Compliance to self-monitoring of blood glucose among patients with type 2 diabetes mellitus and its influential factors: a real-world cross-sectional study based on the Tencent TDF-I blood glucose monitoring platform
Introduction
In recent years, the prevalence of type 2 diabetes mellitus (T2DM) has been rising with the change of lifestyle, living environment, and accelerated aging process (1,2). According to the International Diabetes Federation (IDF), the global diabetes prevalence estimate was 8.8% in 2015, and the number of people with diabetes reached 415 million people. In the high-income countries, T2DM accounts for about 87–91% of all diagnosed cases of diabetes. Diabetes kills over 5 million people every year, and most of them died of diabetic complications (3). Some studies including the UK Prospective Diabetes Study (UKPDS) and the Diabetes Control and Complications Trial (DCCT) have confirmed that good blood sugar control could effectively reduce the risk of diabetic complications (4,5). Thus, blood glucose monitoring has become essential for evaluating diabetic patients, developing a reasonable hypoglycemic regimen, reflecting the effectiveness of hypoglycemic treatment, and guiding treatment adjustment. Self-monitoring of blood glucose (SMBG) has been recommended for all diabetic patients in guidelines released by IDF, American Diabetes Association (ADA), and many other organizations (6,7).
Studies have revealed that SMBG can significantly improve metabolic control in T2DM patients and may reduce diabetes-related endpoint events (6,8). However, the SMBG implementation is far from satisfactory worldwide. For instance, the International Diabetes Management Practices Study (IDMPS) found that the rate of SMBG use was only 29.7%, 35.7%, and 38.5% among T2DM patients in Asia, Eastern Europe, and Latin America (9). Patients’ SMBG compliance is an important factor in determining the performance of SMBG. Thus, it is particularly important to identify the patients’ SMBG compliance and its influential factors. Although a number of previous studies have surveyed the patients’ SMBG compliance and analyzed the potential factors that might affect SMBG compliance, these studies were mainly based on questionnaires and the results were often affected by a variety of human factors such as memory and emotion and thus could not reflect the real-world SMBG compliance (10-12).
In our current study, the real-world SMBG use among T2DM patients was automatically recorded in a real-time manner by using a blood glucose monitoring platform (TDF-I, Tencent, China), and SMBG compliance and its influential factors were analyzed accordingly (Figure 1).

Methods
Subjects
In this prospective study, 120 endocrinologists or general physicians who were involved in diabetes management were recruited via DXY.cn (website: www.dxy.cn/bbs/topic/31756300) from May to December 2015, and via these doctors 500 adults (≥18 years of age) patients with T2DM were randomly selected. After the enrollment of these patients, a uniform questionnaire was used to record the patients’ clinical features including gender, age, body mass index (BMI), income, educational background, hypertension, and histories of cardiovascular and cerebrovascular diseases.
The inclusion criteria of T2DM patients were based on the diagnostic criteria of T2DM in the Chinese Guidelines on the Management of Type 2 Diabetes Mellitus (2013 edition), i.e., fasting plasma glucose (FPG) ≥7.0 mmol/L or 2 h postprandial plasma glucose (2hPPG) ≥11.0 mmol/L. The exclusion criteria for this study were: (I) younger than 18 years of age; (II) unconscious or unable to learn how to use the blood glucose meter; (III) accompanied by other major diseases such as malignancies, end-stage liver disease, or kidney disease; and (IV) with an expected survival of less than 90 days. This study strictly followed the Declaration of Helsinki on medical protocol and ethics, and all patients signed the informed consents.
Blood glucose monitoring method and definition of SMBG compliance
The blood glucose monitoring conditions within 90 days after patient enrollment were recorded. The blood glucose meters used by all patients was TDF-I intelligent blood glucose meter (Tencent, China), and the test strips were based on glucose oxidase technique, with double electrodes to ensure measurement accuracy. The device has passed the ISO2013 quality system certification. Unlike the conventional portable glucose meters, the TDF-I intelligent blood glucose meter has built-in MTK6571 dual core CPU and 512Mb+4G memory, with own GSM SIM card for network connection, which allows the synchronization of blood glucose monitoring data to patient management platform.
