The utility of virtual consultations in breast outpatient clinics: a proposed model in response to COVID-19 pandemic
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has disrupted non-emergency clinical work in ways that were never witnessed in modern medicine before. Breast Clinical Services were particularly vulnerable to this disruption as the nature of the service involves high traffic through Outpatient Clinics, Radiology Departments, Screening Centres and Day-case Services. The Association of Breast Surgery (ABS) response to the COVID pandemic was swift, clear and timely. The first ABS announcement was published on 15th March 2020 and contained directives of how the Breast Services had to function during this crisis.
Across the United Kingdom (UK), all breast units responded promptly, dramatic changes to regular practice were adopted from triaging new referrals, audio and video consultations to temporary alterations of surgical, neo-adjuvant and adjuvant pathways. Despite the disruption, this unprecedented state of shock has offered us, as professionals and service providers, a unique opportunity to reflect on our normal practice. We now have to consider futuristic models of care that are less disruptive, yet equally safe and effective.
Since the start of the pandemic, breast referrals have dropped by approximately 60–70% (1), consequently a surge in referrals is anticipated at the awakening from this peak of the pandemic. Professionals and public alike now appreciate that the new normal way of life will involve social distancing in almost every human activity and perhaps for longer periods of time than initially anticipated. Therefore, it is essential to think of adaptive models where breast services can be safely delivered observing social distancing and minimising the risk of viral transmission. This article proposes a model to run breast outpatient clinics with as little as necessary face-to-face consultations yet respecting patients’ physical and emotional needs and providing a high standard of care.
Methods
Similar to many breast units across the UK, our unit utilises referral triaging and virtual consultations in line with the ABS guidelines and the Greater Manchester Combined Authority consultations. Review of the new practices was performed. Extensive discussions amongst all consultant surgeons in the Breast Department at the Pennine Acute Hospitals NHS Trust, together with representative consultants from other Trusts in Greater Manchester area has been conducted. A balanced, evidence-based, expert opinion was reached, distributed and agreed amongst all participants. Recommendations about how to run breast outpatient clinics, including new referrals and follow ups, during the COVID-19 pandemic and the recovery phase were issued.
Results
The consultations resulted in the following recommendations
Encouraging breast referrals
It is vital to encourage patients with breast concerns to seek professional advice without delays. Assessments procedures will be tailored to the individual’s own circumstances and their risk category. In countries like the UK where access to specialist services is through general practitioners (GPs), it is important to explain to GPs that all referrals are encouraged. They will be triaged and managed utilising pragmatic protocols, but they will all have safe and professional assessments. Charities and social media platforms in the UK and worldwide are being used to encourage patients with breast symptoms to seek referral during COVID pandemic. A dedicated specialist hotline or speciality generic e-mail that is manned during working hours could be proposed to aid GPs manage their referrals and patients’ expectations effectively. A post COVID wave of late breast cancer presentations is a genuine concern to breast specialists, particularly with the temporary suspension of breast screening.
Triaging referrals
In pre-COVID era, all UK GP referrals were seen directly by specialist services, within targeted waiting times, regardless of their age, presentation or index of suspicion. Overnight, this became unfeasible and obviously unsafe. Therefore, all UK breast units have adopted triage policies to all new referrals since the start of the pandemic. Apart from minute differences between regions, these policies were largely identical. The focus was to identify red flag symptoms (new lump; peau d’orange; ulceration, axillary lump), high-risk individuals (those with personal or a strong family history), and to prioritise the clinical assessment urgency and its form accordingly. Some very low risk referrals like breast pain were managed by writing directly to patients without a direct consultation.
In the current state of COVID pandemic, referrals can be simply triaged into two categories: low-risk category, these referrals can be initially assessed by phone or video consultations, then either discharged, followed up, referred directly to investigations (mammogram, ultrasound with or without a biopsy) or escalated to the high-risk category where a face-to-face consultation and triple assessment is essential. This is explored in more details by the presenting symptoms below.
New referrals pathways
The consultations proposed a pathway dependent on the presentation and the index of suspicion.
Lumps or distortion
More than 80% of breast cancers present as defined lump or change in shape of breast (2), especially in the younger age group (3). Therefore, all patients referred with a new lump or persistent distortion should be in the high-risk category and offered a face-to-face triple assessment as per pre-COVID protocols.
