Abstract
Migraine is a paroxysmal disorder with attacks of headache, nausea, vomiting, photo- and phonophobia and malaise. Mild migraine attacks are treated with antiemetics followed by analgesics such as aspirin (acetylsalicylic acid), paracetamol (acetaminophen) or nonsteroidal anti-inflammatory drugs (NSAIDs). Moderate to severe attacks are treated by antiemetics combined with ergotamine or dihydroergotamine.
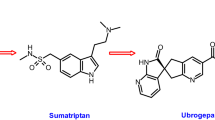
Sumatriptan, a specific serotonin 5-HT1b/d receptor agonist, is used if attacks do not respond to ergotamine or if intolerable adverse effects occur. The new migraine drugs zolmitriptan, naratriptan, rizatriptan and eletriptan differ in their pharmacological profile from sumatriptan, but this translates into only minor differences in efficacy, headache recurrence and adverse effects.
Migraine prophylaxis should be implemented when more than 3 attacks occur per month, if attacks do not respond to acute treatment or if the adverse effects of acute treatment are severe. Substances with proven efficacy include the β-blockers metoprolol and propranolol and the calcium antagonist flunarizine. Drugs less effective or those with unpleasant adverse effects are the serotonin receptor antagonists (pizotifen, methysergide and lisuride), dihydroergotamine, cyclandelate, NSAIDs, valproic acid (sodium valproate) and amitriptyline. The efficacy of aspirin or magnesium is still under evaluation.
Similar content being viewed by others
References
Headache Classification Committee of the International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia 1988; 8 Suppl. 7: 1–93
Joutel A, Bousser M-G, Biousese V, et al. A gene for familial hemiplegic migraine maps to chromosome 19. Nat Genet 1993; 5: 40–5
Ophoff RA, Terwindt GM, Vergouwe MN, et al. Familial hemiplegic migraine and episodic ataxia type-2 are caused by mutations in the Ca2+ channel gene CACNL1A4. Cell 1997; 87: 543–52
Diener HC, Peatfield RC. Migraine. In: Brandt T, Caplan LR, Dichgans J, et al., editors. Neurological disorders: course and treatment. San Diego: Academic Press, 1996: 1–16
Ferrari MD, Saxena PR. 5-HT1 receptors in migraine pathophysiology and treatment. Eur J Neurol 1995; 2: 5–21
Olesen J. A review of current drugs for migraine. J Neurol 1991; 238 Suppl. 1: S23–7
Welch KMA. Drug therapy of migraine. N Engl J Med 1993; 329: 1476–82
Goadsby PJ. How do the currently used prophylactic agents work in migraine? Cephalalgia 1997; 17: 85–92
Couch JR. Placebo effect and clinical trials in migraine therapy. Neuroepidemiology 1987; 6: 178–85
Buzzi G, Sakas DE, Moskowitz MA. Indomethacin and acetylsalicylic acid block neurogenic plasma protein extravasation in rat dura mater. Eur J Pharmacol 1989; 165: 251–8
Kaube H, Hoskin KL, Goadsby PJ. Intravenous acetylsalicylic acid inhibits central trigeminal neurons in the dorsal horn of the upper cervical spinal cord in the cat. Headache 1993; 33: 541–4
Oral Sumatriptan and Aspirin plus Metoclopramide Comparative Study Group. A study to compare oral sumatriptan with oral aspirin plus oral metoclopramide in the acute treatment of migraine. Eur Neurol 1992; 32: 177–84
Tfelt-Hansen P, Henry P, Mulder LJ, et al. The effectiveness of combined oral lysine acetylsalicylate and metoclopramide compared with oral sumatriptan for migraine. Lancet 1995; 346: 923–6
MacGregor EA, Wilkinson M, Bancroft K. Domperidone plus paracetamol in the treatment of migraine. Cephalalgia 1993; 13: 124–7
Moskowitz MA. Neurogenic versus vascular mechanisms of sumatriptan and ergot alkaloids in migraine. Trends Pharmacol Sci 1992; 13: 307–11
Edvinsson L, Goadsby PJ. Neuropeptides in the cerebral circulation: relevance to headache. Cephalalgia 1995; 15: 272–6
Goadsby PJ, Edvinsson L. The trigeminovascular system and migraine: studies characterizing cerebrovascular and neuropeptide changes seen in humans and cats. Ann Neurol 1993; 33: 48–56
