
Recanalizing left anterior descending artery chronic total occlusion with reverse controlled antegrade and retrograde tracking technology through epicardial collateral
Introduction
Chronic total occlusion (CTO) refers to the complete occlusion of coronary artery for more than 3 months (1), and it is a stubborn obstacle to overcome during coronary intervention. In recent years, with the continuous advancement of surgical instruments and experience of surgeons, especially in the application of antegrade and retrograde guiding wire technology, the success rate of CTO-percutaneous coronary intervention (PCI) has been significantly improved (2,3). Although the antegrade guiding wire technology is the most important means of CTO-PCI treatment, retrograde guiding wire technology is also competent in treating CTO.
Retrograde approach providing new perspectives through the use of collateral channels has improved primary success rate of CTO-PCI, while only few cases of successful direct retrograde wire crossing have been reported, and reverse controlled antegrade and retrograde tracking (CART) is the most frequently used technique for retrograde wire crossing (4). The reverse CART technique is relatively simple and can significantly shorten the operation time and it is a milestone strategy for CTO-PCI (5).
Case presentation
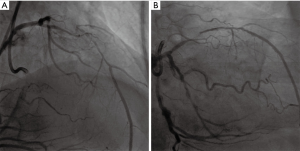
The patient was a 67-year-old man with 15 years of old myocardial infarction (OMI). He had a 3-year history of high blood pressure (BP) and glucose without systemic treatment. He was also a smoker of 30 years. On this occasion, he was hospitalized for one month of repeated chest pain. Admission examination revealed a BP of 127/72 mmHg, and a pulse rate of 90 beats/min, and no abnormalities in cardiopulmonary function. In blood examination, there was a slight increase in fasting blood glucose, which was 7.14 mmol/L, there were no abnormalities in myocardial enzymes, brain natriuretic peptide, blood routine, liver and kidney function. Admission electrocardiogram showed an old anterior wall myocardial infarction, and a heart rate of 90 beats/min. Cardiac ultrasound showed no obvious abnormalities, with an ejection fraction of 65%. Admission diagnosis revealed coronary atherosclerotic heart disease, unstable angina, OMI, high BP level 2 and type 2 diabetes. Thoracic angiography showed left main (LM) plaque, 100% occlusion in the proximal left anterior descending artery (LAD), 100% occlusion in the medial branch, 50% stenosis in the proximal left circumflex artery (LCX), and 90% stenosis in the middle of the right coronary artery (RCA) with unstable plaque. The distal spontaneous suture was accompanied by intramural hematoma, and the distal end of the RCA provided a level 2 collateral circulation to the LAD. Considering that the patient's newly angina pectoris was related to the proximal segment of the RCA, a stent of 4.0 mm × 28 mm (12 atm, 6 s) was implanted into the proximal segment of RCA. After 3 days, we tried to recanalize the CTO lesions in the anterior descending branch. Bilateral femoral artery access was established, and 7F EBU3.5 was selected as the antegrade guidance catheter and 7F AL1.0 as the retrograde guidance catheter to complete bilateral angiography, as shown in the Figure 1A,B.
First attempt
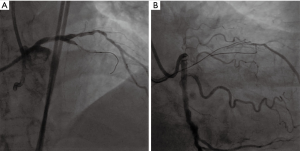
In the direction of 7F EBU3.5, we sent the Sion blue guide wire to the branch next to the LAD occlusion segment. The intravascular ultrasound (IVUS) check confirmed that the LAD true lumen was above the branch (Figure 2A). With the help of Kaneka double-cavity microcatheter, the Gaia first guide wire was sent to the LAD occlusion along the front Kaneka side hole. We failed to pass through the occlusion segment after repeated attempts, so we turned to the Gaia third guide wire, while the guide wire went beneath intima, which was itself confirmed in false lumen by contralateral angiography (Figure 2B).
Retrograde approach
Guided by 7F AL1.0, the Sion blue guide wire guided the 1.5 m Corsair microcatheter to the far end of the RCA. Tip injection found that collateral circulations were 0 to 1, in which condition the Sion, Sion blue and SOUHO3 guide wire surfing all failed to pass through (Figure 3A).
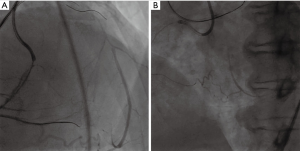
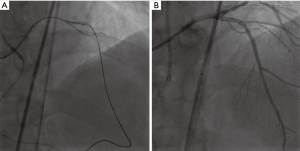
Epicardial pathway
The Sion blue guide wire was used to guide the 1.5 m Corsair microcatheter to the far end of the RCA, then the Sion guide wire was used, the wire passed smoothly through the lateral branch into the LAD distal segment, then into the middle of the LAD (Figure 3B). Then we pushed the microcatheter forward and turned to Gaia 2 guide wire, and failed when we tried to enter into the true cavity. Guided by the contralateral guide wire, we used antegrade Gaia 1 guide wire to pass through the occlusion slowly, overlap with the retrograde guide wire, and used the reverse CART to expand the LAD occlusion with a 2.0 mm × 15 mm balloon (10 atm, 6 s) (Figure 4A). We further used a Gaia 2 guide wire to puncture proximal occlusion segment of the LAD and enter into the forward EBU guide catheter. Next, we pushed the Caravel microcatheter forward into the EBU catheter, changed to the RG3 guide wire, externalized guide wire through the AL1.0-RCA-AM-micro-guide-LAD-EBU3.5, and expanded the lesion with a 2.0 mm × 15 mm balloon (12 atm, 6 s) and 2.5 mm × 15 mm balloon (10 atm, 6 s). After IVUS check, 2.5 mm × 30 mm (12 atm, 6 s) and 2.5 mm × 18 mm (14 atm, 6 s) stents were placed in the middle of the LAD (Figure 4B). At last, the retrograde guidewire and microcatheter were withdrawn, and the RCA angiography showed no collateral circulation damage and rupture.