Few exceptions may be considered, if necessary. As breast cancer in women under the age of 30 makes 0.6% of all breast cancers (4,5), referrals from this age group, with no significant family history may be offered a virtual (telephone or video) consultation followed by direct radiological assessment, if deemed low risk. Similarly, patients with history of confirmed recurring cysts who had breast imaging in the last 6 months, or patients with increase in the size of previously diagnosed benign lump by biopsy may follow a similar pathway.
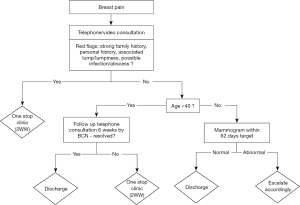
Pain
Breast pain is the most common presenting symptom to outpatient clinic (6). Approximately 4% of patient presenting with breast pain will have a diagnosis of in situ or invasive cancer (2). The relationship between breast pain and early malignancy remains poorly understood, and to a great extent, is believed to be coincidental. All breast pain referrals can initially be assessed by virtual consultations, if no red flags are identified then they should be offered a planned mammogram within 62 days if they were over 40 years old. For those under 40, advice can be given during the telephone consultation and may be emphasised by post. Patients may subsequently be discharged or offered a follow up to confirm symptoms have resolved. It is well established that reassurance plays a major role in managing breast pain (7), therefore support from breast care nurses (BCN) may be required. Obviously, referrals with red flags should be seen in one stop clinic for triple assessment as per pre-COVID protocols. The flowchart in Figure 1 summarises this model for breast pain.
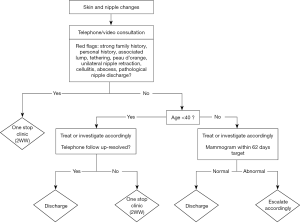
Changes to skin/nipple-areola complex
Breast referrals with isolated skin changes to the breast or nipple-areola complex are less common and may represent a benign or malignant pathology (8). Referrals with skin changes to the breast envelope associated with red flag signs (peau d’orange or tethering) are high-risk and should be offered a face-to-face triple assessment as per pre-COVID protocols.
Paget’s disease of the nipple is rare with an incidence of 1–4% of all breast cancers (9), early identification is essential to avoid delays in management. Nipple changes can be assessed initially by phone or video consultation; if no red flags were identified, they can be referred for targeted imaging and have a trial of medical treatment if deemed consistent with eczema. Further follow up by virtual consultation to ensure symptoms have resolved is recommended. If red flags were identified they should be offered a face-to-face triple assessment as per pre-COVID protocols.
Acute unliteral nipple retraction is rare and should be considered as high risk, these patients are best served in one-stop face-to-face consultation for triple assessment. Patients with bilateral or long-standing nipple retraction are less likely to have a significant pathology and can be offered a virtual consultation with a planned mammogram and retroareolar USS within 62 days if they were older than 40 years.
Breast abscess
Breast abscess is an acute pathology and should continue to be reviewed urgently in one stop breast clinic as per pre-COVID protocols.
Nipple discharge (ND)
Over 80% of females will have at least one episode of ND in their lifetimes (10). Clinical features of pathological ND include blood-stained; spontaneous; uniductal; and unilateral. The incidence of underlying malignancy in pathological ND is variable and may range between 3% and 30% (11). Additionally, up to 20% of malignant or high-risk lesions presenting as ND are identified solely after surgery having had no concerning radiological features (10). In general, patients under 50 years of age with no risk factors may be considered low-risk and candidates for follow up management. Our model proposes that all ND referrals to have a virtual consultation. If pathological ND is suspected, then a face-to-face triple assessment is recommended. Non-pathological ND can either be discharged after a virtual consultation or be referred for relevant breast imaging within 62 days, especially if they are over 40 years of age. The flowchart in Figure 2 summarises the proposed model for skin and nipple changes.
Cosmetic/symmetry/implant complications
Patients referred with urgent implant-related complications such as infection, rupture, leak, enlarged axillary lymph nodes, acute seroma or acute change in shape will require urgent face-to face assessment, especially if anaplastic large cell lymphoma (ALCL) is suspected. Other congenital or long standing cosmetic and asymmetrical presentations can be initially addressed using virtual consultations until operating theatre and clinic capacities will allow for elective cosmetic work.
Gender affirmation surgeries are only offered in specialised hubs in the UK and most referrals live quite far from their treating centres. Therefore, it may be advisable to assess new referrals in virtual clinics until this service is resumed. Selecting priorities for gender affirmation surgery after COVID may be heavily influenced by psychological considerations.
