Gastric emptying after esophagectomy: comparing single therapy versus dual therapy method for pyloric drainage
Introduction
Each year in the United States, 17,000 cases of esophageal cancer are diagnosed resulting in over 16,000 deaths (1,2). In the U.S. adenocarcinoma comprises more than 60% of esophageal cancers and the incidence continues to rise, the major risk factors include smoking and excessive alcohol consumption (3-5). Esophagectomy remains a mainstay in the treatment of esophageal cancer (6). Esophagectomy is used as a first line intervention or following neoadjuvant therapy, complications occur as high as 80% in low volume centers (7,8). In an attempt to minimize those complications many surgeons have utilized minimally invasive esophagectomy (MIE) and other modifications of the surgery in the hopes of further minimizing risks (9). Common complications include anastomotic leaks, strictures, recurrent laryngeal nerve injury, dysphagia, gastric outlet obstruction and aspiration. Anastomotic leak is a particularly morbid complication occurring in up to 40% of patients with a mortality as high as 12% (10-12).
It is well established that delayed emptying is associated with morbidity resulting in increased length of stay due to complications including dysphagia and poor nutritional intake which ultimately impair long-term quality of life (13,14). As such, it is common practice to perform a drainage procedure of the pylorus to prevent delayed gastric emptying. Techniques such as botulinum toxin injection, balloon pyloroplasty and pyloromyotomy have all been examined. The literature is largely inconclusive in determining which technique is superior (15-19). Prior to this study literature regarding the combining of pyloric drainage techniques is absent. We sought to examine our experience of combining botulinum toxin with balloon dilation to reduce the incidence of gastric outlet obstruction.
Methods
In this single institution (Albany Medical Center, Albany, NY, USA) retrospective study, data was gathered from 2010 to 2016 on patients with esophageal cancer or high-grade dysplasia who underwent minimally invasive esophagectomy (MIE) consisting of laparoscopy and thoracoscopy. The study methods and data collection were approved by the Committee on Research Involving Human Subjects (IRB) protocol number 4314. Exclusion criteria included patients who did not receive Botox, pyloric dilation, or an esophagram, as well as patients who underwent esophagectomy for benign disease or were unable to undergo a minimally invasive approach.
Patients were divided into two groups. The control group (single therapy) received either balloon dilation or Botox injections and the second group (dual therapy) received both treatments.
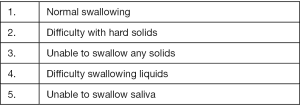
Data collection included age, gender, diagnosis, length of stay and diet tolerated at time of discharge. The post-operative esophagram was read by radiologists blinded to drainage procedure and data was collected with particular attention to any mention of delayed emptying, retained contrast, anastomotic leak, and reflux. The severity of dysphagia in these patients was quantitatively measured using a dysphagia score (Figure 1, Table 1).
Table 1
| Patient demographics | Dual therapy | Botox | Dilation |
|---|---|---|---|
| Age average | 63 | 59 | 73 |
| Sex: male [female] | 38 [8] | 11 [3] | 2 [1] |
| Squamous cell carcinoma | 7 | 4 | 0 |
| Adenocarcinoma | 36 | 6 | 3 |
| Benign (acalasia, high grade dysplasia) | 3 | 4 | 0 |
| Totals | 46 | 14 | 3 |
The injections and the dilations were performed during the MIE. The balloon dilation was performed endoscopically using a 20 mm CRETM balloon dilator following induction of general anesthesia. The balloon was inflated to six atmospheres for a duration of 5 minutes. The Botox injection was completed after mobilization of the conduit. Two hundred units of Botox mixed in 5cc of normal saline were injected into the pylorus via an extraluminal approach as we have previously described (9).
The need for prolonged nutritional support was assessed by the clinic notes from the first post-operative visit, comparing those that had their feeding tubes removed with patients requiring additional tube feeds after the first post-operative visit.
The data comparing the two groups was analyzed using STATA 14.0 statistic software. Chi square analysis and Fisher’s exact tests were used to compare categorical variables.
Results
Seventy nine consecutive esophagectomies at Albany Medical Center were identified. Two were excluded for alternative methods of esophagectomy such as robotic or open approach. Six patients did not have a post-operative esophagram while one patient had no documented pyloric drainage procedure. Seven patients were excluded for benign disease or gastric cancer.
Sixty three patients met the inclusion criteria and thus underwent retrospective chart review. The dual therapy group included 46 (73%) patients. The single therapy group included 17 (27%) of which 14 (22%) received Botox alone and 3 (5%) underwent dilation alone. The average age of patients in this study was 63; 75% of whom were males. The majority (75%) of pathology was adenocarcinoma (Figure 2).
