Screening for prostate cancer: are organized screening programs necessary?
Prostate cancer (PCa) screening: the trials
It is now 27 years ago that a study was published on the usefulness of the prostate-specific antigen (PSA) test in the detection and staging of PCa (1). This multicentre study demonstrated that biopsying men with a PSA level greater than 4.0 ng/mL, with or without a suspicious digital rectal examination (DRE), was an effective selection process. Of every 100 men aged 50–75, approximately 85 men had PSA values less than 4.0 ng/mL. Of the remaining 15 men who were biopsied, 4–5 men were found to have a clinically significant cancer. If DRE alone had been used to select the men who had biopsies, 32% of cancers would have been missed. In addition, the use of DRE and PSA increased the rate of organ confined disease from 70–85% as compared to 30% when detection was driven by DRE only. The authors concluded that although the PSA test is an imperfect screening test, when combined with DRE it increases the rate of (organ confined) PCa detection. Interestingly, already then screening for PCa was considered controversial due to the considerable risk of detecting latent PCa. In addition, there was concern about the impact of results of randomised PCa screening trials that, if not properly interpreted, could give a false impression on the effect on survival. However, it was clear cut that such trials were needed and just two years after this publication both in the US and Europe two randomised screening trials on PSA-based screening for PCa were initiated.
It is highly unlikely that someone working in the field of PCa early detection has not heard of the European Randomised study of Screening for Prostate Cancer (ERSPC) and the Prostate, Lung, Colorectal and Ovary (PLCO) cancer screening trials (2,3). Both trials aimed to answer the question whether PSA-based screening could reduce disease-specific mortality. During the period 1993–2009 the trials recruited and screened participants and gathered data for future analyses on their main outcome. All the while, the PSA test was used as a screening tool in daily clinical practice. The test became widely adopted for screening and the U.S. Food and Drug Administration (FDA) and professional societies issued guidelines where its use was acknowledged or supported (4-6).
After sixteen years of relative silence while working hard behind the scenes, both trials published their results on the effect of PSA-based screening on disease-specific mortality simultaneously in 2009 (7,8). Unfortunately, the publications caused confusion. The main question whether PSA-based screening resulted in a decrease of PCa-specific mortality as compared to a situation with no or little screening could not be answered with a definite yes or no. Many years of debate followed during which the PSA test was used abundantly. It became clear that the PLCO, claiming a negative answer to the question, suffered from weakness in design and conduct of the trial while the ERSPC was sufficiently powered to answer the question (9,10). In fact, a recently published study using analytic and microsimulation models concluded that “After differences in implementation and settings are accounted for, the ERSPC and PLCO provide compatible evidence that screening reduces PCa mortality” (11). So, now that it is more or less accepted that screening can save men dying from PCa we can finally fully focus on who these men are and how to identify them.
During the conduct of the trials and certainly after the first publications in 2009 the focus of research was already on balancing the harms and (potential) benefits of screening. It soon became clear that the observations about the risk of diagnosing latent PCa already made in 1991 became reality. Since the early nineties, in virtually all western countries an enormous increase in incidence was observed (12,13). The majority of these newly diagnosed cancers were clinically localized, which led to an increase in radical prostatectomy and radiation therapy, aggressive treatments intended to cure these early-stage cancers but in fact causing over treatment.
PCa screening: the guidelines and shared decision making (SDM)
As stated earlier, the potential of the PSA test as a screening tool was already acknowledged in different guidelines in the 90s. However, with more data becoming available on steeply increasing PCa detection rates, related over treatment and a questionable benefit of screening, the medical societies changed their views and adapted their guidelines. The guidelines focused more on an individual approach and stressed on the importance of SDM. Table 1 shows a summary of the guidelines of the European Association of Urology (EAU), the American Urological Association (AUA) and the US Preventive Services Task Force (USPSTF), issued in 2012–2014.
