Association of body mass index with all-cause mortality in patients with diabetes: a systemic review and meta-analysis
Introduction
Overweight and obesity are clustered with many metabolic abnormalities, and the prevalence of morbid obesity is increasing in the general population worldwide (1). Obesity is a well-known risk factor for the development of cardiovascular disease (CVD) and adversely affects cardiovascular hemodynamics, structure, and function.
However, overweight or obesity, as measured by increased body mass index (BMI), which was defined as body weight (kg)/height (m2), has been shown to improve the survival in patients with established CVD such as coronary heart disease (2), stroke (3), and heart failure (4). This phenomenon was called as the obesity paradox.
Besides CVD, obesity paradox has been found in different clinical situations, such as end stage renal disease (5), advanced cancer (6), and also in patients with diabetes, which has been regarded as the coronary heart disease equivalent. The relationship between BMI and mortality in patients with diabetes has revealed various results in previous prospective studies, including a U-shaped or J-shaped association (7,8) or no clear relationship (9,10). Despite the obesity paradox in patients with CVD has been confirmed previously (11,12), this phenomenon in diabetes remains controversy since the etiology of diabetes development in different BMI category is probably not the same. The diabetic patients with lower BMI are more likely to be associated with β cell dysfunction (13), but those with higher BMI are more likely associated with insulin resistance due to adiposity. So we conducted a systematic review to summarize current evidence on the association between BMI and all-cause mortality in patients with diabetes, and to explore potential sources of heterogeneity among study results.
Method
Searching strategy
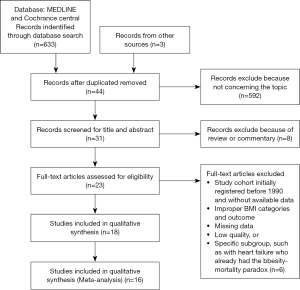
PubMed, Science Direct and Cochrane Library databases were systematically searched for studies which reported total mortality rates in relation to BMI in patients with diabetes from 1990 to 2015. Medical subject heading (MeSH) and keywords BMI, mortality, diabetes, and obesity paradox or reverse epidemiology were used to identify English literature of current studies investigating the association between BMI and all-cause mortality in patients with diabetes. The study selection process was performed according to the PRISMA statement as Figure 1. Studies that did not meet these criteria were excluded. Additional studies were identified from the references of articles retrieved and previous reviews on this topic. Studies that did not provide either effect estimates (e.g., odds ratio) for BMI and mortality or sufficient data for us to calculate them were also excluded.
Data extraction
Two reviewers (HWC and GML) independently extracted data on study design, sample size, country, year of publication, patient characteristics (e.g., sex, age), BMI categories, cause of mortality, and crude and adjusted effect measures of BMI on all-cause mortality. Effects of BMI on mortality by sex were identified if available. Specific subgroups, such as with heart failure that already had the obesity-mortality paradox were also extracted from the identified studies. Studies comparing obese and non-obese were excluded unless outcomes in the normal BMI category alone were available. To avoid eliminating studies with important data, we considered BMI levels within 2 kg/m2 of standard categories to be acceptable. We did not contact original authors for additional information. We utilized a 9-star system by Newcastle-Ottawa Scale for assessing the quality of studies (14). The meta-analysis collected publicly available data and the information was recorded in a manner in which the subjects cannot be identified, which was exempt from full review by the Institutional Review Board.
Statistical analyses
The meta-analysis was conducted using RevMan version 5.2 to perform random effect analysis by the inverse variance method. Hazard ratios (HRs) and 95% confidence intervals (CIs) (the abnormal BMI groups versus the normal weight group) were calculated and risk factor-adjusted to measure the association between abnormal BMI and the risk of all-cause mortality among patients with diabetes. Heterogeneity was examined using the Higgins I2 test. Roughly, Higgins I2 values of 25, 50, and 75% can be interpreted as indicating low, moderate, and high heterogeneity (15). For the purpose of our meta-analysis, patients were further divided into 5 groups: underweight (BMI: <18.5), normal weight (BMI: 18.5–24.9), overweight (BMI: 25–29.9), mild obesity (BMI: 30–34.9) and morbid obesity (BMI: ≥35).