Family history and genetics
Consultations that don’t normally involve clinical examination are best served in a virtual approach. This does not only minimise traffic through clinical areas, it is also more time-efficient and easier for patients as they don’t have to worry about travelling to clinic or car parking. Eventually, having a face-to-face consultation when both patient and consultant are wearing a mask may pose more communication barriers than a well-structured video consultation. Qualitative research to understand the nature and implications of communication barriers in the clinical settings of COVID era would definitely help to assess patients’ satisfaction and influence referral pathways.
Male breast lumps
Over 90% of male breast cancers present after the age of 50 (12,13). Therefore, unilateral, isolated breast lumps in men over 50 years of age should be assessed in face-to-face one stop clinics directly. Bilateral gynaecomastia with no isolated lumps can be evaluated in virtual clinics and referred for bilateral mammograms if deemed necessary according to individual unit’s policy.
Follow-up pathways
Post op
It is essential to empower patients with their post-operative care. Patients should be encouraged to contact their BCN if they have any acute concerns about their wounds or general wellbeing following their operation. Following simple breast surgery (without reconstruction) wound check and discussion of pathology results can be conducted in virtual manner to limit patients visits to the hospital. Patients should be asked in advance if they prefer to attend a telephone, video or face to face consultations post-operatively. Pre-operative treatment options and treatment summary consultations after conclusion of surgery can be safely done in virtual clinics. Further follow up and care should be provided in line with the guidance on personalised stratified follow up.
Breast reconstructions
Following complex breast reconstruction surgery, it is essential to conduct an initial face-to-face follow up, especially if adjuvant treatment is expected. The aim will be to act quickly on any signs of complications and to avoid delays in adjuvant treatment. Patients can be seen by both their operating surgeon and specialist nurse during this consultation. Subsequent consultations can be conducted in a virtual manner to ensure patient’s satisfaction with their reconstruction.
Logistical considerations
The consultants’ discussions raised some logistical recommendations for the outpatient setting and consultation etiquettes virtual consultations which are detailed below.
Outpatient clinics
It is recommended that virtually every physical space where patients or relatives may visit, walk through, wait in, or receive medical care at is formally risk assessed and re-designed in ways that minimise viral transmission and facilitate social distancing. The “new normal” should be observed whether a person is visiting a medical institute or taking a bus ride. This will naturally reduce the capacity of any medical unit at a given period of time and therefore careful logistical planning is required to safely maximise capacity.
A one-way traffic system is recommended with a separate entry and exit points. Whenever possible, this should apply to outpatient clinics and radiology departments to minimise the risk of crowding. Waiting areas must be redesigned allowing social distancing and all members off staff should wear personal protective equipment (PPE) in the clinical environment. PPE should be changed after physical contact with patients and strict hand-washing protocols should be implemented. In line with WHO recommendations, all patients and visitors are advised to wear face masks when present in a clinical area (14). The unit should be cleaned at the end of every working day.
All effort should be made to accommodate for high risk, frail, immunocompromised and shielding patients. Whenever possible, they should be booked as first cases of the day to reduce their risk of infection. If this is not feasible, then consider booking their consultations at times when there is reduced footfall through the clinic, such as during the multi-disciplinary team meetings. Waiting times should ideally be reduced to minimum and time allocations for individual appointments are advised to account for all care elements including anticipated radiology requirements, mobility issues, disabilities, language barriers and the need for interpreters. Some units may benefit from a call-in model where patients are encouraged to wait in their cars, upon arrival to hospital for their appointment, until they are called in.
Virtual consultations
Virtual consultations have been expedited in response to COVID pandemic in many specialities including urology, dermatology, physiotherapy, paediatrics and General Practice. The patient and professional feedbacks have been hugely encouraging (15,16). Telephone consultations should be conducted in a controlled professional manner, a quiet environment with minimal interruptions is essential. Documentation of consultation is recommended to take place during the same session with a consultation summary letter sent to both patient and GP, at the end of each virtual clinic. Similar applies to video consultations. Additionally, these are recommended to take place in a neutral environment with enough lighting and minimal glare. Make sure there is no distracting items in the background such as personal or family photographs, similarly no items that may reflect your religious or political beliefs. Use a fixed chair to avoid unnecessary body movements, introduce yourself and any members of staff with you, check patient’s identity, make sure they can hear you and see you well and obtain their consent to proceed with the virtual consultation. Explain confidentiality particularly that all available video consolation software does not record the consultations but if the patient wishes to record it on their smart device then a mutual consent is required. It is recommended that video consultations are attended by a chaperone, especially the first consultation, whenever examination by inspection is expected (examples: skin rash, post op wound concerns) and if you are breaking unexpected news. Additional training in virtual consultation etiquette may benefit clinicians undertaking this activity.