Patients’ SMBG frequency was determined by the physicians based on the guidelines for blood glucose monitoring [e.g., Chinese Guidelines on Clinical Application of Blood Glucose Monitoring (2015 edition)] (13) and on individual patient’s blood glucose level, blood glucose variability, history of medical visits, history of medication, and course of disease. Poor compliance was defined as the average weekly SMBG frequency over 90 days was below the criteria established by the physicians, and otherwise the patients were regarded as with good compliance.
Statistical analysis
Kolmogorov-Smirnov method was used to assess whether the continuous variables were normally distributed. The differences in the continuous variables between two groups were analyzed using independent t-test or Mann-Whitney U test. Categorical data were compared using chi-square test; for categorical variables with a hierarchical structure, rank transformation was performed firstly before Mann-Whitney U test. Multivariate logistic regression analysis was performed to analyze the effect of each potential variable on patients’ SMBG compliance. All the statistical processing was completed in SPSS 22.0 software and GraphPad Prism 6.0 software. A P value of <0.05 was considered statistically significant.
Results
Clinical features and SMBG compliance of the patients
Totally 415 T2DM patients entered the final analysis. The clinical features of these subjects are summarized in Table 1. It was found that 236 T2DM patients (57.6%) had good T2DM compliance.
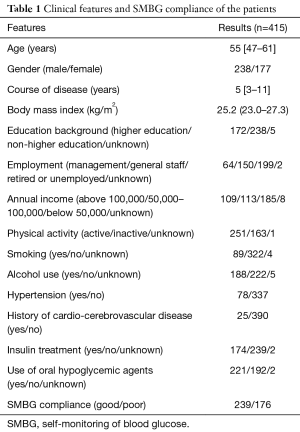
Full table
Factors affecting SMBG compliance of patients
To identify the factors affecting SMBG compliance of patients, we compared the clinical features of patients with good SMBG compliance and those with poor SMBG compliance. As shown in Table 2, age, sex, BMI, history of hypertension, history of cardiovascular disease, education background, income status, employment, and insulin treatment were not associated with SMBG compliance (P>0.05). Only the duration of diabetes mellitus and use of oral hypoglycemic agents were correlated with patients’ SMBG compliance (P<0.01).
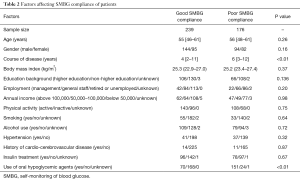
Full table
Multivariate logistic regression analysis was further applied to assess the effects of the duration of diabetes mellitus and use of oral hypoglycemic agents on SMBG compliance among the enrolled T2DM patients. It was found that both two factors were independently correlated with the patients’ SMBG compliance (Table 3). Longer duration of diabetes was associated with poorer SMBG compliance among the T2DM patients (for each 1-year extension, OR =0.96; 95% CI: 0.92–1.00); besides, patients who had used oral hypoglycemic agents had poorer SMBG compliance too (OR =16.16; 95% CI: 9.54–27.36).

Full table
Discussion
In our current study, the real-world SMBG use among T2DM patients was recorded by using a blood glucose monitoring platform (TDF-I, Tencent, China), it was found that only 57.6% of patients had good SMBG compliance. Multivariate logistic regression models showed that only the duration of T2DM and the use of oral antidiabetic agents were independently associated with SMBG compliance; more specifically, patients with longer course of disease had poorer SMBG compliance, and those had used oral antidiabetic agents had poorer SMBG compliance.
