
Optimizing Anti-HER2 Therapy in early breast cancer: updates from the KRISTINE trial
Introduction
Early breast cancer which overexpresses the human epidermal growth factor receptor 2 (HER2) was once considered an inherently aggressive disease, associated with adverse outcome (1). However, systemic chemotherapy in combination with HER2-directed therapy has led to significant improvements in overall survival (OS) (2). Pathologic complete response (pCR), rigorously defined as the absence of residual cancer in breast or axillary lymph nodes following neoadjuvant (preoperative) treatment, has been considered as a valid primary study endpoint as a pCR has been linked to excellent OS (3). In combination with traditional cytotoxic chemotherapy, dual HER2 targeting with the monoclonal antibodies Trastuzumab (H) and Pertuzumab (P) has improved pCR rates (4). The antibody-drug conjugate Trastuzumab emtansine (T-DM1) is another effective option for the management of HER2-positive breast cancer. It has a favorable safety profile and combines the anti-HER2 mechanism of H with the cytotoxic agent DM1 (5). The KRISTINE study aimed to examine whether combination dual HER2 targeting with this exciting antibody-drug conjugate would be equally effective, but less toxic, than conventional cytotoxic chemotherapy for those with early HER2-positive disease (6).
Summary of the trial
The KRISTINE study was a randomized multicenter phase III trial involving 444 patients, which evaluated T-DM1 plus P and compared this to HP with Docetaxel (T) and Carboplatin (C), in patients with Stage II to III HER2-positive breast cancer. Patients were randomized to receive either neoadjuvant T-DM1+P or TCH-P for 6 cycles, followed by surgery. Anti-HER2 therapy was given on a 3 weekly schedule up to a maximum of 18 cycles. The primary efficacy endpoint was locally determined pCR (ypT0/is, ypN0). Secondary efficacy endpoints included event-free survival (EFS), invasive disease-free survival (IDFS) and OS. EFS was given as the time from randomization to progression of disease. The definition of IDFS was the time from surgery to the first documented occurrence of an IDFS event, which was defined as ‘ipsilateral invasive local recurrence, ipsilateral locoregional invasive recurrence, distant recurrence, contralateral invasive breast cancer, or death from any cause’. OS was defined as time from random assignment to death from any cause (6). As previously described, the T-DM1+P regimen resulted in a reduced rate of pCR than the conventional systemic chemotherapy–based regimen of TCH-P, (44.4% vs. 55.7%; P=0.016). In a recent update published by Hurvitz et al., it was found that patients in the TCH-P arm had a superior 3-year EFS rate (94.2% vs. 85.3%; HR, 2.61; 95% CI: 1.36–4.98) (7). This difference in EFS was mainly driven by higher rates of loco-regional progression before surgery in the T-DM1+P arm versus those receiving TCH-P, (6.7% vs. 0%). In fact, the two treatment groups had a similar risk of an IDFS event following surgery [HR, 1.11 (95% CI, 0.52 to 2.40)] (7).
In terms of toxicities, fewer Grade III or higher adverse events (13.0% vs. 64.4%) were seen with T-DM1+P pre-operatively. Taking both neoadjuvant and adjuvant phases into account, T-DM1 continued to have a better safety profile: Grade III-IV adverse events occurred in 31.8% of patients versus 67.6% in the TCH-P arm. The only Grade III-IV adverse event to occur more frequently in the T-DM1+P group was peripheral neuropathy (3.1% vs. 0.5%). Otherwise, Grade III-IV adverse events were more common in the TCH-P regimen; neutropenia (35.1% vs. 3.6%), febrile neutropenia (15.1% vs. 1.8%), diarrhea (15.5% vs. 1.8%), and anemia (11% vs. 5.8%).
Strengths
The KRISTINE study was a well-designed, randomized, multicenter, phase III trial, which facilitated the direct comparison of two neoadjuvant regimens in the management of locally advanced HER2-positive breast cancer. It was an important study that examined the novel concept of a chemotherapy-sparing regimen in this setting. The patient characteristics at baseline were well matched between the two arms and accurately reflected the patient population of interest. Importantly, random assignment was stratified by hormone receptor status, clinical stage at presentation and geographic location. The patient characteristics were representative of the real world setting: median age 49–50 years, 62.2% hormone receptor–positive disease and 83.1% of patients were stage IIA-IIIA. The trial was diverse in terms of ethnicity with 66.4% white and 25.2% Asian participants (6). The trial used rigorous definitions as defined by the standardized definitions for efficacy endpoints (STEEP) criteria. The STEEP criteria were designed to facilitate the consistent analysis of clinical trials in breast cancer, therefore allowing the performance of cross-trial comparisons and meta-analyses (8). The definition of IDFS was consistent with the STEEP criteria, except for the fact that it did not include non-breast second primary invasive cancer (6).