Result
Study characteristics
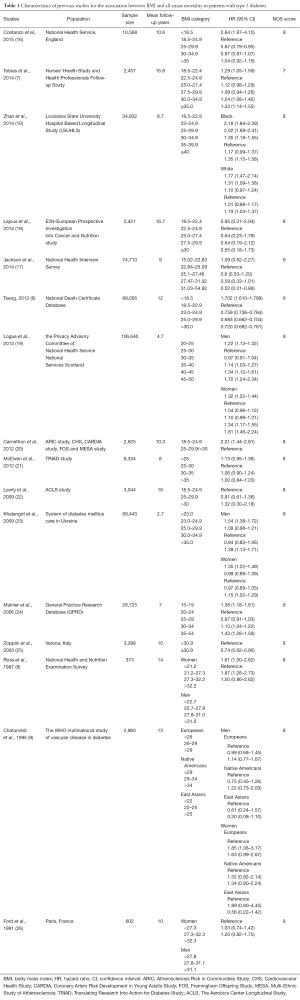
Of the 636 articles identified, 44 articles met the inclusion criteria. Overall, 16 cohort studies with a total number of 385,925 patients were included in the analysis (6-10,16-26). Study design, patients’ characteristics, mean follow-up years, BMI category and its effect on mortality are summarized in Table 1. Among these selected studies, one enrolled Asian patients (6), and the others were White patients. Three studies enrolled only female patients (7,18,21). The mean follow-up period was from 2.7 years (23) to 16 years (22). In all studies, the HRs were obtained by the adjustments for traditional vascular risk factors, and in some studies, the HRs were additionally controlled for other confounding factors, such as duration of diabetes (6,16,17,21,22,24,25), diabetic complications (9,21), menopause status (7,18), comorbid condition (16,18), and glomerular filtration rate (10).
Full table
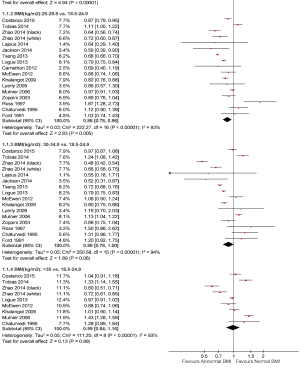
The association of BMI with all-cause mortality in the overall cohort
Figure 2 shows the association of each BMI category with all-cause mortality in the overall cohort. As compared to the normal weight, the underweight had higher risk of all-cause mortality (HR: 1.59, 95% CI: 1.32–1.91). In contrast, both the overweight and the mild obesity were associated with lower risk of mortality (HR: 0.86, 95% CI: 0.78–0.96, and 0.88, 95% CI: 0.78–1.00, respectively). However, the morbid obesity was not associated with all cause-mortality (HR: 0.99, 95% CI: 0.84–1.16). Notably, the heterogeneity for all of the analyses was significant (all I2 >75%; P values <0.05).
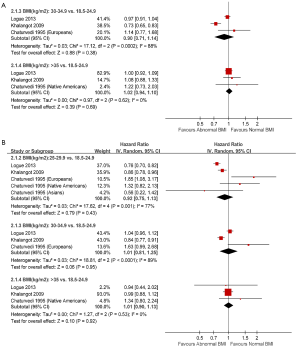
The sex specific association of BMI with all-cause mortality
Figure 3 shows the sex-specific association between BMI and all-cause mortality. There were only three papers included in the sex specific analyses (24-26). In reference to the normal weight, the overweight was associated with lower risk of all-cause mortality in males (HR: 0.82, 95% CI: 0.74–0.90), but not in females (HR: 0.92, 95% CI: 0.75–1.13). The BMI associations were consistent between men and women. In men, both mild and morbid obesity were not associated with all-cause mortality (HR: 0.90, 95% CI: 0.71–1.14, and 1.02 95% CI: 0.94–1.10, respectively). Similarly in females, mild and morbid obesity were not associated with all-cause mortality as well (1.01, 95% CI: 0.81–1.25, and 1.01, 95% CI: 0.90–1.13, respectively). Notably, the heterogeneity for all of the analyses was significant in the overweight and mild obesity groups (all I2 >75%; P values <0.05). For the morbid obesity group, the results among studies were homogeneous (I2 =0; P values >0.1).