Data from 67 major centers in the United States indicated that, regardless of patient age or treatment, a higher frequency of SMBG use was associated with lower glycated hemoglobin (HbA1c) value (14). Thus, it is particularly important to identify the factors that affect patients’ SMBG compliance. However, most previous studies (10-12,15-18) on SMBG compliance were questionnaire-based, which could not perfectly reflect the real-world situations. In our current study, the monitoring platform could record and store the patients’ SMBG use in a real-time manner and thus restore the real-world SMBG situations; furthermore, it can avoid impacts of subjective interference factors such as memory, personal emotion, and concealment, which are common in questionnaire-based surveys. We found that 57.6% of T2DM patients had good SMBG compliance. While the definition of SMBG compliance may differ among studies, the poor SMBG compliance among T2DM patients in our study was consistent with the findings of many other studies (16,18,19). Thus, there is still a long way to go to further improve the patients’ compliance to SMBG.
We also found that SMBG compliance was associated with duration of diabetes and use of oral antidiabetic drugs: patients with longer course of diabetes had poorer SMBG compliance, besides, patients who had used oral antidiabetic drugs had poorer SMBG compliance too. The poor compliance in patients with long course of disease may be explained by the fact that patients tend to have negative attitude towards the disease along with the prolongation of the course of disease. Abubakari et al. concluded that patients’ negative perceptions of disease and confidence in disease control were important predictors of diabetes self-management (15). The poor compliance among patients under oral antidiabetic medication may be related to unrealistic SMBG recommendations proposed by clinicians under different treatment protocols. According to Metcalfe et al., there appeared to be relatively large under-dispensing of SMBG in patients requiring insulin and a high over-dispensing in those using oral drug alone (20).
In addition, in our current study we also found that T2DM patients’ SMBG compliance was not correlated with age, gender, BMI, high education level, income, employment, physical activity, smoking, alcohol use, history of hypertension, history of cardio-cerebrovascular disease, and insulin treatment. However, some questionnaire-based studies had conflicting findings. Li et al found that higher income was independently correlated with better SMBG compliance (18). Charity et al. found that payment for glucose meter was associated with the poor compliance to SMBG program (19), while O’Neil et al. concluded economic hardship was not an associated factor of SMBG in diabetic patients (17). It is speculated that these controversies might be caused by both the research design (questionnaire-based or real-world recording) and the definition of SMBG compliance.
However, our study had some limitations. Considering the operational feasibility, we only collected the information on SMBG use over 90 days after enrollment but did not collect blood glucose-related data such as postprandial blood glucose, glycosylated hemoglobin, and hypoglycemia. In our future studies we will further collect these information and optimize data analysis. Furthermore, by using the blood glucose monitoring platform (TDF-I, Tencent, China), we will further realize mobile health care to remind patients of SMBG use and medication in real time, so as to evaluate the effectiveness of mobile platforms in increasing SMBG compliance and integrated diabetes management.
In summary, we for the first time used an intelligent blood glucose meter to record the SMBG use in T2DM patients and reflected the real-world SMBG implementation in a real-time manner; furthermore, we accurately analyzed the influential factors of SMBG compliance. It was found that only 57.6% of T2DM patients had good SMBG compliance; more specifically, patients with longer duration of diabetes had poorer SMBG compliance, besides, patients who had used oral antidiabetic drugs had poorer SMBG compliance too. Thus, for patients with a longer course of disease and/or under oral antidiabetic medication, interventions such as patient education should be adopted to increase the SMBG compliance.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study strictly followed the Declaration of Helsinki on medical protocol and ethics, and all patients signed the informed consents.
References
- Werfalli M, Engel ME, Musekiwa A, et al. The prevalence of type 2 diabetes among older people in Africa: a systematic review. Lancet Diabetes Endocrinol 2016;4:72-84. [Crossref] [PubMed]
- Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults. JAMA 2013;310:948-59. [Crossref] [PubMed]
- IDF. Diabetes Atlas. 7th edition. Available online: http://www.diabetesatlas.org
- Nasr CE, Hoogwerf BJ, Faiman C, et al. United Kingdom Prospective Diabetes Study (UKPDS). Effects of glucose and blood pressure control on complications of type 2 diabetes mellitus. Cleve Clin J Med 1999;66:247-53. [Crossref] [PubMed]
- The Diabetes Control and Complications Trial (DCCT). Design and methodologic considerations for the feasibility phase. The DCCT Research Group. Diabetes 1986;35:530-45. [Crossref] [PubMed]
- Guideline on Self-Monitoring of Blood Glucose in Non-Insulin Treated Type 2 Diabetes. Brussels: International Diabetes Federation; 2009.