Dahlöf C.Placebo-controlled clinical trials with ergotamine in the acute treatment of migraine. Cephalalgia 1993;13: 166–71
Ziegler D, Ford R, Kriegler J, et al. Dihydroergotamine nasal spray for the acute treatment of migraine. Neurology 1994; 44: 447–53
Andersson PG. Ergotism: the clinical picture. In: Diener HC, Wilkinson M, editors. Drug-induced headache. Berlin: Springer, 1988: 16–9
Diener HC, Wilkinson M, editors. Drug-induced headache. Berlin: Springer, 1988
Scholz E, Gerber WD, Diener HC, et al. Dihydroergotamine versus flunarizine versus nifedipine versus metoprolol versus propranolol in migraine prophylaxis: a comparative study based on time series analysis. In: Clifford Rose F, editor. Advances in headache research. London: John Libey and Co., 1987: 135–45
Buzzi MG, Moskowitz MA. Evidence for 5-HT1B/1D receptors mediating the antimigraine effect of sumatriptan and dihydroergotamine. Cephalalgia 1991; 11: 165–8
Ferro A, Longmore J, Hill RG, et al. A comparison of the contractile effects of 5-hydroxytryptamine, sumatriptan and MK-462 on human coronary artery in vitro. Br J Clin Pharmacol 1995; 40: 245–51
Martin GR. Pre-clinical pharmacology of zolmitriptan (Zomig™; formerly 311C90), a centrally and peripherally acting 5HT1b/1dagonist for migraine. Cephalalgia 1997; 17: 4–14
Buzzi MG, Moskowitz MA, Peroutka SJ, et al. Further characterization of the putative 5-HT receptor which mediates blockade of neurogenic extravasation in rat dura mater. Br J Pharmacol 1991; 103: 1421–8
Goadsby PJ, Edvinsson L. Sumatriptan reverses the changes in calcitonin gene-related peptide seen in the headache phase of migraine. Cephalalgia 1991; 11 Suppl. 11: 3–4
Godsby PJ, Hoskin KL. Inhibition of trigeminal neurons by intravenous administration of the serotonin (5HT)1B/D receptor agonist zolmitriptan (311C90): are brainstem sites therapeutic target in migraine? Pain 1996; 67: 355–9
Cumberbatch MJ, Hill RG, Hargreaves RJ. Rizatriptan has central antinociceptive effects against durally evoked responses. Eur J Pharmacol 1997; 328: 37–40
Cutler NR, Claghorn J, Sramek JJ, et al. Pilot study of MK-462 in migraine. Cephalalgia 1996; 16: 113–6
Solomon GD, Cade RK, Klapper JA, et al. Clinical efficacy and tolerability of 2.5 mg zolmitriptan for the acute treatment of migraine. Neurology 1997; 49: 1219–25
Pilgrim AJ, Blakeborough P. The clinical efficacy of sumatriptan in the acute treatment of migraine. Rev Contemp Pharmacother 1994; 5: 295–309
Oral Sumatriptan Dose-Defining Study Group. Sumatriptan —an oral dose-defining study. Eur Neurol 1991; 31: 300–5
Wilkinson M, Pfaffenrath V, Schoenen J, et al. Migraine and cluster headache — their management with sumatriptan: a critical rewiew of the current clinical experience. Cephalalgia 1995; 15: 337–57
Mathew NT, Asgharnejad M, Peykamian M, et al. Naratriptan is effective and well tolerated in the acute treatment of migraine: results of a double-blind, placebo-controlled, crossover study. Neurology 1997; 49: 1485–90
Tfelt-Hansen P. Preliminary analysis of randomized placebo-controlled clinical trials with newer 5-HT1d receptor agonists for the treatment of migraine attacks. In: Oleson J, Tfelt-Hansen P, editors. Frontiers of headache research headache treatment: trial methodology and new drugs. New York: Raven Press, 1997: 253–6
Visser WH, Jaspers NMWH, de Vriend RHM, et al. Risk factors for headache recurrence after sumatriptan: a study in 366 migraine patients. Cephalalgia 1996; 16: 264–9
Weiller C, May A, Limmroth V, et al. Brain stem activation in spontaneous human migraine attacks. Nat Med 1995; 1: 658–60
Winner P, Ricalde O, Le Force B, et al. A double-blind study of subcutaneous dihydroergotamine vs subcutaneous sumatriptan in the treatment of acute migraine. Arch Neurol 1996; 53: 180–4
Jackson NC, on behalf of the Eletriptan Steering Committee. Clinical measures of efficacy, safety and tolerability for the acute treatment of migraine: a comparison of eletriptan) 20–80mg), sumatriptan (100mg) and placebo [abstract]. Neurology 1998; 50 Suppl. 4: A376