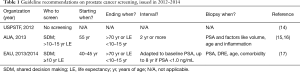
Full table
The most stringent recommendation was that of the USPSTF, recommending against PSA screening. Other guidelines focused on methods to reduce harm and advised on (I) the age to stop further testing, (II) to only test when men are fully informed about the potential benefits and harms (SDM) and (III) using the PSA test as an initial risk stratification tool followed by various screening intervals or additional testing (reflex testing) before referring for prostate biopsy. In addition, many guidelines mentioned the option of active surveillance in case of a diagnosis of low-risk PCa.
So, while one organization recommended to stop using PSA as a screening test, others set constraints, but felt that it was appropriate to screen if a man was well-informed. It was felt that if these straightforward recommendations were followed the burden of unnecessary testing and over diagnosis should be acceptable. This potential reduction of harms was confirmed in modelling studies. Gulati performed a microsimulation modelling study of PCa incidence and mortality quantifying harms and lives saved for alternative PSA screening strategies. They concluded that PSA screening strategies that use higher thresholds for biopsy referral for older men and that screening men with low PSA levels less frequently can reduce harms while preserving lives saved (18). Carlsson, also using a microsimulation model on the basis of ERSPC data (MISCAN), compared outcomes of a daily clinical practice model with a “recommended good practice” model where these simple recommendations on screening and treatment found in many guidelines were incorporated. The results, expressed in quality adjusted life years (QALYs) gained, showed that for a cohort of 1,000 screened men followed over the course of their life the recommended good practice approach led to 73 life-years (LYs) and 74 QALYs gained. In contrast, common practice led to 78 LYs gained while only gaining 19 QALYs; which is more than a 75% relative reduction in QALYs gained. The authors noted that this reduction was mainly caused by the use of aggressive treatment for low-risk PCa and continuous PSA testing in older men (19).
Most likely confusing for both physician and patient, the USPSTF decided to adapt their recommendation on PSA screening. In May 2017 the latest data on PSA-based screening, i.e., longer term follow-up results of the randomised controlled trials, and changes in treatment options were evaluated. The USPSTF released a draft recommendation stating that they advise individualized decision-making about screening for PCa after discussion with a clinician, so that each man has an opportunity to understand the potential benefits and harms of screening and to incorporate his personal values and preferences into his decision. This recommendation holds for men aged 55–69 years (20). The EAU refined its recommendations and focused on individual risk stratification and the use of risk calculators, while the AUA in 2015 confirmed the validity of its 2013 guidelines (21,22) (Table 2).
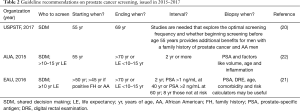
Full table
In summary, the current recommendations on PSA-based screening are that one can offer a PSA test to a well-informed man, that this PSA test should serve as a baseline risk stratification tool and that further testing (repeat PSA) depends on the PSA level and a man’s life expectancy (often summarised into an cut-off age <70–75 years). For the decision to biopsy the outcome of reflex testing (additional biomarkers, risk prediction tools and/or imaging) should be leading. The decision to biopsy should not be done on the basis of a PSA test alone.
Implementation of guidelines and recommendations into daily clinical practice is however not straightforward. Recommendations in guidelines are predominantly based on the evidence of effectiveness, but physicians have to consider many other highly relevant factors like patient preferences, costs, competing health issues and the actual benefit of the intervention when dealing with an individual. Despite the fact that contemporary guidelines acknowledge the role of patient preferences and costs, no guideline can weigh their importance for every individual patient. This was recently acknowledged by the release of an evidence-based clinical guideline on how to manage localized PCa by a joint initiative of three professional societies, the AUA, the American Society for Radiation Oncology and the Society of Urologic Oncology. The chair of the guideline development panel said that “Selecting optimal care for each PCa patient is a complex process that requires physicians to help patients choose options consistent with the patient’s own values and in accordance with the best available scientific evidence” (23).
SDM is thus the general advice. A term that was introduced many years ago referring to the process by which patients, physicians and caregivers arrive at treatment decisions together based on clinical evidence within the context of patients’ personal preferences. In the 90s SDM was considered neither sufficient nor desirable, as this would lead to an unrealistic responsibility for patients. The words, “it’s your decision” would make patients feel abandoned, rather than cared or empowered. However, SDM should be seen as a conversation between physician and (future) patient in which they think, talk, and consider the situation of each patient; it is an expression of care (24).