Although virtual consultations are reliant on internet connectivity and IT literacy, it has the potential to save patients’ time, expenses and efforts. It is expected to be particularly helpful for patients who have mobility challenges and in complex cases where case conferencing may be required. To date, virtual consultation application remains limited when interpreter services are necessary.
Quality assurance
This proposed model can be adjusted (measures tightened or loosened) according to national guidelines and the recommended social distancing measures. It is vital to audit the performance results and feedback from professionals and service users alike to keep improving the clinical model.
Conclusions
It is clear that the COVID pandemic has fast tracked, and occasionally forced, some dramatic changes to how breast services are run within a very short time frame. The co-ordination, speed and magnitude of change would have been unimaginable in otherwise normal circumstances. It is therefore pertinent to learn from this experience and to evaluate these changes in protocols hoping that it may reshape our practice to the better on the long term. Such protocols may include continuing triaging referrals and utilising the technology of virtual consultations more effectively.
Acknowledgments
We are grateful to Greater Manchester Combined Authority – Cancer for sharing their consultations in the COVID recovery document published on May 27th, 2020.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs-20-75). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mahase E. Covid-19: Urgent cancer referrals fall by 60%, showing "brutal" impact of pandemic. BMJ 2020;369:m2386. [Crossref] [PubMed]
- Dixon JM, Barber MD. Breast Surgery: A Companion to Specialist Surgical Practice.6thed. Edinburgh: Elsevier; 2018.
- Ruddy KJ, Gelber S, Tamimi RM, et al. Breast cancer presentation and diagnostic delays in young women. Cancer 2014;120:20-5. [Crossref] [PubMed]
- Anders CK, Johnson R, Litton J, et al. Breast cancer before age 40 years. Semin Oncol 2009;36:237-49. [Crossref] [PubMed]
- Fredholm H, Eaker S, Frisell J, et al. Breast cancer in young women: poor survival despite intensive treatment. PLoS One 2009;4:e7695 [Crossref] [PubMed]
- Sivarajah R, Welkie J, Mack J, et al. A Review of Breast Pain: Causes, Imaging Recommendations, and Treatment. J Breast Imaging 2020;2:101-11. [Crossref]
- Smith RL, Pruthi S, Fitzpatrick LA. Evaluation and management of breast pain. Mayo Clin Proc 2004;79:353-72. [Crossref] [PubMed]
- Nicholson BT, Harvey JA, Cohen MA. Nipple-areolar complex: normal anatomy and benign and malignant processes. Radiographics 2009;29:509-23. [Crossref] [PubMed]
- Nance FC, DeLoach DH, Welsh RA, et al. Paget's disease of the breast. Ann Surg 1970;171:864-74. [Crossref] [PubMed]
- Morrogh M, Park A, Elkin EB, et al. Lessons learned from 416 cases of nipple discharge of the breast. Am J Surg 2010;200:73-80. [Crossref] [PubMed]
- Waaijer L, Simons JM, Borel Rinkes IH, et al. Systematic review and meta-analysis of the diagnostic accuracy of ductoscopy in patients with pathological nipple discharge. Br J Surg 2016;103:632-43. [Crossref] [PubMed]
- Cutuli B, Le-Nir CC, Serin D, et al. Male breast cancer. Evolution of treatment and prognostic factors. Analysis of 489 cases. Crit Rev Oncol Hematol 2010;73:246-54. [Crossref] [PubMed]
- Anderson WF, Jatoi I, Tse J, et al. Male breast cancer: a population-based comparison with female breast cancer. J Clin Oncol 2010;28:232-9. [Crossref] [PubMed]
- Feng S, Shen C, Xia N, et al. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med 2020;8:434-6. [Crossref] [PubMed]
- Greenhalgh T, Wherton J, Shaw S, et al. Video consultations for covid-19. BMJ 2020;368:m998. [Crossref] [PubMed]
- Greenhalgh T, Koh GCH, Car J. Covid-19: a remote assessment in primary care. BMJ 2020;368:m1182. [Crossref] [PubMed]
Cite this article as: Touqan N, Fatayer H, Williams K, Bramley M, Nasir N, Absar MS. The utility of virtual consultations in breast outpatient clinics: a proposed model in response to COVID-19 pandemic. Ann Breast Surg 2021;5:4.