Brown EG, Endersby CA, Smith RN, et al. The safety and tolerability of sumatriptan: an overview. Eur Neurol 1991; 31: 339–44
Diener HC. Substance P antagonist RPR100893-201 is not effective in human migraine attacks. 6th International Headache Research Seminar; 1995 Nov 19: Copenhagen
Goldstein DJ, Wang O, Saper JR, et al. Ineffectiveness of neurokinin-1 antagonist in acute migraine: crossover study. Cephalalgia 1997; 17: 785–90
May A, Gijsman HJ, Wallnöfer A, et al. Endothelin antagonist bosentan blocks neurogenic inflammation, but is not effective in aborting migraine attacks. Pain 1996; 67: 375–8
Roon K, Diener HC, Ellis P, et al. CP-122,288 blocks neurogenic inflammation, but is not effective in aborting migraine attacks: results of two controlled clinical trials [abstract]. Cephalalgia 1997; 17(3): 245
Hämäläinen ML, Hoppu K, Santavuori P. Sumatriptan for migraine attacks in children: a randomized placebo-controlled study. Do children with migraine attacks respond to oral sumatriptan differently from adults? Neurology 1997; 48: 1100–3
Lanzi G, Balottin U, Zambrino CA, et al. Guidelines and recommendations for the treatment of migraine in Pediatric and adolescent patients. Funct Neurol 1996; 11: 269–75
Caers LI, DeBeukelaar F, Amery WK. Flunarizine, a calciumentry blocker, in childhood migraine, epilepsy, and alternating hemiplegia. Clin Neuropharmacol 1987; 10: 162–8
DelBene E, Gatto G, Poggioni M. Clinical and pharmacological investigation in flunarizine treated migrainous children. Collegium Internationale Neuropsychopharmacologicum 1984; 51
Haemaelaeinen ML, Hoppu K, Sanatvuori PR. Oral dihydroergotamine for therapy-resistant migraine attacks in children. Pediatr Neurol 1997; 2: 114–7
Linder SL. Treatment of childhood headache with dihydroergotamine mesylate. Headache 1994; 34: 578–80
Saadah HA. Abortive headache therapy with intramuscular dihydroergotamine. Headache 1992; 32: 18–20
Diener HC, Limmroth V. The treatment of migraine. Rev Contemp Pharmacother 1994; 5: 271–84
Hoffert MJ, Couch JR, Diamond S, et al. Transnasal butorphenol in the treatment of acute migraine. Headache 1995; 35: 65–9
Couturier EGM, Hering R, Steiner TJ. Weekend attacks in migraine patients: caused by caffeine withdrawal. Cephalalgia 1992; 12: 99–100
van Dusseldorp M, Katan MB. Headache caused by caffeine withdrawal among moderate coffee drinkers switched from ordinary to decaffeinated coffee: a 12-week double-blind trial. BMJ 1990; 300: 1558–9
Migraine-Nimodipine European Study Group (MINES). European multicenter trial of nimodipine in the prophylaxis of common migraine (migraine without aura). Headache 1989; 29: 633–8
Migraine-Nimodipine European Study Group (MINES). European multicenter trial of nimodipine in the prophylaxis of classic migraine (migraine with aura). Headache 1989; 29: 639–42
Holroyd KA, Penzien DB, Cordingley GE. Propranolol in the management of recurrent migraine: a meta-analytic review. Headache 1991; 31: 333–40
Peatfield RC, Fozard JR, Rose CF. Drug treatment of migraine. In: Clifford Rose F, editor. Handbook of clinical neurology. Vol. 4 (48): Headache. Amsterdam: Elsevier Science Publishers B.V., 1986: 173–217
Stensrud P, Sjaastad O. Comparative trial of Tenormin (atenolol) and Inderal (propranolol) in migraine. Headache 1980; 20: 204–7
Tfelt-Hansen P, Standnes B, Kangasniemi P, et al. Timolol vs propranolol vs placebo in common migraine prophylaxis: a double-blind multicenter trial. Acta Neurol Scand 1984; 69: 1–8
Freitag FG, Diamond S. Nadolol and placebo comparison study in the prophylactic treatment of migraine. J Am Osteopath Assoc 1984; 84: 343–7
van de Ven LLM, Franke CL, Koehler PJ. Prophylactic treatment of migraine with bisoprolol: a placebo-controlled study. Cephalalgia 1997; 17: 596–9
Olesen J, Tfelt-Hansen P, Welch KMA, editors. The headaches. New York, Raven Press, 1993
Markley HG, Cheronis CD, Piepho RW. Verapamil in prophylactic therapy of migraine. Neurology 1984; 34: 973–6
