
Stafne’s bone defect: a case report and review of literatures
Introduction
Stafne’s bone defect (SBD) is an uncommon mandibular defect. It is usually accidentally found via radiograph during other dental treatments because patients often present no abnormal clinical symptom (1). Through panoramic radiography an ovoid or round radiolucency can be observed near the angle of mandible, usually located between the inferior alveolar nerve and the lower margin of mandible. The diagnosis of SBD is not too difficult with the help of CT and MRI, but differential diagnosis with other cyst-like lesions in mandible is needed, such as ameloblastoma, residual cyst, periapical cyst or lesions from salivary gland (2). We experienced a female patient with SBD located in the right mandible. This study aims to report and summarize clinical and radiographic features, histopathology and treatment after reviewing previously reported literatures relevant to SBD to facilitate diagnosis for clinicians in clinical practice.
Case presentation
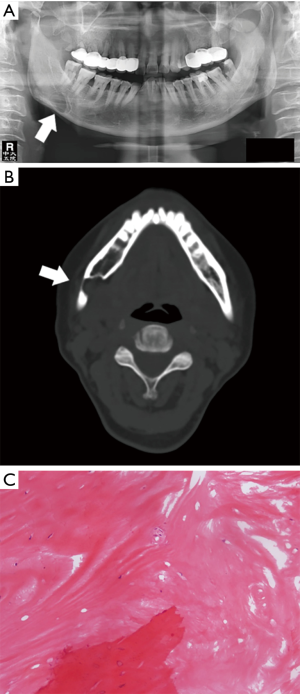
A 48-year-old female was found via panorama to have an ovoid radiolucency in her right lower jaw. The patient was referred to our clinic to treat her decayed teeth but was discovered to have this lesion without presenting any pain and numbness in the mucosa and the lip. She was hospitalized and CT scanning as well as microscopic observation on specimen obtained from surgical intervention were performed. Features such as location, size, border and margin were carefully examined. X-ray image showed a well-defined ovoid radiolucency with high-density margin (Figure 1A). The lesion was located near the angle of the right jaw. In particular, the lesion was located below the periapical area of 47 and 48, whose roots were intact without any resorption. Right inferior alveolar nerve perforated the lesion. CT image revealed that the lack of continuity of lingual cortex of the right lower jaw could be found, leaving the buccal cortex extremely thin. Besides, soft tissue could be observed in the lesion (Figure 1B). Pathological results showed that clot and bone tissue were found in the specimen obtained from surgical intervention (Figure 1C). Considering all the collected evidence, there was a diagnostic indication of SBD. At the 6-month follow-up after discharge, the patient was asymptomatic and had a good recovery.
Discussion
Epidemiology and origin
SBD is a rare lesion which was first reported in 1942 (3). The incidence is 0.1% to 0.48% in different reports (1). In fact, actual incidence of SBD may be higher than that’s reported because of the difficulty of diagnosis without radiograph in cases where patients show no any abnormal symptoms. SBD are often observed among males between 50 and 70, while a reported youngest case occurred on an 11-year-old child (4). SBD can be observed in the posterior or anterior area of the mandible and the ramus of mandible which is very much rare. The etiology of SBD remains to be uncertain. It is mostly accepted that SBD is a developmental anatomic impression caused by proliferation or translocation of adjacent structures such as salivary gland or other soft tissues.
Clinical presentation
To summarize clinical and radiographic characteristic of SBD, relevant literatures search of PubMed for cases reports of SBD was carried out. Data such as gender, age, location of the lesion, manifestation, X-ray radiography and Computed tomography (CT) was retrieved and summarized in Tables 1,2.
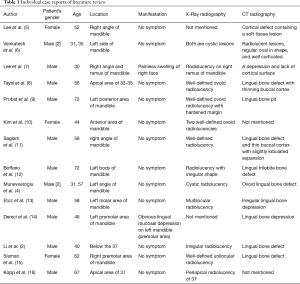
Full table

Full table
In most cases, SBD is accidentally observed via panoramic X-ray film when patients are receiving other dental treatments. There are patients who come for help because they find an obvious lingual mucosal depression on their mandible. Pain is rarely found, so as to ulceration, bleeding or fistula. In our case presentation, patient was asymptomatic, which proved that SBD was uneasy to find without the help of radiographic examination.
Diagnostic imaging
Radiographic evaluation can greatly help to diagnose SBD. In our experience, panorama can provide initial evaluation of SBD. In most cases, a well-defined ovoid radiolucency can be observed beneath the inferior alveolar nerve. Apical area of canine and premolar is the most common location of SBD in the anterior area of mandible. Anterior SBD can be easily mistaken for residual cyst, which should raise enough attention in clinical practice. History of local tooth extraction after hopeless apical infection of relevant tooth can help to diagnose residual cyst while there is usually no contact of SBD with relevant teeth. CT has the ability to show more details when it comes to the buccolingual location and provide information on whether or not the defect has perforated through buccal cortex, which 2-dimentional panorama cannot provide. Further CT scanning after speculated diagnosis of SBD from panorama to determine buccolingual position does great help to the differential diagnosis of SBD (9,11). Three-dimensional reconstruction of CT is now available to help to directly observe the spatial relationship of SBD and the inferior alveolar nerve (2,7). However, though much benefits can be brought from CT radiograph, consequent ionizing radiation is still a worrying issue in CT evaluation. MRI can not only rid patients of ionizing radiation but also help to observe the content of the defect, which is beneficial to the diagnosis of SBD. The disadvantages of MRI may be relatively high cost, discomfort feeling during the scanning and the radiographic artifacts and distortion in images. Sialography is an effective technique to determine whether there is glandular tissue in the defect, which is an important indication of the glandular sources of the lesion. But it is unsuitable for anterior SBD because submandibular glandular ducts are so tiny that imaging in the ducts is almost impossible (5,8).