This sounds without doubt as the right thing to do, however practice change is governed by factors such as cost and efficiency. Informing a patient can be time-consuming and time constraints are the most frequently cited barrier to any change in clinical practice. In this context, implementation might also be complicated by the readily available, apparently inexhaustible information accessible on the internet. In fact, while patients feel more confident with having medical information and feel they are better able to ask more informed questions, practice can turn out to be different. In a study among medical oncologists, researchers found that when a patient brings online health information to an appointment, the doctor had to spend about 10 extra minutes discussing it before they could actually start with the true purpose of the visit (25).
PCa screening: daily clinical practice
Now back to PSA-based screening and what is actually happening in daily clinical practice. Published data on PSA screening practices in both Europe and the US are not that encouraging. When focusing on the recommendation to be prudent with testing in elderly men several studies show the opposite (Table 3). A study among 136 London inner GP practices showed that the rate of PSA testing was positively associated with age and the peak testing prevalence was amongst patients 70–80 years old (26). In Poland, based on data from the population-based PolSenior study, it was shown that PSA testing rates were highest in men >70 years (27). Similar results were reported from a population-based cross-sectional survey on awareness of colorectal, breast, cervical and PCa screening in Spain (28). Men in the highest age group (>67 years) had the highest rate of PSA testing (36%). The largest study covering this topic is a Swedish study conducted among males living in Stockholm County (N=1,034,129). The highest prevalence of PSA testing was amongst men aged 70–79 years with the third highest being men aged >80 years (29). In addition, this study reported retesting rates showing that despite a low PSA level of <1.0 ng/mL, according to the guidelines a level where retesting should not be done or at least with an interval >4 years, 30% of men were retested within 2 years. In 2006, in the US, based on data from a cohort study of 597,642 male veterans aged 70 years and older without a history of PCa, elevated PSA, or PCa symptoms and having the availability on comorbidity data according to the Charlson comorbidity score [best health (score =0) to worst health (score ≥4)] the researchers concluded that 56% of men were PSA tested. In addition, while it is known that an increase in Charlson score from 0 to 4 is associated with more than a 4-fold increased risk of death, bad health was associated with only a small decrease in PSA testing rates. PSA rates ranged from 58% for men in best health to 51% for men in worst health (30).
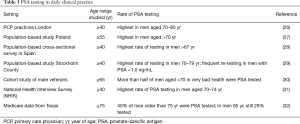
Full table
In 2011, based on the population-based 2000 and 2005 National Health Interview Survey (NHIS), it was shown that the PSA screening rate was 24.0% in men age 50 to 54 years, increasing to 45.5% among age 70 to 74 years. In men age 85 years or older still 24.6% reported being screened (31). Also here, the authors concluded that the merits and limitations of PSA should be discussed with all patients considering PCa screening. Frequent testing in the elderly was again confirmed with Texan Medicare data from 2013. Researchers found that 41% of men 75 or older were regularly screened and about 29% of these PSA tests were ordered by primary care physicians (PCP) where it was noted that some PCPs were up to seven times more likely to order a PSA test (32). This observation of differences in the rate of ordering a PSA test could point toward a subjective approach in ordering PSA tests. Data from Germany corroborate this. On the basis of a survey among 500 randomly selected PCPs from all over Germany it was shown that male PCPs were 3.7 to 7.9 times as likely to recommend and conduct PCa screening on a regular basis. Patient-physician gender concordance made it more likely that male-specific cancer screenings would be recommended. Remarkably this was not the case for female-specific screenings (33). A similar survey conducted among PCPs in the US showed comparable results. The likelihood of having a discussion on PSA testing was significantly associated with the belief that PSA screening is advantageous. The most common identified barriers to start a discussion on PSA testing were lack of time, the complexity of the topic, and a language barrier (34).