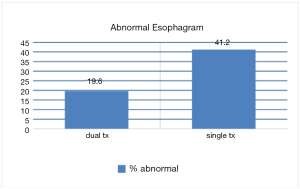
Esophagram showed delayed gastric emptying in 9 (20%) in the dual therapy group and 7 (41%) in the single therapy group who underwent Botox only (P=0.08). There was no delayed gastric emptying observed among the 3 patients who underwent dilation only (Figure 3).
No difference was observed in the post-operative leak rates. Of all 63 patients included in the study, anastomotic leak was identified in a total of 4 (6%) patients. In the single therapy group, 1 of 17 patients (6%) experienced an anastomotic leak and 3 (4%) of the 46 patients in the dual therapy group experienced an anastomotic leak (P=0.8).
Readmission was noted in 15 (33%) of 46 patients in the dual therapy group within the first 30 days, compared to 6 (35%) of the 17 patients in the single therapy group, although this difference was not significant.
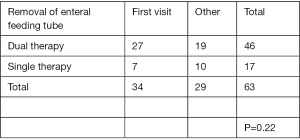
Regarding nutritional supplement, 27 of 46 patients (59%) of the dual therapy group had the feeding tube removed at the first post-operative visit versus 7 of 17 (42%) patients in the single therapy group (P=0.22) (Figure 4).
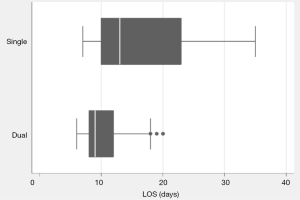
The median length of stay in the single therapy group was 16 days (range, 2–35 days) compared to 10 days (range, 6–20 days) in the dual therapy group (P=0.034). The single therapy group had 4 patients with a length of stay greater than 21 days (range, 23–35 days) while 1 patient in the dual therapy group did. Finally, one patient was excluded in the single therapy group who had a LOS of 41 days as this was a clear outlier in the data set (Figure 5).
Discussion
Delayed gastric emptying can lead to aspiration, dietary restrictions, dysphagia and reflux. These issues alone or in combination can complicate the post-operative course, increase length of stay, and worsen quality of life. No gold standard exists, and the literature is inconclusive regarding ideal management of the pylorus. Our study sought to assess the benefit of dual pyloric drainage procedures (9,17-22).
Postoperative delayed gastric emptying occurs in 15–30% of esophagectomy patients. Traditionally gastric emptying procedures such as pyloromyotomy and pyloroplasty were used . These procedures are not without risks including leak, bleeding, stricture, and death. A large study by Fok et al. (23) demonstrated a significant reduction in gastric transit time in patients who underwent emptying procedure, as documented by nuclear emptying scan. In this study patients who underwent an emptying procedure had an emptying time of 6.6 minutes compared 24.3 minutes (P<0.001) in patients who did not undergo an emptying procedure. Urshel et al. (24) published a large meta-analysis in 2002 of 553 patients. Early complications related to delayed gastric emptying were reduced if pyloroplasty was performed (relative risk, 0.018; P=0.046) (9,25-27).
Although benefits have been demonstrated from emptying procedures it remains difficult to define absolute benefit. Simply performing an emptying procedure does not ensure prompt emptying. Many variables exist which may influence emptying postoperatively, most notably conduit size, denervation of the vagus, and hiatal obstruction. In our institution we have chosen to continue performing drainage procedures. In 2007 we initially published our data using botulinum (5). In 2009 we published a larger series of botulinum toxin injection and demonstrated 43 of 45 (96%) had no delayed gastric emptying (9,18,19). Two patients had delayed gastric emptying both requiring intervention before discharge. There was one aspiration event in the entire group. During this study we recognized the value of prompt emptying and also that Botox can fail. The current study added balloon dilation in the hopes of further optimizing emptying and reducing failure of Botox injection alone.
Miller et al. reported a large retrospective series with open procedures and found no difference in emptying between the three groups pyloroplasty, pyloromyotomy, and botulin toxin injection (P=0.14) (28). The study found that Botox injection was associated with shorter operative time but an increase need for repeated endoscopy.
We utilized esophagram, obtained prior to beginning oral intake, as an objective measure of gastric outlet obstruction. Blind radiological interpretation of these contrast studies suggested that those in the dual therapy group had improved emptying that was trending toward significance when compared to the single study group, evidenced by delayed gastric emptying in 9 (20%) versus 7 (41%) (P=0.08).
