Advantages of wound retractor device versus rigid trocar at camera port in video-assisted thoracic surgery—a single institution experience
Introduction
During video assisted thoracic surgery (VATS), scope and instruments are inserted into the chest wall through separate holes also known as “ports”. To allow an easy instrument insertion through the ports, surgeons usually use rigid trocars (1,2).
Common thoracic trocars consist of a blunt-tipped obturator and a threaded sleeve with a shroud at its proximal end to protect against foreign materials entering the chest cavity, and for instrument stabilization. The cannula (or sleeve) is usually rigid and changes in size ranging from 5 to 15 mm. Once inserted into a free space in the chest cavity, the threaded sleeve is turned clockwise until securely seated in the tissue. The threaded sleeve will grip tissue to reduce slippage during instrument manipulation. In our opinion, rigid trocar presents some technical disadvantages due to its own structure. First, the cannula trocar, when inserted in the intercostal space, makes a pressure on surrounding tissue, resulting in a likely injury of the intercostal nerve. This may determine a postoperative neuritis and increase acute and chronic pain incidence. Second, since the sleeve is long and rigid, the movement of thoracoscopic devices on their fulcrum is very demanding when an extreme acute angle with the chest wall is needed. This determines a reduction in devices maneuverability and precision, and an increasing intercostal nerve compression when an extreme angulation is reached. Therefore, although VATS reduces postoperative chest pain, some patients complain of severe intercostal pain associated with the thoracoscopic access incisions. Pain is usually more intensive in correspondence of the camera port since the scope is the only thoracoscopic device that seats in the port for all the surgical intervention long (3). Moreover, the neuritis of the camera port intercostal space could be worsened by the chest tube insertion through the same thoracostomy at the end of surgery.
On the contrary, wound retractor (WR) system, designed for laparoscopic surgery, is an instrument offering retraction and protection when an organ or specimen requires removal through a small incision (4). It is also used in VATS when a mini-thoracotomy is performed (4-6). In fact, WR, placed in the mini-thoracotomy incision, provides an atraumatic circumferential retraction, while the intercostal space is not spread and the intercostal muscles and nerves are protected; starting from here, we have already described the use of WR as camera trocar in thoracoscopic surgery (7).
Assuming that WR is less traumatic on surrounding tissue and allows better instruments movement, we decide to compare in a randomized study this device with rigid trocar with the aim to determine if WR is associated with less postoperative pain and better scope maneuverability.
Methods
The study has been approved by local Ethics Committee at our hospital (recorded with the code 2016/ST/088). Data were obtained from our division of thoracic surgery prospective data-base. All patients provided informed and written consent to make use of their personal data. From October 2016 to June 2017 at our Division of Thoracic Surgery at ASST Santi Paolo e Carlo in Milan, we enrolled 40 consecutive patients who underwent anatomical VATS resection for NSCLC (power analysis 88%; t-test for independent data; alpha err. prob. 0.05).
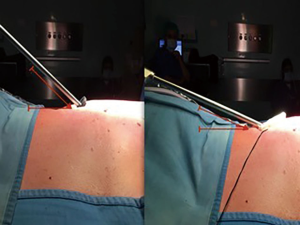
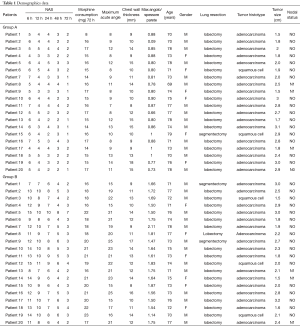
Patients were allocated in two groups (20 cases in each group): A) for those who underwent VATS resection using an extra small (4 cm) WR at camera port, B) using an 11.5-mm rigid trocar. Allocation was performed by computer-generated randomization (SAS® software). Inclusion criteria were: age >18 or <80, Karnofsky p.s. ≥70%, ASA <IV, FEV1 ≥50% predicted, WG >4,000/mm3, PST >100,000/mm3, Hb >8.5 g/dL, bilirubin <3.0 mg/dL, SGOT <2 times limits, creatinin <3.0 mg/dL, pCO2 <50 mmHg. Exclusion criteria were: age <18 or >80, pregnancy, abuse of alcool or drugs, Allergies, spinal deformities, neurologic diseases, psychiatric diseases, past thoracic surgery, pre-operative chest tube, BMI >30. All patients underwent anatomical lung resection for cancer by VATS. Surgery was always performed by triportal thoracoscopy (Copenaghen technique). The same team of surgeons always prepared a 4 cm lateral minithoracotomy in 5th intercostal space; a low anterior 1 cm