Although the patients who received TCH-P had higher rates of pCR, 44% of patients in the T-DM1+P arm achieved a pCR without having received any traditional cytotoxic chemotherapy (6). Thus, there is a cohort of patients who are likely cured from a HER2 directed approach alone, without the need for traditional cytotoxic agents. The outcome of patients who had obtained a pCR was excellent; pCR was associated with a lower risk of an IDFS event [stratified HR, 0.24 (95% CI, 0.09 to 0.60)]among all those who underwent surgery (n=418) (7).
Limitations
Although the KRISTINE study adds important information about how pCR translates into long-term benefit, questions remain surrounding the validity of pCR as a primary study endpoint in HER2-positive breast cancer. Several agents have improved pCR in the preoperative setting, however this benefit has not always translated into improved OS. Additionally, inconsistencies in the definition of pCR have made reporting and interpretation of data challenging. The most rigorous definition of pCR (as used in KRISTINE) is ‘no residual invasive carcinoma in the breast or axillary lymph nodes’, however in order to more critically evaluate results, a standardized definition should be used in all clinical trials (9). In KRISTINE, pCR was locally (rather than centrally) determined, which introduces the possibility of bias. Another limitation was that this was a relatively small study, which was not adequately powered to detect differences in the secondary endpoints of EFS, IDFS, and OS (7).
Discussion
This phase III study demonstrated that for patients with stage II-III HER2-positive breast cancer, a HER2-targeted neoadjuvant regimen of T-DM1+P led to a greater risk of an EFS event but a comparable risk of an IDFS event when compared to the conventional systemic chemotherapy regimen of TCH-P. In fact, 15 (6.7%) patients in the T-DM1+P arm experienced loco-regional progression before surgery. Tumor analysis from this cohort revealed lower HER2 expression and higher HER2 heterogeneity when compared to other patients who received T-DM1+P. This suggests that in this group of patients who have low or heterogeneous HER2 expression, conventional systemic chemotherapy may still be required (7).
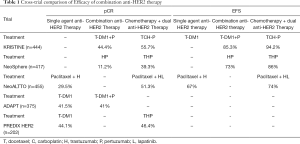
Several studies have evaluated a variety of HER2 targeted approaches in the neoadjuvant setting. The Phase II NeoSphere trial (n=417) was a four-armed study that compared neoadjuvant T plus H, P or both. Patients with tumors ≥2 cm were enrolled. The primary endpoint was pCR in the breast with remaining in-situ lesions allowed. The percentage of patients who achieved pCR and were axillary lymph node negative at surgery was higher with THP versus those treated with TH (39.3% vs. 21.5%). In the Swedish PREDIX trial, which included women with HER2-positive breast cancer >2 cm; pCR rates after six cycles of neoadjuvant single-agent T-DM1 compared favorably to those treated with six cycles of THP (44% versus 46%) (10), thus, establishing the basis for the control arm on the KRISTINE study (6). Similar results were seen in the ADAPT study, in which only 4 cycles of neoadjuvant T-DM1 was associated with a pCR rate of 41% although a difference was that this trial focused on patients with tumors which were both HER2 and hormone receptor positive disease (11). In total, 375 patients were randomized to either 12 weeks of T-DM1 with or without endocrine therapy (ET) or to H with ET. The primary endpoint was pCR (ypT0/is/ypN0). Broadly, there is consistency between these trials that T-DM1+P results in similar rates of pCR to THP, which is predictable given that the cytotoxic component of T-DM1, like T, inhibits microtubules and given the known activity of T-DM1 in the metastatic setting (Table 1).