Discussion
In our meta-analysis, being overweight or mild obesity in patients with diabetes was associated with lower risk of mortality during long-term follow-up among these sixteen studies. Overweight and mild obesity may reduce 14% and 12% relative risk of all-cause mortality respectively. In contrast, diabetic patients with underweight had the highest risk of all-cause mortality and increased up to 59% relative risk in comparison to those with normal weight. In addition, there was no difference with regard to the risk of mortality between the morbid obesity and the normal weight. These findings suggested a U-shaped relationship between BMI and total mortality in patients with diabetes.
In previous sixteen cohort studies we included, the associations between BMI and overall mortality in patients with type 2 diabetes were inconsistent. In summary, the U-shaped relationship was reported in eleven studies (6-8,10,16,19,21-24,26). The lowest risk of mortality was found in patients with overweight in eight out of eleven studies (6-8,16,21,22,24,26), and in those with obesity in other three studies (10,19,23). In contrast, three studies found that an inverse rather than a U-shaped relationship between BMI and all-cause mortality (17,18,20). One study found that an inverse BMI association was only present in the elderly populations whereas a positive association was observed in the younger patients with diabetes (25). Moreover, one study showed that the sex difference regarding the BMI association might be affected by race/ethnicity where the overweight was associated with higher risk of all-cause mortality in Asian male patients, but inversely in Asian female patients (9).
The heterogeneity among studies in our meta-analysis suggested that the BMI associations may vary by different conditions and we should interpret the data with caution. In our analysis, several confounders may explain a considerable proportion of the heterogeneity to influence the BMI effect on overall mortality in patients with diabetes. For instance, smoking status was a notable factor to mortality, which had been mentioned in five studies with inconsistent results (7,17,23,24,26). A higher risk of mortality in current smokers or ex-smoker with comparison to non-smokers has been found in Mulnier’s and Ford’s studies (24,26). In the Tobias’s study, the U-shaped association between BMI and all-cause mortality was present in those who ever smoked, and the inverse relationship was found in those who never smoked (7). The U-shaped or inverse relationship remained unchanged in patients with diabetes after controlling for the smoking status in Khalangot’s study and Jackson’s study, respectively (17,23). Therefore, the impact of current smoking on the mortality was still inconclusive now and it needs further studies. Age, sex, and race/ethnicity may also affect the BMI association. The White population had lower mortality than other race/ethnicities which was found in Ford’s study (26). In Chaturvedi’s and Zhao’s studies (9,10), the U-shaped association existed both in Black and White patients and in Europeans and Native Americans, but not in East Asians. The age difference has been described above in Jackson’s study (17). With regard to the sex difference, males had higher risk of all-cause mortality than females in Mulnier’s study (24). In Logue’s and Khalangot’s studies, the U-shaped association existed both in males and females, but the lowest risk of mortality was found in females with overweight and males with obesity (19,23). In contrast, the Chaturvedi’s study found no significant relationship between BMI and mortality in females of different ethnic populations (11). The other possible confounders had been observed among these studies, such as diabetes duration, co-morbidities, and physical activity. The longer duration of diabetes with higher risk of mortality was demonstrated in Mulnier’s study (24). Among patients with diabetes duration less than 10 years, the nadir of U-shaped association was observed in obese patients in Khalangot’s study (23), but the inverse association rather than the U-shaped relationship between BMI and mortality was found in Jackson’s study (17). Among patients with diabetes duration more than 10 years, the nadir of U-shaped association was observed in those with overweight in Khalangot’s study (23); but in contrast, no significant relationship between BMI and mortality was present in Jackson’s study (17). Higher serum cholesterol levels, longer follow-up duration for hypertension, and lesser physical activity were found to increase all-cause mortality in patients with diabetes in Ford’s study (26). These potential confounders may affect the BMI association in diabetes and cause the heterogeneity among studies.
