F, Kunter E, Cermik H, et al. The effect of inhaled budesonide and formoterol on bronchial remodeling and HRCT features in young asthmatics. Lung 2007 Mar; 185(2): 89–96
Boobis AR. Comparative physiochemical and pharmacokinetic profiles of inhaled beclomethasone dipropionate and budesonide. Respir Med 1998; 92 Suppl. B: 2–6
McGavin JK, Goa KL, Jarvis B. Inhaled budesonide/formoterol combination. Drugs 2001; 61(1): 71–8
Newman SP, Pitcairn GR, Hirst PH, et al. Scintigraphic comparison of budesonide deposition from two dry powder inhalers. Eur Respir J 2000 Jul; 16(1): 178–83
Thorsson L, Edsbäcker S, Conradson T-B. Lung deposition of budesonide from Turbuhaler® is twice that from a pressurized metered-dose inhaler P-MDI. Eur Respir J 1994; 7: 1839–44
Kaiser H, Aaronson D, Dockhorn R, et al. Dose-proportional pharmacokinetics of budesonide inhaled via Turbuhaler®. Br J Clin Pharmacol 1999 Sep; 48(3): 309–16
Thorsson L, Edsbäcker S, Källén A, et al. Pharmacokinetics and systemic activity of fluticasone via Diskus® and pMDI, and of budesonide via Turbuhaler®. Br J Clin Pharmacol 2001; 52: 529–38
Bousquet J, Boulet LP, Peters MJ, et al. Budesonide/formoterol for maintenance and relief in uncontrolled asthma vs. high-dose salmeterol/fluticasone. Respir Med. Epub 2007 Oct 1
Kuna P, Peters MJ, Manjra AI, et al. Effect of budesonide/ formoterol maintenance and reliever therapy on asthma exacerbations. Int J Clin Pract 2007 May; 61(5): 725–36
O’Byrne PM, Bisgaard H, Godard PP, et al. Budesonide/ formoterol combination therapy as both maintenance and reliever medication in asthma. Am J Respir Crit Care Med 2005 Jan 15; 171(2): 129–36
Rabe KF, Atienza T, Magyar P, et al. Effect of budesonide in combination with formoterol for reliever therapy in asthma exacerbations: a randomised controlled, double-blind study. Lancet 2006 Aug 26; 368(9537): 744–53
Rabe KF, Pizzichini E, Ställberg B, et al. Budesonide/formoterol in a single inhaler for maintenance and relief in mild-to-moderate asthma: a randomized, double-blind trial. Chest 2006 Feb; 129(2): 246–56
Scicchitano R, Aalbers R, Ukena D, et al. Efficacy and safety of budesonide/formoterol single inhaler therapy versus a higher dose of budesonide in moderate to severe asthma. Curr Med Res Opin 2004 Sep; 20(9): 1403–18
Lundborg M, Wille S, Bjermer L, et al. Maintenance plus reliever budesonide/formoterol compared with a higher maintenance dose of budesonide/formoterol plus formoterol as reliever in asthma: an efficacy and cost-effectiveness study. Curr Med Res Opin 2006 May; 22(5): 809–21
Sears R, Boulet LP, Laviolette M, et al. Budesonide/formoterol maintenance and reliever therapy for asthma compared to conventional best practice: a randomised real-life study [abstract no. E3601]. Eur Respir J 2006 Sep; 28 Suppl. 50: 613–4s
Vogelmeier C, D’Urzo A, Pauwels R, et al. Budesonide/ formoterol maintenance and reliever therapy: an effective asthma treatment option? Eur Resp J 2005 Nov; 26(5): 819–28
Buhl R, Vogelmeier C. Budesonide/formoterol maintenance and reliever therapy: a new treatment approach for adult patients with asthma. Curr Med Res Opin 2007; 23(8): 1867–78
Johansson G, Andreasson EB, Larsson PE, et al. Cost effectiveness of budesonide/formoterol for maintenance and reliever therapy versus salmeterol/fluticasone plus salbutamol in the treatment of asthma. Pharmacoeconomics 2006; 24(7): 695–708
Miller E, Sears MR, McIvor A, et al. Canadian economic evaluation of budesonide-formoterol as maintenance and reliever treatment in patients with moderate to severe asthma. Can Respir J 2007 Jul; 14(5): 269–75