camera-port was positioned at the level of the top of the diaphragm and anterior to the level of the hilum and the phrenic nerve. The third incision was 1.5 cm, positioned at the same level but more posteriorly and inferiorly from the scapula and anterior to the latissimus dorsi muscle. All patients had a wound protectors placed at the access incision. A single chest tube was always placed in the lower port. Post-operative pain management, since patient awakens, was obtained by paravertebral block (continuous infusion of naropine 3.75%, 7 mL/h) (8) and opioid intravenous patient controlled analgesia (OIVPCA: morphine 1 mg/1ml bolus, lock out 10 minutes). In order to describe and compare camera movements in the two groups, we intra-operatively recorded maximum acute angle obtained between the camera and chest wall (Figure 1), and chest wall thickness. Measurements were done intraoperatively by a surgeon using a sterile goniometer. In the trocar group, it was always left between the ribs (trocarless technique was never used). Chest wall thickness was measured through the camera port from the skin to parietal pleura by a sterile ruler. The ratio between these two measures gives an index of maneuverability based on anatomical characteristics of each patient. In order to determine in which group post-operative pain was lower we have measured it in each patient by NAS at 6, 12, 24, 48 and 72 h. NAS measurements were done by nurses at scheduled time after surgery. Since these data are subjective we also recorded the total morphine consumption at 72 h administered by PCA system (Table 1).
Full table
Statistical analysis
T test for independent data and regression linear model for repeated data were used to analyze the camera maneuverability (expressed by comparison between camera angle and thickness), use of morphine at 72 h and NAS between two groups, respectively. Shapiro-Wilk W test was used for normal data.
Results
The 2 groups were composed of 20 patients (A) and 20 patients (B). Mean patient age was 74.3 years for group A and 73.9 years for group B. No statistical significance was found in the demographic traits of the 2 groups. No patients in either group had a prior history of thoracic surgery and none had known allergies. All patients had surgery for lung cancer. The opioid (morphine) consumption was recorded after 72 h finding a statistical significance in favor of group A (P<0.0001). The maximum acute angle obtained between camera and chest wall was recorded during surgery with statistical significance in favor of group A (P<0.0001). Chest wall thickness was recorded and no statistically difference were found between the two groups (P=0.5743). Data from recording maximum angle of the camera and chest wall thickness were related in order to obtain an index of maneuverability of the camera, with a statistical significance in favor of group A (P<0.0001). NAS was recorded in every patients at 6, 12, 24, 48 and 72 h after surgery with a statistical difference between the two groups in favor of group B (P<0.0001).
Moreover, introducing WR, it was also possible to observe that the impact and damage on the skin around the port was very lower because the external ring is softer than the upper part of the trocar. This was particularly evident when the camera was extremely angled (Figure 2). We also observed that WR membrane sheath length was adaptable to the chest wall thickness, then, once fixed, reduces slippage avoiding replacements that often occurs during surgery using trocars, especially in obese patients. Lastly, WR protected the camera from small bleeding and liquid from the chest wall, avoiding repeated leans cleaning.
Discussion
Studies demonstrated that VATS surgery is better than open surgery in terms of postoperative pain. Particularly, many studies show that the incidence of “post thoracotomy pain syndrome” (PTPS) is proximal to zero (9,10). Our data improve this result, showing that pain after surgery is considerably reduced in patients who had WR during surgery, decreasing also the use of drugs against pain. Indeed, morphine consumption (11), as confirmed by our data, is clearly lower when WR is used, avoiding all collateral effect that is linked with drugs use. This result is reached because the membrane sheath enlarges gently thoracotomy edges, avoiding compression of the intercostal nerve eliminating a possible postoperative neuritis. Supporting this device, we also suggest the use of a Vaseline oil drop to make easier the camera slipping into the WR sleeve.