The mechanism of the U-shaped association in patients with diabetes was unclear. There were several possible explanations for higher risk of mortality in patients with underweight. First, being underweight in patients with diabetes may have genetic influence on β cell dysfunction, possibly leading to poor glycemic control and the related serious diabetic complications as compared with those with overweight or mild obesity. Second, patients with underweight were usually accompanied with greater burden of chronic disease and multiple comorbidities as compared with non-diabetic counterparts, which may be aggravated and caused higher risk of mortality. Third, higher prevalence of smoking and alcohol consumption in diabetic patients with underweight may contribute to adverse effects and lead to higher risk of all-cause mortality (27,28). In addition, patients with underweight may reflect a malnutrition status and thus have higher risk of mortality. For diabetic patients with morbid obesity, numerous adipokines and inflammatory mediators may be released from adiposity and play important roles in the pathogenesis of many obesity-related CVD (29). On the other hand, overweight or mild obesity was protective to mortality, and the mechanism was unknown. Possible explanations were listed as below: first, diabetic patients with overweight may have early screening of metabolic disorder and accept early treatment for the prevention for serious CVD complications, which may decrease the risk of all-cause mortality. Second, excess body mass may provide a metabolic reserve in older patients, protecting against frailty, malnutrition, and age-related sarcopenia (30,31).
There were several strengths and limitations of our study. The main strength of this meta-analysis was the comprehensive inclusion of current studies to show the relationship between BMI and all-cause mortality in patients with diabetes. And the limitations in our meta-analysis were as below. First, BMI data were collected from various methods, such as self-report or medical record in different studies, which may influence our results by misclassification of BMI. Second, most of the studies included the older population which may affect our findings by survivor bias and result in underestimation of relationship between BMI and mortality. Finally, since the heterogeneity was significant among studies, our findings were suggested to be interpreted in appropriate situations such as by age, sex, and race/ethnicity.
Conclusions
Our meta-analysis of patients with diabetes in current studies showed a U-shaped relationship between BMI and all-cause mortality. Overweight and mild obesity may be protective to the mortality in patients with diabetes. The sex-specific association showed a consistent U-shaped relationship in males but not in females. Since there was a significant heterogeneity among studies and substantial evidence regarding the confounders such as sex difference in our subgroup analysis may affect the BMI association, our findings should be interpreted according to the clinical situations.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sturm R. Increases in clinically severe obesity in the United States, 1986-2000. Arch Intern Med 2003;163:2146-8. [Crossref] [PubMed]
- Lin GM, Li YH, Lin CL, et al. Relation of body mass index to mortality among Asian patients with obstructive coronary artery disease during a 10-year follow-up: a report from the ET-CHD registry. Int J Cardiol 2013;168:616-20. [Crossref] [PubMed]
- Wohlfahrt P, Lopez-Jimenez F, Krajcoviechova A, et al. The obesity paradox and survivors of ischemic stroke. J Stroke Cerebrovasc Dis 2015;24:1443-50. [Crossref] [PubMed]
- Lavie CJ, Alpert MA, Arena R, et al. Impact of obesity and the obesity paradox on prevalence and prognosis in heart failure. JACC Heart Fail 2013;1:93-102. [Crossref] [PubMed]
- Park J, Ahmadi SF, Streja E, et al. Obesity paradox in end-stage kidney disease patients. Prog Cardiovasc Dis 2014;56:415-25. [Crossref] [PubMed]
- Tseng CH. Obesity paradox: differential effects on cancer and noncancer mortality in patients with type 2 diabetes mellitus. Atherosclerosis 2013;226:186-92. [Crossref] [PubMed]
- Tobias DK, Pan A, Jackson CL, et al. Body-mass index and mortality among adults with incident type 2 diabetes. N Engl J Med 2014;370:233-44. [Crossref] [PubMed]