Full table
Patients who achieve a pCR from preoperative therapy have a better prognosis than those who do not (12). In the five-year analysis of NeoSphere, those who obtained a pCR (all groups combined) had an improved EFS versus those who did not have a pCR (85% vs. 76%, respectively; HR =0.54; 95% CI, 0.29–1.00) (13). A similar result was seen in the NeoAltto trial, in which the oral tyrosine kinase inhibitor lapatinib (L) plus H and weekly paclitaxel significantly increased pCR rates compared with paclitaxel plus either single anti-HER2 agent alone (46.8% L+H+ Paclitaxel vs 27.6% L+H vs 20% L+Paclitaxel) (14). Again, the 6-year EFS and OS were significantly higher in patients with a pCR compared with those without a pCR, (77% and 65%) and (89% and 77%) respectively (15). Hence, pCR, is well established as a prognostic biomarker. However, a key consideration is whether or not incremental improvements in pCR with more intensive therapies translate into corresponding improvements in OS. Given the high rates of cure in early stage HER2 positive breast cancer in general, there is a high bar for which new therapies have to overcome. Although L improved pCR in the NeoAltto trial, the much larger Altto trial (n=8,381), failed to show an OS benefit for the addition of a longer course of L to H-based postoperative combination chemotherapy. Although it has been argued that these disappointing results might have been explained by a lack of efficacy and tolerability of L, similar results have been seen with P. Specifically, although the addition of P to preoperative therapy improved pCR in the NeoSphere trial, this did not equate to improved long term OS (13). The 5-year EFS rates in Neosphere were 86%, 81%, 73% and 73% for THP, TH, TP and HP respectively (13). Furthermore the APHINITY trial (n=4805) failed to show an improvement in OS when P was added to chemotherapy in the adjuvant setting (16).
Of note, the above studies demonstrate that there are a subset of patients who obtain pCR without having received classic chemotherapy. If these subsets can be reliably identified in future studies, this may facilitate the de-escalation of systemic anti-cancer treatment and reduce treatment associated side-effects. Like in the KRISTINE study, there was a proportion of patients (11.2%) who achieved pCR without conventional cytotoxic chemotherapy in the NeoSphere trial (17). In the phase II ADAPT trial, patients treated with T-DM1 alone had a pCR rate of 41.0% (11).
The development of predictive biomarkers to accurately select patients who may benefit from more intensive anti-HER2 therapy or those who may be able to forego chemotherapy will be a key area of interest going forward. In the NeoSphere study, high HER2 levels were significantly associated with improved pCR rates (P=0.001) and sensitivity to P. In addition, a PIK3CA exon 9 mutation was associated with residual disease and a poor response to anti-HER2 therapy (17). An analysis of the NeoAltto trial showed that patients who experienced a rash within the first 6 weeks of treatment with L, had a better chance of obtaining a pCR (18). Similarly, the development of early rash in the phase III adjuvant Altto trial was associated with improved OS as compared with patients who did not develop an early rash (multivariable: HR =0.63, 95% CI, 0.48 to 0.82, P<0.001) (19). This is not surprising since L also targets HER1 (also called EGFR) and rash has been correlated with clinical benefit from EGFR tyrosine kinase inhibitors in lung cancer. Although the development of rash would be clinically reproducible outside of research studies, it may not be of major utility given the extensive toxicities that typically accompany the L-related rash (fatigue, diarrhea etc.) and the obvious question as to whether treatment should be changed in patients without an early rash.
An alternative approach, which has been further informed by KRISTINE is the use of response in the preoperative setting to select adjuvant therapy. Specifically, the KRISTINE study suggests that patients who do not respond clinically to T-DM1+P can potentially be salvaged by surgery, have escalation of their treatment (to include more cytotoxic chemotherapy) postoperatively without an apparent negative impact on outcome (similar EFS). Alternatively, in the KATHERINE trial patients who did not achieve a pCR with preoperative chemotherapy with H were randomized to H or T-DM1. This study showed a reduced risk of recurrent invasive breast cancer or death with T-DM1 versus H (HR 0.50; 95% CI, 0.39 to 0.64; P<0.001) (20). This approach might be attractive in terms of the financial impact of anti-HER2 therapy, since novel more expensive agents (such as T-DM1) are preferentially given to patients with the highest risk of recurrence, rather than the opposite approach adopted in KRISTINE. Conversely, this means that potentially more patients are exposed to cytotoxic chemotherapy and the resultant toxicities. Such a risk adaptive strategy also requires the broad use of neoadjuvant as opposed to adjuvant systemic therapy.