In addition to the data mentioned above, the rate of PSA testing in those who might benefit from early detection is heavily depended on socioeconomic status (SES). In Australia it was found that the probability of a man having a PSA test and if applicable the management of his PCa depends on where he lives. While PSA testing is common across the whole of Australia, age-standardised rates were 16% lower in regional and rural areas than in capital cities (35). In a recent US-based study the impact of race and SES on receipt of PSA testing among low-income men was examined. From 2002 to 2009 black (n=22,167) and white (n=9,588) men aged ≥40 years completed a questionnaire where among other questions they were asked whether they had ever received PSA testing and had testing within the prior 12 months. Lower SES was significantly associated with less receipt of PSA testing in both groups (36).
In summary, PSA testing in daily clinical practice is not quite comparable to what is recommended in the guidelines. Looking at the high rates of detection of low risk PCa it is obvious that also recommendations on reflex testing before the decision to biopsy is most likely something that could be improved. Furthermore, data from Sweden showed that unregulated opportunistic screening in fact only lead to harm (unnecessary testing and over diagnosis) while there was no benefit in terms of PCa mortality reduction (37).
After PSA testing many biomarkers and nowadays also mpMRI are recommended to be used before deciding to biopsy. This so-called reflex testing has shown to be able to reduce unnecessary testing and the diagnosis of low-risk potentially over diagnosed cancers with up to 50% and 40% respectively (38,39). In summary, while knowledge is available to streamline PSA testing these guidelines are poorly implemented despite numerous publications and straightforward appeals to do so (40,41).
PCa screening in an organized setting?
Reiterating the data mentioned above the question arises how to continue. Stopping the use of the PSA test as a screening tool is unrealistic. Even a very distinct recommendation not to use the PSA test for screening purposes (USPSTF in 2012) had at best a very modest impact. So, while accepting that the PSA test is here to stay and that in fact it can save suffering of metastatic disease and mortality, another option is to take PSA testing out of clinical care into organized screening programs. Organized screening differs from opportunistic screening primarily on the basis of how men are invited. In organized screening, invitations are based on centralized population registers while in opportunistic screening participation actually depends on the individual’s decision or on visits to health care providers, possibly also for totally different reasons. In addition, in organized screening crucial issues like eligibility requirements, quality assurance and adequate follow-up are defined and constantly monitored. Because the potential benefits of screening are sensitive to shortcomings at any of these in the process, screening that is organized and appropriately funded should have greater potential to yield maximum benefit (42).
If we would decide to organize PSA screening in population-based programs the first obvious question is how to design the algorithm. What both randomised trials showed ubiquitously was that a pure PSA-based algorithm in combination with a random biopsy technique and repeating this intervention at fixed intervals in all men eligible is not the way to go. The consequences of initiation of such a population-based program can be found in Lithuania. The programme was launched in 2006, where men aged 50–74, as well as men aged 45–49 with family history of PCa were offered PSA testing once a year. In 2008 this was already changed to every 2 years due to logistical and costs restraints. Compared to 1990–1994, when approximately 2,200 PCa were diagnosed, diagnoses increased by 50% between 1995–1999, and doubled in each consecutive period. In the period 2005–2009 more than 15,000 PCa were detected. This incidence peak is most likely the highest age-specific PCa incidence peak ever recorded in a country to date. Although it is too soon to expect any effect on PCa mortality reduction it is obvious that over diagnosis is a considerable problem within this program (43).