- American Diabetes Association. Standards of Medical Care in Diabetes—2017 Summary of Revisions. Diabetes Care 2017;40:S4-5. [Crossref] [PubMed]
- Guerci B, Drouin P, Grangé V, et al. Self-monitoring of blood glucose significantly improves metabolic control in patients with type 2 diabetes mellitus: the Auto-Surveillance Intervention Active (ASIA) study. Diabetes Metab 2003;29:587-94. [Crossref] [PubMed]
- Chan JC, Gagliardino JJ, Baik SH, et al. Multifaceted determinants for achieving glycemic control: the International Diabetes Management Practice Study (IDMPS). Diabetes Care 2009;32:227-33. [Crossref] [PubMed]
- Polonsky WH, Fisher L, Hessler D, et al. A survey of blood glucose monitoring in patients with type 2 diabetes:are recommendations from health care professionals being followed? Curr Med Res Opin 2011;27 Suppl 3:31-7. [Crossref] [PubMed]
- Larkin AT, Hoffman C, Stevens A, et al. Determinants of adherence to diabetes treatment. J Diabetes 2015;7:864-71. [Crossref] [PubMed]
- Kristensen LJ, Thastum M, Mose AH, et al. Psychometric evaluation of the adherence in diabetes questionnaire Diabetes Care 2012;35:2161-6. [Crossref] [PubMed]
- Chinese Diabetes Society. Clinical application guideline of blood glucose monitoring in China (2015). Chin J Diabetes Mellitus 2015;7:603-13.
- Hoey H, Mlinac A, Tran CT, et al. 5th Annual Symposium on Self-monitoring of blood glucose(SMBG) applications and beyond, May 3-5, 2012, Dublin, Ireland. Diabetes Technol Ther 2012;14:1155-73. [Crossref] [PubMed]
- Abubakari AR, Cousins R, Thomas C, et al. Sociodemographic and Clinical Predictors of Self-Management among People with Poorly Controlled Type 1 and Type 2 Diabetes: The Role of Illness Perceptions and Self-Efficacy. J Diabetes Res 2016;2016:6708164. [Crossref] [PubMed]
- Al-Keilani MS, Almomani BA, Al-Sawalha NA, et al. Self-monitoring of blood glucose among patients with diabetes in Jordan: Perception, adherence, and influential factors. Diabetes Res Clin Pract 2017;126:79-85. [Crossref] [PubMed]
- O'Neil A, Williams ED, Browne JL, et al. Associations between economic hardship and markers of self-management in adults with type 2 diabetes: results from Diabetes MILES - Australia. Aust N Z J Public Health 2014;38:466-72. [Crossref] [PubMed]
- Yuan L, Guo X, Xiong Z, et al. Self-monitoring of blood glucose in type 2 diabetic patients in China: current status and influential factors. Chin Med J (Engl) 2014;127:201-7. [PubMed]
- Wambui Charity K, Kumar AM, Hinderaker SG, et al. Do diabetes mellitus patients adhere to self-monitoring of blood glucose (SMBG) and is this associated with glycemic control? Experiences from a SMBG program in western Kenya. Diabetes Res Clin Pract 2016;112:37-43. [Crossref] [PubMed]
- Metcalfe S, Moodie P, Norris H, et al. Self-monitoring blood glucose test strip use with diabetes medicines in people with types 1 and 2 diabetes in New Zealand. N Z Med J 2014;127:48-62. [PubMed]
Cite this article as: Hu ZD, Zhang KP, Huang Y, Zhu S. Compliance to self-monitoring of blood glucose among patients with type 2 diabetes mellitus and its influential factors: a real-world cross-sectional study based on the Tencent TDF-I blood glucose monitoring platform. mHealth 2017;3:25.