Our results suggested the dual therapy group had a significantly shortened length of stay of (10 versus 16 days when compared to the single therapy group (P=0.034). We attributed this difference to a relative reduction in gastric outlet obstruction. Less emptying delay translates into less dysphagia, less need for nutritional support, and shorter overall length of stay. Combining the two relatively simple and low risk procedures of balloon dilation and Botox injection intraoperatively did not significantly extend the operative time. Both can be performed in minutes, and our preference is to scope the patient immediately prior to incision and dilate for 5 minutes.
Additional nutritional support via jejunostomy feedings was used as an indirect marker reflecting a higher dysphagia score attributable to delayed gastric emptying. Although not statistically significant (P=0.22), we observed that a higher percentage of patients in the dual therapy group 27 (59%) enjoyed freedom from prolonged jejunostomy feeding compared to the single therapy group 7 (42%).
The limitations of this study include the inherent bias present in nonrandomized retrospective single center studies. Although considered a high volume center, data obtained from one center may not be applicable in other patient populations. The procedures were performed minimally invasively however there are multiple techniques and various approaches to this procedure. Challenges exist measuring outcomes such as emptying. We choose to have two blinded radiologists separately read the contrast studies. This was an attempt to establish an objective measure of emptying. We find esophagram to be very helpful in patient management when prompt emptying is identified. It should be noted that in cases with delayed radiographic emptying many of these patients do well and not all have clinically relevant delayed emptying.
Conclusions
Anastomotic leak is a well-recognized complication of esophagectomy (5-7). The anastomotic leak rates in our study were less than what is frequently reported. (dual therapy =4%; single therapy =5.9%). We believe delayed gastric emptying is a significant risk for both clinical and sub-clinical anastomotic failure. Furthermore, in the case of anastomotic leaks, delayed emptying can contribute to longer time to heal (24,25).
Pyloric drainage procedures during esophagectomy have value for patients. In some centers intervention with Botox and balloon dilation at the time of esophagectomy may be justified to reduce risks and time associated with traditional procedures. The ease with which these procedures are performed compared to the more traditional pyloromyotomy and pyloroplasty, particularly in the minimally invasive surgery era justifies their use.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Ghulam Abbas) for the series “Minimally Invasive Esophageal Surgery” published in Shanghai Chest. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2020.02.07). The series “Minimally Invasive Esophageal Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study methods and data collection were approved by the Committee on Research Involving Human Subjects (IRB) protocol number 4314. Individual informed consent was waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bollschweiler E, Wolfgarten E, Gutschow C, et al. Demographic variations in the rising incidence of esophageal adenocarcinoma in white males. Cancer 2001;92:549-55. [Crossref] [PubMed]
- Li B, Zhang J-H, Wang C, et al. Delayed gastric emptying after esophagectomy for malignancy. J Laparoendosc Adv Surg Tech A 2014;24:306-11. [Crossref] [PubMed]
- Asti E, Lovece A, Bonavina L. Thoracoscopic implant of neurostimulator for delayed gastric conduit emptying after esophagectomy. J Laparoendosc Adv Surg Tech A 2016;26:299-301. [Crossref] [PubMed]
- Antonoff MB, Puri V, Meyers BF, et al. Comparison of pyloric intervention strategies at the time of esophagectomy: is more better? Ann Thorac Surg 2014;97: 1950-7; discussion 1657-8.
- Brown LM, Devesa SS. Epidemiologic trends in esophageal and gastric cancer in the United States. Surg Oncol Clin N Am 2002;11:235. [Crossref] [PubMed]
- Price TN, Nichols FC, Harmsen WS, et al. CA comprehensive review of anastomotic technique in 432 esophagectomies. Ann Thorac Surg 2013;95:1154-60; discussion 1160-1. [Crossref] [PubMed]
- Seely AJ, Ivanovic J, Threader J, et al. Systematic classification of morbidity and mortality after thoracic surgery. Ann Thorac Surg 2010;90:936-42. [Crossref] [PubMed]
- Briel JW, Tamhankar AP, Hagen JA, et al. Prevalence and risk factors for ischemia, leak, and stricture of esophageal anastomosis: gastric pull-up versus colon interposition. J Am Coll Surg 2004;198:536-41. [Crossref] [PubMed]
- Fuchs HF, Broderick RC, Harnsberger CR, et al. Intraoperative Endoscopic Botox Injection During Total Esophagectomy Prevents the Need for Pyloromyotomy or Dilatation. J Laparoendosc Adv Surg Tech A 2016;26:433-8. [Crossref] [PubMed]
- Eldaif SM, Lee R, Adams KN, et al. Intrapyloric botulinum toxin increases postoperative esophagectomy complications. Ann Thorac Surg 2014;97:1959-64; discussion 1964-5.