Other European countries, especially the Nordic countries, opted for another approach. Here, very large population-based trials were and are initiated to assess the value of recent developments around biomarkers and imaging in selecting those men that could benefit from early diagnosis and hence avoiding biopsy in those men that will not harbour PCa or low-risk PCa. In the Stockholm area a trial comprising of 47,688 men age 50–69 years reported on the performance of the so-called STHLM-3 risk prediction model which selectively identifies men with Gleason ≥7 PCa. The STHLM3 model is a test consisting of a combination of plasma protein biomarkers (PSA, free PSA, intact PSA, hK2, MSMB, and MIC1), genetic markers, clinical variables (age, family history, previous prostate biopsy), and a prostate exam (digital rectal exam and prostate volume). Data showed that at a sensitivity level for detecting PCa comparable to biopsying all men with a PSA ≥3.0 ng/mL the STHLM3 model could reduce the number of biopsies by 32% and could avoid 44% benign biopsies (44). Obviously, while the detection was based on a 10–12 core systematic biopsy the next step is to combine the panel with mpMRI. This so-called STHLM3 MRI phase 2 study is almost completed and will include 9,000 men (45). In Finland a population-based randomized screening trial will be started, with 67,000 men aged 55–67 years at entry (46). A quarter of the men will be allocated to the intervention arm, have their PSA measured and in case of a PSA >3.0 ng/mL be tested with the so-called 4K test (47). Those men considered at increased risk of clinically relevant PCa will undergo mpMRI. Men with a malignancy-suspect finding on MRI are referred for targeted biopsies. Also the screening interval will be individualised with an interval of 6 years for men with baseline PSA <1.5 ng/mL, 4 years for PSA 1.5–3.0 ng/mL and 2 years if initial PSA >3.0 ng/mL. Obviously, results related to PCa mortality will be available after 10–15 years. Also in the Netherlands a population-based initiative is being developed where individual multivariate risk prediction and mpMRi will be part of the screening algorithm. Within Europe these initiatives are endorsed by >30 PCa screening experts. During a consensus meeting in 2016, they concluded that starting pilot studies for the implementation of limited organized PCa screening is justified. This decision was based on the available evidence for effectiveness, balance between harms and benefits, and the cost-effectiveness of organized screening as described in the literature. Additional conclusions were that developments in biomarkers, risk predictors, MRI, active surveillance for low-risk PCa combined into stratified screening strategies should be further explored to improve harm-benefit trade-offs and therefore the cost-effectiveness. A well-organized programme in a relatively small age range is preferred over the currently considerable amount of opportunistic testing at older ages (48).
In conclusion, the advice to implement the currently available knowledge as summarised in guidelines remains crucial and should be quoted as much as possible. In the future a change to organized, evidence-based, population-based screening programs is the way to go and research as described in this focused issue on screening and active surveillance is crucial in achieving this.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Catalona WJ, Smith DS, Ratliff TL, et al. Measurement of prostate-specific antigen in serum as a screening test for prostate cancer. N Engl J Med 1991;324:1156-61. [Crossref] [PubMed]
- Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial (PLCO). National Cancer Institute, Division of Cancer Prevention. Available online: prostate-lung-colorectal (accessed: November 27, 2017).https://prevention.cancer.gov/major-programs/
- ERSPC Background. Available online: (accessed: November 27, 2017).http://www.erspc.org/prostatecancer/erspc-background/#study-protocol
- Mettlin C, Jones G, Averette H, et al. Defining and updating the American Cancer Society guidelines for the cancer-related checkup: prostate and endometrial cancers. CA Cancer J Clin 1993;43:42. [Crossref] [PubMed]
- Aus G, Abbou CC, Pacik D, et al. EAU guidelines on prostate cancer. Eur Urol 2001;40:97-101. [Crossref] [PubMed]
- Available online: (assessed at November 26, 2017).http://www.nytimes.com/1994/08/31/us/fda-approves-prostate-blood-test.html
- Schröder FH, Hugosson J, Roobol MJ, et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med 2009;360:1320-8. [Crossref] [PubMed]
- Andriole GL, Crawford ED, Grubb RL 3rd, et al. Mortality results from a randomized prostate-cancer screening trial. N Engl J Med 2009;360:1310-9. [Crossref] [PubMed]
- Gulati R, Tsodikov A, Wever EM, et al. The impact of PLCO control arm contamination on perceived PSA screening efficacy. Cancer Causes Control 2012;23:827-35. [Crossref] [PubMed]
- Shoag JE, Mittal S, Hu JC. Reevaluating PSA testing rates in the PLCO trial. N Engl J Med 2016;374:1795-6. [Crossref] [PubMed]
- Tsodikov A, Gulati R, Heijnsdijk EAM, et al. Reconciling the effects of screening on prostate cancer mortality in the ERSPC and PLCO trials. Ann Intern Med 2017;167:449-55. [PubMed]
- Bray F, Kiemeney LA. Epidemiology of Prostate Cancer in Europe: Patterns, Trends and Determinants. In: Bolla M, van Poppel H. editors. Management of Prostate Cancer. Cham: Springer, 2017.