Price D, Wirén A, Kuna P. Cost-effectiveness of budesonide/ formoterol for maintenance and reliever asthma therapy. Allergy 2007 Oct; 62(10): 1189–98
Bousquet J, Miravitlles M, Wirén A. Budesonide/formoterol provides better efficacy at a lower or similar cost as compared to high-dose salmeterol/fluticasone treatment [abstract no. P1185]. Eur Respir J 2007 Sep; 30 Suppl. 51: 193s
Martinez FD. Safety of long-acting beta-agonists: an urgent need to clear the air. N Engl J Med 2005 Dec 22; 353(25): 2637–9
FDA public health advisory: Serevent Diskus (salmeterol xinofoate inhalation powder), Advair Diskus (fluticasone propionate & salmeterol inhalation powder), Foradil Aerolizer (formoterol fumarate inhalation powder) [online]. Available from URL: http://www.fda.gov/cder/drug/advisory/laba.htm [Accessed 2007 Sep 24]
Martinez FD. Serious adverse events and death associated with treatment using long-acting β-agonists. Clin Rev Allergy Immunol 2006; 31(2–3): 269–78
Symbicort® (budesonide/formoterol) Turbuhaler®, 160/4.5 micrograms/inhalation, inhalation powder: summary of product characteristics (Sweden) [online]. Available from URL: http://www.lakemedelsverket.se/upload/SPC_PIL/Pdf/enhumspc [Accessed 2007 Aug 13]
Tattersfield AE, Postma DS, Barnes PJ, et al. Exacerbations of asthma: a descriptive study of 425 severe exacerbations. Am J Respir Crit Care Med 1999 Aug; 160(2): 594–9
Tattersfield AE, Löfdahl CG, Postma DS, et al. Comparison of formoterol and terbutaline for as-needed treatment of asthma: a randomised trial. Lancet 2001 Jan 27; 357(9252): 257–61
Barnes PJ. Using a combination inhaler (budesonide plus formoterol) as rescue therapy improves asthma control. BMJ 2007 Sep 8; 335(7618): 513
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: P.J. Barnes, Imperial College London, Airway Disease Section, National Heart and Lung Institute, London, UK; H. Chrystyn, School of Applied Sciences, University of Huddersfield, Huddersfield, UK; M. Duong, Department of Medicine, Hamilton Health Sciences, McMaster University, Hamilton, Ontario, Canada; A.D. D’Urzo, Primary Care Lung Clinic, Toronto, Ontario, Canada; G. Johansson, Department of Public Health and Caring Sciences, Family Medicine and Clinical Epidemiology, Uppsala University, Uppsala, Sweden; K. Mortimer, Nottingham City Hospital, Nottingham, UK; P. Pohunek, Pediatric Department, Charles University, University Hospital Motol, Prague, Czech Republic; A. Tal, Department of Pediatrics B, Soroka University Medical Center, Ben-Gurion University, Beer-Sheva, Israel.
Data Selection
Sources: Medical literature published in any language since 1980 on ‘budesonide/formoterol’, identified using MEDLINE and EMBASE, supplemented by AdisBase (a proprietary database of Wolters Kluwer Health | Adis). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: MEDLINE, EMBASE and AdisBase search terms were ‘budesonide/formoterol’ or (‘budesonide’ and ‘formoterol’). Searches were last updated 8 October 2007.
Selection: Studies in patients with asthma who received budesonide/formoterol as maintenance and reliever therapy using a single inhaler. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Budesonide/formoterol, asthma, pharmacodynamics, pharmacokinetics, therapeutic use, tolerability, pharmacoeconomics.
Rights and permissions
About this article
Cite this article
McCormack, P.L., Lyseng-Williamson, K.A. Budesonide/Formoterol. Drugs 67, 2407–2431 (2007). https://doi.org/10.2165/00003495-200767160-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200767160-00007