The considerable toxicities with chemotherapy and antiHER2 therapy must be carefully balanced against the generally more favorable outcomes in women with the smallest lowest risk cancers. Tolaney et al. examined the competing approach of adjuvant paclitaxel and H in a trial involving 406 women with node negative HER2-positive breast cancer. Patients were treated with paclitaxel + H on a weekly schedule for 12 weeks, and subsequently received H monotherapy for 9 months. IDFS was the primary endpoint. The results suggested that adjuvant paclitaxel + H was associated with a low risk of early recurrence, (less than 2% at 3 years). There was a low rate of serious adverse events, (incidence of heart failure only 0.5%) (21). The recent Phase 2 ATEMPT trial expanded on this concept and sought to determine whether T-DM1 has a clinically acceptable event rate in those with stage I HER2-positive breast cancer and whether T-DM1 is associated with less clinically relevant toxicity (CRT) as compared with Paclitaxel + H. Patients were randomized to either adjuvant T-DM1 or to paclitaxel + H. The coprimary endpoints were 3-year DFS in the T-DM1 arm and compared incidence of clinically relevant toxicities (CRTs) between T-DM1 and paclitaxel + H. T-DM1 proved to be highly effective with a 3-year DFS of 97.7% (95% CI, 96.2–99.3%). The trial did not compare 3-year DFS between the two groups, however 3-year DFS was 92.8% (95% CI, 87.8–98.1%) among those assigned to paclitaxel + H. No difference in CRTs was noted (46% in both arms) but there was a different toxicity profile. The trial suggests that paclitaxel + H remains a very reasonable standard of care in this patient population, however T-DM1 can be considered in select patients, albeit with increased financial toxicities particularly if paclitaxel + H related toxicities such as neurotoxicity are a concern (22). The ongoing KAITLIN trial compares adjuvant T-DM1+P to H, P and a taxane following anthracycline therapy in HER2-positive early breast cancer. These results will be important in the future management of HER2-positive early breast cancer and may further clarify strategies in HER2 targeted adjuvant treatment for this patient cohort.
Conclusions
In HER2 positive early stage breast cancer the litany of active therapies means that increasingly treatment is becoming individualized. Overall, there is a growing need to identify the most appropriate therapy in this group of patients who have a biologically aggressive disease. The KRISTINE study showed that relative to TCH-P, T-DM1+P resulted in a greater risk of an EFS event due to locoregional progression events prior to surgery. The risk of an IDFS event was similar between groups. The T-DM1+P arm also experienced fewer grade III or greater AEs during the neoadjuvant phase of treatment, as well as more AEs in the adjuvant setting, resulting in early discontinuation of treatment (7). De-escalation of therapy is appealing as it allows the option to avoid conventional systemic chemotherapy, reduce toxicity and potentially shorten the duration of adjuvant treatment, but there are important cost implications. The level of HER2 expression and HER2 heterogeneity appeared to play a role in predicting response in KRISTINE and biomarkers are needed to better identify patients who may benefit from a targeted therapy approach (7). In addition, the emergence of immunotherapy may provide further new treatment options and ongoing progress in this area is needed.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Arteaga CL, Sliwkowski MX, Osborne CK, et al. Treatment of HER2-positive breast cancer: current status and future perspectives. Nat Rev Clin Oncol 2011;9:16-32. [Crossref] [PubMed]
- Morris PG, Hudis CA. Trastuzumab-Related Cardiotoxicity Following Anthracycline-Based Adjuvant Chemotherapy: How Worried Should We Be? J Clin Oncol 2010;28:3407-10. [Crossref] [PubMed]
- Cortazar P, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 2014;384:164-72. [Crossref] [PubMed]
- Murphy CG, Morris PG. Recent advances in novel targeted therapies for HER2-positive breast cancer. Anticancer Drugs 2012;23:765-76. [Crossref] [PubMed]
- Pernas S, Tolaney SM. HER2-positive breast cancer: new therapeutic frontiers and overcoming resistance. Ther Adv Med Oncol 2019;11:1758835919833519. [Crossref] [PubMed]