- Wong MC, Goggins WB, Wang HH, et al. Global Incidence and Mortality for Prostate Cancer: Analysis of Temporal Patterns and Trends in 36 Countries. Eur Urol 2016;70:862-74. [Crossref] [PubMed]
- Moyer VA. U.S. Preventive Services Task Force. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2012;157:120-34. [Crossref] [PubMed]
- Carter HB, Albertsen PC, Barry MJ, et al. Early detection of prostate cancer: AUA guideline. J Urol 2013;190:419-26. [Crossref] [PubMed]
- Carter HB, Albertsen PC, Barry MJ, et al. Early detection of prostate cancer: AUA guideline (unabridged version). American Urological Association, 2013. Available online: http://www.auanet.org/guidelines/early-detection-of-prostate-cancer-(2013-reviewed-and-validity-confirmed-2015)
- Heidenreich A, Abrahamsson PA, Artibani W, et al. Early detection of prostate cancer: European Association of Urology recommendation. Eur Urol 2013;64:347-54. [Crossref] [PubMed]
- Gulati R, Gore JL, Etzioni R. Comparative effectiveness of alternative prostate-specific antigen--based prostate cancer screening strategies: model estimates of potential benefits and harms. Ann Intern Med 2013;158:145-53. [Crossref] [PubMed]
- Carlsson SV, de Carvalho TM, Roobol MJ, et al. Estimating the harms and benefits of prostate cancer screening as used in common practice versus recommended good practice: A microsimulation screening analysis. Cancer 2016;122:3386-93. [Crossref] [PubMed]
- Available online: https://www.uspreventiveservicestaskforce.org/Page/Document/draft-recommendation-statement/prostate-cancer-screening, accessed at November 27, 2017.
- Mottet N, Bellmunt J, Briers E, et al. EAU guidelines (full text guidelines) prostate cancer. European Association of Urology. Available online: https://uroweb.org/guideline/prostate-cancer/
- Available online: http://www.auanet.org/guidelines/early-detection-of-prostate-cancer-(2013-reviewed-and-validity-confirmed-2015), accessed at November 27, 2017.
- AUA, ASTRO and SUO Release New Clinical Guideline on Standard of Care for Men with Localized Prostate Cancer. Available online: https://www.prnewswire.com/news-releases/aua-astro-and-suo-release-new-clinical-guideline-on-standard-of-care-for-men-with-localized-prostate-cancer-300453577.html, accessed at November 27, 2017.
- Kunneman M, Montori VM, Castaneda-Guarderas A, et al. What Is Shared Decision Making? (and What It Is Not). Acad Emerg Med 2016;23:1320-4. [Crossref] [PubMed]
- Helft PR, Hlubocky F, Daugherty CK. American oncologists' views of internet use by cancer patients: a mail survey of American Society of Clinical Oncology members. J Clin Oncol 2003;21:942-7. [Crossref] [PubMed]
- Nderitu P, Van Hemelrijck M, Ashworth M, et al. Prostate-specific antigen testing in inner London general practices: are those at higher risk most likely to get tested? BMJ Open 2016;6:e011356. [Crossref] [PubMed]
- Prajsner A, Chudek J, Szybalska A, et al. Socioeconomic determinants of prostate-specific antigen testing and estimation of the prevalence of undiagnosed prostate cancer in an elderly Polish population based on the PolSenior study. Arch Med Sci 2016;12:1028-35. [Crossref] [PubMed]
- Carrasco-Garrido P, Hernandez-Barrera V, Lopez de Andres A, et al. Awareness and uptake of colorectal, breast, cervical and prostate cancer screening tests in Spain. Eur J Public Health 2014;24:264-70. [Crossref] [PubMed]
- Nordström T, Aly M, Clements MS, et al. Prostate-specific antigen (PSA) testing is prevalent and increasing in Stockholm County, Sweden, Despite no recommendations for PSA screening: results from a population-based study, 2003-2011. Eur Urol 2013;63:419-25. [Crossref] [PubMed]