Discussion
For this case, the CTO segment was very short (occlusion part about 10–15 mm) with side branch at the blunt end and no angulation, the J-CTO score was 1 point, antegrade approach should be quite effective. According to the APCTO algorithm (6), we firstly chose IVUS-guided entry and parallel wire technique, but we failed to enter into the true lumen. Then we turned to retrograde approach, in which septal channel was primarily tried, and with the help of surfing technique, we couldn’t pass through the septal channel partly due to its ambiguous continuity. Then we chose the epicardial collateral and reverse CART technique and successfully recanalized the LAD CTO.
At present, the commonly used retrograde guiding wire technology includes (I) retrograde guiding wire-to-kiss technology; (II) retrograde guiding wire passing technology; (III) controlled antegrade and retrograde subintimal tracking; (IV) and reverse CART technique (7,8). The CART technique is relatively mature, while it has a number of limitations. For example, it is difficult to cross or dilate small and tortuous septal channels and there exists the risk of septal injury when making septal dilatations. It is also easy to cause channel rupture, balloon trapping and subintimal dissection. In contrast to CART technology, the reverse CART technology does not require reverse delivery of the balloon catheter, which avoids damage to the collateral vessel and lowers the risk of perforation. In the reverse CART technique, the balloon is advanced into the CTO segment along the antegrade guide wire and expanded to form a confined false lumen. The retrograde guiding wire is advanced into the lumen, and then further into the proximal true lumen. Because it is relatively simpler, quicker and safer, the reverse CART technique has become the most popular retrograde guide wire technology in CTO (2,9,10). Once the retrograde guide wire cannot pass the occlusion lesion and overlaps the antegrade guide wire by 20 to 30 mm, the reverse CART technique is considered. To ensure the success of the reverse CART technique, it is recommended that the surgeon guides the retrograde wire to the antegrade wire in the direction of the long axis of the blood vessel as much as possible. For anterior descending lesions, a 2.0–2.5 mm balloon is usually chosen for reverse CART technique, and for right coronary artery occlusion lesion, a 2.5–3.0 mm balloon is recommended. When the reverse CART technique is performed, the sandwich caused by the expansion of the antegrade balloon may have a two-way extension. To reduce the damage to the target vessel, the contrast agent should be prohibited from being pushed through the antegrade guiding catheter after the balloon is expanded in the antegrade balloon. If the antegrade guiding wire is still unable to enter into the proximal lumen when the balloon is dilated, the surgeon can perform reverse CART technique under the guidance of IVUS.
Conclusions
The reverse CART technique is relatively simple and can significantly shorten the operation time. The combined use of forward and retrograde technologies will significantly improve the surgical success rate of complex CTO-PCI.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Ge JB. Current status of percutaneous coronary intervention of chronic total occlusion. J Zhejiang Univ Sci B 2012;13:589-602. [Crossref] [PubMed]
- Tajti P, Burke MN, Karmpaliotis D, et al. Update in the Percutaneous Management of Coronary Chronic Total Occlusions. JACC Cardiovasc Interv 2018;11:615-25. [Crossref] [PubMed]
- Lee SW, Lee PH, Ahn JM, et al. Randomized Trial Evaluating Percutaneous Coronary Intervention for the Treatment of Chronic Total Occlusion. Circulation 2019;139:1674-83. [Crossref] [PubMed]
- Matsuno S, Tsuchikane E, Harding SA, et al. Overview and proposed terminology for the reverse controlled antegrade and retrograde tracking (reverse CART) techniques. EuroIntervention 2018;14:94-101. [Crossref] [PubMed]
- Kimura M, Katoh O, Tsuchikane E, et al. The efficacy of a bilateral approach for treating lesions with chronic total occlusions the CART (controlled antegrade and retrograde subintimal tracking) registry. JACC Cardiovasc Interv 2009;2:1135-41. [Crossref] [PubMed]
- Harding SA, Wu EB, Lo S, et al. A New Algorithm for Crossing Chronic Total Occlusions From the Asia Pacific Chronic Total Occlusion Club. JACC Cardiovasc Interv 2017;10:2135-43. [Crossref] [PubMed]
- Rathore S, Katoh O, Tuschikane E, et al. A novel modification of the retrograde approach for the recanalization of chronic total occlusion of the coronary arteries intravascular ultrasound-guided reverse controlled antegrade and retrograde tracking. JACC Cardiovasc Interv 2010;3:155-64. [Crossref] [PubMed]
- Surmely JF, Tsuchikane E, Katoh O, et al. New concept for CTO recanalization using controlled antegrade and retrograde subintimal tracking: the CART technique. J Invasive Cardiol 2006;18:334-8. [PubMed]
- Tajti P, Brilakis ES. Chronic Total Occlusion Percutaneous Coronary Intervention: Evidence and Controversies. J Am Heart Assoc 2018. [Crossref] [PubMed]
- Suzuki Y, Tsuchikane E, Katoh O, et al. Outcomes of Percutaneous Coronary Interventions for Chronic Total Occlusion Performed by Highly Experienced Japanese Specialists: The First Report From the Japanese CTO-PCI Expert Registry. JACC Cardiovasc Interv 2017;10:2144-54. [Crossref] [PubMed]
Cite this article as: Wang C, Sun Z. Recanalizing left anterior descending artery chronic total occlusion with reverse controlled antegrade and retrograde tracking technology through epicardial collateral. AME Case Rep 2019;3:15.