Differential diagnosis
SBD should be diagnosed excluding other odontogenic or non-odontogenic cystic lesion. Dentigerous cyst can also be observed near the angle of mandible, containing the crown of an un-erupted tooth mostly occurred in the impacted wisdom tooth. Radicular cyst is obviously related to inflamed teeth which could cause relevant symptoms on teeth such as bite pain or swelling. Ameloblastoma can present near the angle of mandible. Consequent cut-shaped root resorption of teeth can provide important clue to differentiate these two diseases as SBD have no relationship to the teeth. Langerhans cell histiocyosis (LCH) can be observed below the lower molars, whose radiolucency is usually ill-circumscribed. LCH is mostly found in children in 5-15 and could cause swelling and pain on maxillofacial area. Differential diagnosis also includes other jaw lesions such as vascular malformation, non-ossifying fibroma and fibrous dysplasia, basal cell nevus syndrome and a metastasis from a primary malignant tumour from other organs.
Management
As SBD is a benign, developmental bony defect causing no any pathological changes, surgical intervention is no longer needed to treat SBD. But follow-ups on a regular basis are recommended to check whether there is radiographic enlarging tendency or any abnormal signs of the lesion.
Acknowledgments
None.
Footnote
Conflicts of Interests: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Sisman Y, Miloglu O, Sekerci AE, et al. Radiographic evaluation on prevalence of Stafne bone defect: a study from two centres in Turkey. Dentomaxillofac Radiol 2012;41:152-8. [Crossref] [PubMed]
- Li B, Long X, Cheng Y, et al. Cone beam CT sialography of Stafne bone cavity. Dentomaxillofac Radiol 2011;40:519-23. [Crossref] [PubMed]
- Stafne EC. Bone Cavities Situated Near the Angle of the Mandible. The Journal of the American Dental Association 1942;29:1969-72. [Crossref]
- Munevveroglu AP, Aydin KC. Stafne bone defect: report of two cases. Case Rep Dent 2012;2012:654839. [Crossref] [PubMed]
- Lee JI, Kang SJ, Jeon SP, et al. Stafne Bone Cavity of the Mandible. Arch Craniofac Surg 2016;17:162-4. [Crossref] [PubMed]
- Venkatesh E. Stafne bone cavity and cone-beam computed tomography: a report of two cases. J Korean Assoc Oral Maxillofac Surg 2015;41:145-8. [Crossref] [PubMed]
- Lee KH, Thiruchelvam JK, McDermott P. An Unusual Presentation of Stafne Bone Cyst. J Maxillofac Oral Surg 2015;14:841-4. [Crossref] [PubMed]
- Taysi M, Ozden C, Cankaya B, et al. Stafne bone defect in the anterior mandible. Dentomaxillofac Radiol 2014;43:20140075. [Crossref] [PubMed]
- Probst FA, Probst M, Maistreli IZ, et al. Imaging characteristics of a Stafne bone cavity--panoramic radiography, computed tomography and magnetic resonance imaging. Oral Maxillofac Surg 2014;18:351-3. [Crossref] [PubMed]
- Kim H, Seok JY, Lee S, et al. Bilateral stafne bone cavity in the anterior mandible with heterotopic salivary gland tissue: a case report. Korean J Pathol 2014;48:248-9. [Crossref] [PubMed]
- Saglam M, Salihoglu M, Sivrioglu AK, et al. Multimodality imaging of Stafne bone defect. BMJ Case Rep 2013;2013.
- Boffano P, Gallesio C, Daniele D, et al. An unusual trilobate Stafne bone cavity. Surg Radiol Anat 2013;35:351-3. [Crossref] [PubMed]
- Etoz M, Etoz OA, Sahman H, et al. An unusual case of multilocular Stafne bone cavity. Dentomaxillofac Radiol 2012;41:75-8. [Crossref] [PubMed]
- Dereci O, Duran S. Intraorally exposed anterior Stafne bone defect: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol 2012;113:e1-3. [Crossref] [PubMed]
- Sisman Y, Etoz OA, Mavili E, et al. Anterior Stafne bone defect mimicking a residual cyst: a case report. Dentomaxillofac Radiol 2010;39:124-6. [Crossref] [PubMed]
- Kopp S, Ihde S, Bienengraber V. Differential diagnosis of stafne idiopathic bone cyst with Digital Volume Tomography (DVT). J Maxillofac Oral Surg 2010;9:80-1. [Crossref] [PubMed]