- Ross C, Langer RD, Barrett-Connor E. Given diabetes, is fat better than thin? Diabetes Care 1997;20:650-2. [Crossref] [PubMed]
- Chaturvedi N, Fuller JH. Mortality risk by body weight and weight change in people with NIDDM. The WHO Multinational Study of Vascular Disease in Diabetes. Diabetes Care 1995;18:766-74. [Crossref] [PubMed]
- Zhao W, Katzmarzyk PT, Horswell R, et al. Body mass index and the risk of all-cause mortality among patients with type 2 diabetes mellitus. Circulation 2014;130:2143-51. [Crossref] [PubMed]
- Lavie CJ, McAuley PA, Church TS, et al. Obesity and cardiovascular diseases: implications regarding fitness, fatness, and severity in the obesity paradox. J Am Coll Cardiol 2014;63:1345-54. [Crossref] [PubMed]
- De Schutter A, Lavie CJ, Patel DA, et al. Obesity paradox and the heart: which indicator of obesity best describes this complex relationship? Curr Opin Clin Nutr Metab Care 2013;16:517-24. [Crossref] [PubMed]
- George AM, Jacob AG, Fogelfeld L. Lean diabetes mellitus: An emerging entity in the era of obesity. World J Diabetes 2015;6:613-20. [Crossref] [PubMed]
- GA Wells, B Shea, D O'Connell, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [Crossref] [PubMed]
- Costanzo P, Cleland JG, Pellicori P, et al. The obesity paradox in type 2 diabetes mellitus: relationship of body mass index to prognosis: a cohort study. Ann Intern Med 2015;162:610-8. [Crossref] [PubMed]
- Jackson CL, Yeh HC, Szklo M, et al. Body-Mass Index and All-Cause Mortality in US Adults With and Without Diabetes. J Gen Intern Med 2014;29:25-33. [Crossref] [PubMed]
- Lajous M, Bijon A, Fagherazzi G, et al. Body mass index, diabetes, and mortality in French women: explaining away a "paradox". Epidemiology 2014;25:10-4. [Crossref] [PubMed]
- Logue J, Walker JJ, Leese G, et al. Association between BMI measured within a year after diagnosis of type 2 diabetes and mortality. Diabetes Care 2013;36:887-93. [Crossref] [PubMed]
- Carnethon MR, De Chavez PJ, Biggs ML, et al. Association of weight status with mortality in adults with incident diabetes. JAMA 2012;308:581-90. [Crossref] [PubMed]
- McEwen LN, Karter AJ, Waitzfelder BE, et al. Predictors of mortality over 8 years in type 2 diabetic patients: Translating Research Into Action for Diabetes (TRIAD). Diabetes Care 2012;35:1301-9. [Crossref] [PubMed]
- Lyerly GW, Sui X, Lavie CJ, et al. The association between cardiorespiratory fitness and risk of all-cause mortality among women with impaired fasting glucose or undiagnosed diabetes mellitus. Mayo Clin Proc 2009;84:780-6. [Crossref] [PubMed]
- Khalangot M, Tronko M, Kravchenko V, et al. Body mass index and the risk of total and cardiovascular mortality among patients with type 2 diabetes: a large prospective study in Ukraine. Heart 2009;95:454-60. [Crossref] [PubMed]
- Mulnier HE, Seaman HE, Raleigh VS, et al. Mortality in people with type 2 diabetes in the UK. Diabet Med 2006;23:516-21. [Crossref] [PubMed]
- Zoppini G, Verlato G, Leuzinger C, et al. Body mass index and the risk of mortality in type II diabetic patients from Verona. Int J Obes Relat Metab Disord 2003;27:281-5. [Crossref] [PubMed]
- Ford ES, DeStefano F. Risk factors for mortality from all causes and from coronary heart disease among persons with diabetes. Findings from the National Health and Nutrition Examination Survey I Epidemiologic Follow-up Study. Am J Epidemiol 1991;133:1220-30. [Crossref] [PubMed]
- Howard AA, Arnsten JH, Gourevitch MN. Effect of alcohol consumption on diabetes mellitus: a systematic review. Ann Intern Med 2004;140:211-9. [Crossref] [PubMed]
- Willi C, Bodenmann P, Ghali WA, et al. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA 2007;298:2654-64. [Crossref] [PubMed]
- Mehta T, Fontaine KR, Keith SW, et al. Obesity and mortality: are the risks declining? Evidence from multiple prospective studies in the United States. Obes Rev 2014;15:619-29. [Crossref] [PubMed]
- Oreopoulos A, Kalantar-Zadeh K, Sharma AM, et al. The obesity paradox in the elderly: potential mechanisms and clinical implications. Clin Geriatr Med 2009;25:643-59. viii. [Crossref] [PubMed]
- Cherin P, Voronska E, Fraoucene N, et al. Prevalence of sarcopenia among healthy ambulatory subjects: the sarcopenia begins from 45 years. Aging Clin Exp Res 2014;26:137-46. [Crossref] [PubMed]