- Hurvitz SA, Martin M, Symmans WF, et al. Neoadjuvant trastuzumab, pertuzumab, and chemotherapy versus trastuzumab emtansine plus pertuzumab in patients with HER2-positive breast cancer (KRISTINE): a randomised, open-label, multicentre, phase 3 trial. Lancet Oncol 2018;19:115-26. [Crossref] [PubMed]
- Hurvitz SA, Martin M, Jung KH, et al. Neoadjuvant Trastuzumab Emtansine and Pertuzumab in Human Epidermal Growth Factor Receptor 2–Positive Breast Cancer: Three-Year Outcomes From the Phase III KRISTINE Study. J Clin Oncol 2019;37:2206-16. [Crossref] [PubMed]
- Hudis CA, Barlow WE, Costantino JP, et al. Proposal for Standardized Definitions for Efficacy End Points in Adjuvant Breast Cancer Trials: The STEEP System. J Clin Oncol 2007;25:2127-32. [Crossref] [PubMed]
- Pennisi A, Kieber-Emmons T, Makhoul I, et al. Relevance of Pathological Complete Response after Neoadjuvant Therapy for Breast Cancer. Breast Cancer (Auckl) 2016;10:103-6. [Crossref] [PubMed]
- Bergh JCS, Andersson A, Bjohle J, et al. Docetaxel, trastuzumab, pertuzumab versus trastuzumab emtansine as neoadjuvant treatment of HER2-positive breast cancer: Results from the Swedish PREDIX HER2 trial identifying a new potential de-escalation standard? J Clin Oncol 2019;37:501. [Crossref]
- Harbeck N, Gluz O, Christgen M, et al. De-Escalation Strategies in Human Epidermal Growth Factor Receptor 2 (HER2)-Positive Early Breast Cancer (BC): Final Analysis of the West German Study Group Adjuvant Dynamic Marker-Adjusted Personalized Therapy Trial Optimizing Risk Assessment and Therapy Response Prediction in Early BC HER2- and Hormone Receptor-Positive Phase II Randomized Trial-Efficacy, Safety, and Predictive Markers for 12 Weeks of Neoadjuvant Trastuzumab Emtansine With or Without Endocrine Therapy (ET) Versus Trastuzumab Plus ET. J Clin Oncol 2017;35:3046-54. [Crossref] [PubMed]
- von Minckwitz G, Untch M, Blohmer JU, et al. Definition and Impact of Pathologic Complete Response on Prognosis After Neoadjuvant Chemotherapy in Various Intrinsic Breast Cancer Subtypes. J Clin Oncol 2012;30:1796-804. [Crossref] [PubMed]
- Gianni L, Pienkowski T, Im YH, et al. 5-year analysis of neoadjuvant pertuzumab and trastuzumab in patients with locally advanced, inflammatory, or early-stage HER2-positive breast cancer (NeoSphere): a multicentre, open-label, phase 2 randomised trial. Lancet Oncol 2016;17:791-800. [Crossref] [PubMed]
- de Azambuja E, Holmes AP, Piccart-Gebhart M, et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): survival outcomes of a randomised, open-label, multicentre, phase 3 trial and their association with pathological complete response. Lancet Oncol 2014;15:1137-46. [Crossref] [PubMed]
- Huober J, Holmes E, Baselga J, et al. Survival outcomes of the NeoALTTO study (BIG 1-06): updated results of a randomised multicenter phase III neoadjuvant clinical trial in patients with HER2-positive primary breast cancer. Eur J Cancer 2019;118:169-77. [Crossref] [PubMed]
- von Minckwitz G, Procter M, de Azambuja E, et al. Adjuvant Pertuzumab and Trastuzumab in Early HER2-Positive Breast Cancer. N Engl J Med 2017;377:122-31. [Crossref] [PubMed]
- Gianni L, Pienkowski T, Im YH, et al. Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol 2012;13:25-32. [Crossref] [PubMed]
- Azim HA Jr, Agbor-Tarh D, Bradbury I, et al. Pattern of rash, diarrhea, and hepatic toxicities secondary to lapatinib and their association with age and response to neoadjuvant therapy: analysis from the NeoALTTO trial. J Clin Oncol 2013;31:4504-11. [Crossref] [PubMed]
- Sonnenblick A, de Azambuja E, Agbor-Tarh D, et al. Lapatinib-Related Rash and Breast Cancer Outcome in the ALTTO Phase III Randomized Trial. J Natl Cancer Inst 2016. [Crossref] [PubMed]
- von Minckwitz G, Huang CS, Mano MS, et al. Trastuzumab Emtansine for Residual Invasive HER2-Positive Breast Cancer. N Engl J Med 2019;380:617-28. [Crossref] [PubMed]
- Tolaney SM, Barry WT, Dang CT, et al. Adjuvant Paclitaxel and Trastuzumab for Node-Negative, HER2-Positive Breast Cancer. N Engl J Med 2015;372:134-41. [Crossref] [PubMed]
- Tolaney SM, Hu J, Dang C, et al. TBCRC 033: A randomized phase II study of adjuvant trastuzumab emtansine (T-DM1) vs paclitaxel (T) in combination with trastuzumab (H) for stage I HER2-positive breast cancer (BC) (ATEMPT). Presented at: 2019 San Antonio Breast Cancer Symposium; December 10-14; San Antonio, TX. Abstract GS1-05.