- Walter LC, Bertenthal D, Lindquist K, et al. PSA screening among elderly men with limited life expectancies. JAMA 2006;296:2336-42. [Crossref] [PubMed]
- Drazer MW, Huo D, Schonberg MA, et al. Population-based patterns and predictors of prostate-specific antigen screening among older men in the United States. J Clin Oncol 2011;29:1736-43. [Crossref] [PubMed]
- Jaramillo E, Tan A, Yang L, et al. Variation among primary care physicians in prostate-specific antigen screening of older men. JAMA 2013;310:1622-4. [Crossref] [PubMed]
- Engler J, Dahlhaus A, Güthlin C, et al. The readiness of German GPs to recommend and conduct cancer screening is associated with patient-physician gender concordance. Results of a survey. Eur J Gen Pract 2017;23:11-9. [Crossref] [PubMed]
- Dunn AS, Shridharani KV, Lou W, et al. Physician-patient discussions of controversial cancer screening tests. Am J Prev Med 2001;20:130-4. [Crossref] [PubMed]
- Coory MD, Baade PD. Urban-rural differences in prostate cancer mortality, radical prostatectomy and prostate-specific antigen testing in Australia. Med J Aust 2005;182:112-5. [PubMed]
- Moses KA, Zhao Z, Bi Y, et al. The impact of sociodemographic factors and PSA screening among low-income Black and White men: data from the Southern Community Cohort Study. Prostate Cancer Prostatic Dis 2017;20:424-9. [Crossref] [PubMed]
- Arnsrud Godtman R, Holmberg E, Lilja H, et al. Opportunistic testing versus organized prostate-specific antigen screening: outcome after 18 years in the Göteborg randomized population-based prostate cancer screening trial. Eur Urol 2015;68:354-60. [Crossref] [PubMed]
- Carlsson SV, Roobol MJ. Improving the evaluation and diagnosis of clinically significant prostate cancer in 2017. Curr Opin Urol 2017;27:198-204. [Crossref] [PubMed]
- Nordström T, Grönberg H, Adolfsson J, et al. Balancing Overdiagnosis and Early Detection of Prostate Cancer using the Stockholm-3 Model. Eur Urol Focus 2016. [Epub ahead of print].
- Roobol M. Perspective: Enforce the clinical guidelines. Nature 2015;528:S123. [Crossref] [PubMed]
- Vickers AJ. Prostate Cancer Screening: Time to Question How to Optimize the Ratio of Benefits and Harms. Ann Intern Med 2017;167:509-510. [Crossref] [PubMed]
- Miles A, Cockburn J, Smith RA, et al. A perspective from countries using organized screening programs. Cancer 2004;101:1201-13. [Crossref] [PubMed]
- Gondos A, Krilaviciute A, Smailyte G, et al. Cancer surveillance using registry data: Results and recommendations for the Lithuanian national prostate cancer early detection programme. Eur J Cancer 2015;51:1630-7. [Crossref] [PubMed]
- Grönberg H, Adolfsson J, Aly M, et al. Prostate cancer screening in men aged 50-69 years (STHLM3): a prospective population-based diagnostic study. Lancet Oncol 2015;16:1667-76. [Crossref] [PubMed]
- Nordström T, Picker W, Aly M, et al. Detection of Prostate Cancer Using a Multistep Approach with Prostate-specific Antigen, the Stockholm 3 Test, and Targeted Biopsies: The STHLM3 MRI Project. Eur Urol Focus 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Auvinen A, Rannikko A, Taari K, et al. A randomized trial of early detection of clinically significant prostate cancer (ProScreen): study design and rationale. Eur J Epidemiol 2017;32:521-7. [Crossref] [PubMed]
- Parekh DJ, Punne S, Sjöberg DD, et al. A multi-institutional prospective trial in the USA confirms that the 4Kscore accurately identifies men with high-grade prostate cancer. Eur Urol 2015;68:464-70. [Crossref] [PubMed]
- Heijnsdijk EAM, Bangma CH, Borràs JM, et al. Summary statement on screening for prostate cancer in Europe. Int J Cancer 2018;142:741-6. [Crossref] [PubMed]