- Akkerman RD, Haverkamp L, Hillegersberg RV, et al. Surgical techniques to prevent delayed gastric emptying after esophagectomy with gastric interposition: a systematic review. Ann Thorac Surg 2014;98:1512-9. [Crossref] [PubMed]
- Bailey SH, Bull DA, Harpole DH, et al. Outcomes after esophagectomy: a ten-year prospective cohort. Ann Thorac Surg 2003;75:217-22. [Crossref] [PubMed]
- Bagheri R, Fattahi SH, Haghi SZ, et al. Botulinum toxin for prevention of delayed gastric emptying after esophagectomy. Asian Cardiovasc Thorac Ann 2013;21:689-92. [Crossref] [PubMed]
- Datta J, Williams N, Dempsey D J, et al. Rescue pyloroplasty for refractory delayed gastric emptying following esophagectomy. Surgery 2014;156:290-7. [Crossref] [PubMed]
- Martin JT, Federico JA, Mckelvey AA, et al. Prevention of delayed gastric emptying after esophagectomy: a single center’s experience with botulinum toxin. Ann Thorac Surg 2009;87:1708-13; discussion 1713-4.
- Kent MS, Pennathur A, Fabian T, et al. A pilot study of botulinum toxin injection for the treatment of delayed gastric emptying following esophagectomy. Surg Endosc 2007;21:754-7. [Crossref] [PubMed]
- Swanson EW, Swanson SJ, Swanson RS. Endoscopic balloon dilatation obviates the need for pyloroplasty at esophagectomy. Surg Endosc 2012;26:2023-8. [Crossref] [PubMed]
- Lanuti M, DeDelva P, Morse CR, et al. Management of delayed gastric emptying after esophagectomy with endoscopic balloon dilatation of the pylorus. Ann Thorac Surg 2011;91:1019-24. [Crossref] [PubMed]
- Arya S, Markar SR, Karthikesalingam A, et al. The impact of pyloric drainage on clinical outcome following esophagectomy: a systematic review. Dis Esophagus 2015;28:326-35. [Crossref] [PubMed]
- Visbal AL, Allen MS, Miller DL, et al. Ivor Lewis esophagogastrectomy for esophageal cancer. Ann Thorac Surg 2001;71:1803-8. [Crossref] [PubMed]
- Gaur P, Swanson SJ. Should we continue to drain the pylorus in patients undergoing an esophagectomy? Diseases Esophagus 2014;27:568-73. [Crossref] [PubMed]
- Biere SS, Maas KW, Cuesta MA, et al. Cervical or thoracic anastomosis after esophagectomy for cancer: a systematic review and meta-analysis. Dig Surg 2011;28:29-35. [Crossref] [PubMed]
- Fok M, Cheng SW, Wong J. Pyloroplasty versus no drainage in gastric replacement of the esophagus. Am J Surg 1991;162:447-52. [Crossref] [PubMed]
- Urshel J, Blewett C, Young J, et al. Pyloric Drainage (Pyloroplasty) or no drainage in gastric reconstruction after esophagectomy: a meta-analysis of randomized control trials. Dig Surg 2002;19:160-4. [Crossref] [PubMed]
- Lee JI, Choi S, Sung J. A flow visualization model of gastric emptying in the intrathoracic stomach after esophagectomy. Ann Thorac Surg 2011;91:1039-45. [Crossref] [PubMed]
- Harustiak T, Pazdro A, Snajdauf M, et al. Anastomotic leak and stricture after hand-sewn versus linear-stapled intrathoracic oesophagogastric anastomosis: single-centre analysis of 415 oesophagectomies. Eur J Cardiothorac Surg 2016;49:1650-9. [Crossref] [PubMed]
- Huang Q, Zhong J, Yang T, et al. Impacts of anastomotic complications on the health-related quality of life after esophagectomy. J Surg Oncol 2015;111:365-70. [Crossref] [PubMed]
- Eldif S, Lee R, Adams K, et al. Intrapyloric botulinum injection increases postoperative esophagectmy complications. AnnThorac Surg 2014;97:1959-64. [Crossref]
Cite this article as: Decker C, Burke C, Olutola O, Ata A, Nabagiez J, Fabian T. Gastric emptying after esophagectomy: comparing single therapy versus dual therapy method for pyloric drainage. Shanghai Chest 2020;4:37.