Solomon CGD, Steel MJG, Spaccavento CLJ. Verapamil prophylaxis of migraine. JAMA 1983; 250: 2500–2
Albers GW, Simon LT, Hamik A, et al. Nifedipine versus propranolol for the initial prophylaxis of migraine. Headache 1989; 29: 214–7
Diener HC, Föh M, Iaccarino C, et al. Cyclandelate in the prophylaxis of migraine: a randomized, parallel, double-blind study in comparison with placebo and propranolol. Cephalalgia 1996; 16: 441–7
Bousser MG, Chick J, Fuseau E, et al. Combined low-dose acetylsalicylic acid and dihydroergotamine in migraine prophylaxis. Cephalalgia 1988; 8: 187–92
Buscaino GA, Sorge F, Bussone G, et al. Preventive treatment of headache with slow-release dihydroergotamine: comparison of dosage protocols. Curr Ther Res 1991; 49: 925–35
Scholz E, Gerber WD, Diener HC, et al. Dihydroergotamine versus flunarizine versus nifedipine versus metoprolol versus propranolol in migraine prophylaxis. A comparative study based on time series analysis. In: Clifford Rose F, editor. Advances in headache research. London: John Liey & Co., 1987: 135–45
Dichgans J, Diener HC, Gerber WD, et al. Analgetika-induzierter Dauerkopfschmerz. Dtsch Med Wochenschr 1984; 109: 369–73
Buring JE, Peto R, Hennekens CH. Low-dose aspirin for migraine prophylaxis. JAMA 1990; 264: 1711–3
Grotemeyer K-H, Scharafinski H-W, Schlake H-P, et al. Acetylsalicylic acid vs metoprolol in migraine prophylaxis — a double blind cross-over study. Headache 1990; 30: 639–41
Diener HC, Härtung E, Chrubasik J, et al. Acetylsalicylic acid in migraine prophylaxis: a double blind study in comparison with metoprolol [abstract]. Cephalalgia 1997; 17(3): 434
Bellavance AJ, Meloche JP Comparative study of naproxen sodium, pizotyline and placebo in migraine prophylaxis. Headache 1990; 30: 710–5
Diamond S, Freitag FG, Gallagher RM, et al. Ketoprofen in the prophylaxis of migraine. Headache Quarterly 1990; 1: 75–7
Johnson RH, Hornabrook RW, Lambie DG. Comparison of mefanamic acid and propranolol with placebo in migraine prophylaxis. Acta Neurol Scand 1986; 73: 490–2
Mikkelsen B, Pedersen KK, Christiansen LV. Prophylactic treatment of migraine with tolfenamic acid, propranolol and placebo. Acta Neurol Scand 1986; 73: 423–7
Sternieri E, Bussone G, Manzone GC, et al. Lornoxicam, a new nonsteroidal anti-inflammatory drug, in migraine prophylaxis: a double-blind multicenter study. Cephalalgia 1991; 11 Suppl. 11: 154–5
Couch JR, Hassanein RS. Amitriptyline in migraine prophylaxis. Arch Neurol 1979; 36: 695–9
Ziegler DK, Hurwitz A, Hassanein RS. Migraine prophylaxis: a comparison of propranolol and amitriptyline. Arch Neurol 1987; 44: 486–9
Hering R, Kurzitzky A. Sodium valproate in the prophylactic treatment of migraine: a double-blind study versus placebo. Cephalalgia 1992; 12: 81–4
Jensen R, Brinck T, Olesen J. Sodium valproate has a prophylactic effect in migraine without aura: a triple-blind, placebo-controlled crossover study. Neurology 1994; 44: 647–51
Mathew NT, Saper JR, Silberstein SD, et al. Migraine prophylaxis with divalproex. Arch Neurol 1995; 52: 281–6
Silberstein SD. Divalproex sodium in headache: literature review and clinical guidelines. Headache 1996; 36: 547–55
Klapper J. Divalproex sodium in migraine prophylaxis: a dose-controlled study. Cephalalgia 1997; 17: 103–8
Peikert A, Wilimzig C, Kühne-Volland R. Prophylaxis of migraine with oral magnesium: results from a prospective, multi-center, placebo-controlled and double-blind randomized study. Cephalalgia 1996; 16: 257–63
Pfaffenrath V, Wessely P, Meyer C, et al. Magnesium in the prophylaxis of migraine — a double-blind, placebo-controlled study. Cephalalgia 1996; 16: 436–40
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Diener, HC., Kaube, H. & Limmroth, V. A Practical Guide to the Management and Prevention of Migraine. Drugs 56, 811–824 (1998). https://doi.org/10.2165/00003495-199856050-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199856050-00006