In addition to all positive effect listed before, our experience allows us to assert that the use of WR, increases considerably the camera angulation, because it can be adjusted to the chest wall thickness avoiding limits in the camera movements, supporting surgeons’ work and improving the view of the surgical field.
Main limitation was that, despite NAS measurement was done at scheduled time and during paravertebral continuous analgesic infusion, we did not recorded when patients self-administered the last morphine bolus. This bias could have influenced pain perception, but not the overall morphine consumption. Another bias or criticism could be that trocarless technique has not been considered in our series. However, it has been discarded since pressure against the ribs is not completely avoided and moreover it is affected by the need to clean lens several times.
We were so comfortable with this device, that our encouraging results have prompted us to introduce it in every VATS approach. Nowadays, we have definitively replaced rigid trocars with medium size WR at the utility incision and extra small size at each port.
Conclusions
The use of WR at camera port makes VATS technique even more feasible, allowing better angulation of the camera and protecting it from small bleeding and liquid from the chest wall that bother surgeon during operation. WR reduces pain allowing a patients’ better recovery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: All patients provided written informed consent, and this study was approved by the Ethical Committee of ASST Santi Paolo e Carlo, Università degli Studi di Milano (recorded with the code 2016/ST/088).
References
- Rodgers-Fischl PM, Martin JT, Saha SP. Video-Assisted Thoracoscopic versus Open Lobectomy: Costs and Outcomes. South Med J 2017;110:229-33. [Crossref] [PubMed]
- Hofmann HS. VATS - technique and indications. Chirurg 2015;86:711-21. [Crossref] [PubMed]
- Liu HF, Gao L, Liu T, et al. Comparison of acute phase reaction and postoperative stress in pigs undergoing video-assisted thoracoscopic versus thoracotomy pneumonectomy. Acta Vet Scand 2016;58:75. [Crossref] [PubMed]
- Lohsiriwat V, Lohsiriwat D. Atraumatic O-ring wound retractor reduces postoperative pain. Tech Coloproctol 2014;18:1177-8. [Crossref] [PubMed]
- Igai H, Kamiyoshihara M, Nagashima T, et al. A new application of a wound retractor for chest wall surgery. Gen Thorac Cardiovasc Surg 2013;61:53-4. [Crossref] [PubMed]
- Kamiyoshihara M, Kawatani N, Igai H. Modified application of a wound retractor for surgery in chest trauma. Asian Cardiovasc Thorac Ann 2015;23:232-4. [Crossref] [PubMed]
- Raveglia F, De Simone M, Cioffi U, et al. An Alternative Use of Wound Retractor as Camera Trocar in Thoracoscopic Surgery. Ann Thorac Surg 2016;102:e177-9. [Crossref] [PubMed]
- Cioffi U, Raveglia F, Rizzi A, et al. Paravertebral Analgesia in Video-Assisted Thoracic Surgery: A New Hybrid Technique of Catheter Placement for Continuous Anesthetic Infusion. Thorac Cardiovasc Surg 2015;63:533-4. [Crossref] [PubMed]
- Hardy-Fairbanks AJ, Mackenzie T, McCarthy M Jr, et al. A randomized controlled trial comparing two types of retractors at caesarean delivery. J Obstet Gynaecol 2017;37:1009-14. [Crossref] [PubMed]
- Palade E, Guenter J, Kirschbaum A, et al. Postoperative pain in the acute phase after surgery: VATS lobectomy vs. open lung resection - results of a prospective randomized trial. Zentralbl Chir 2014;139 Suppl 1:S59-66. [PubMed]
- Raveglia F, Rizzi A, Leporati A, et al. Analgesia in patients undergoing thoracotomy: epidural versus paravertebral technique. A randomized, double-blind, prospective study. J Thorac Cardiovasc Surg 2014;147:469-73. [Crossref] [PubMed]
Cite this article as: Raveglia F, Cioffi U, De Simone M, Rizzi A, Leporati A, Tinelli C, Chiarelli M, Baisi A. Advantages of wound retractor device versus rigid trocar at camera port in video-assisted thoracic surgery—a single institution experience. J Vis Surg 2018;4:66.