Techniques for abductor reattachment in proximal femoral replacement for non-oncological reconstructions: a narrative review
Introduction
Background
The rate of revision total hip arthroplasties (rTHAs) as well as periprosthetic fractures has been increasing considerably in recent years as primary THAs are increasing (1-3). Similarly, as the mean age of the population increases thus the rate of proximal femur fragility fractures and failures of such fractures increase too (4-6). All these procedures and their repeated failures can lead to high degrees of bone loss of the proximal femur preventing adequate function in terms of both stability and anchorage of the abductor apparatus (7-9). In these cases of catastrophic failures with a high degree of bone loss, the use of proximal femur megaprostheses has recently been introduced in literature with good results (9-12). Megaprostheses of the proximal femur, also called proximal femur replacements (PFR), were originally designed for reconstruction after malignant bone tumor resections (13).
Rationale and knowledge gap
The popularity of using this drastic solution also in non-oncological cases comes from the fact that PFR reduces bed rest and allows early weight bearing and an early return to daily life activities decreasing systemic complications and overall mortality (14). However, these implants are burdened by several complications among which the most common are soft-tissue failures such as deficiency of the abductor mechanism and infections mining the quality of life of such patients, frequently burdened by numerous surgical interventions (15-18). The deficiency of the abductor mechanism and the consequent lack of the abductor force can ultimately lead to instability (19) and dislocations (20) that range from 11% to 15% of cases after PFR with megaprostheses (21,22).
Therefore, any kind of reconstruction of the abductor musculature function is mandatory in order to prevent such a frequent complication. The surgical techniques of gluteus medius repair/reconstruction or abductor mechanism reattachment are widely debated in the literature, but it is quite rarely dealt with in the context of PFR with megaprostheses, particularly in non-oncologic patients.
Objective
The aim of this study was to perform a review of the current literature about the available treatment options for abductor mechanism repair/reconstruction/reattachment in the treatment of non-neoplastic conditions in patients that undergo a PFR with megaprostheses. We present this article in accordance with the Narrative Review reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-26/rc).
Methods
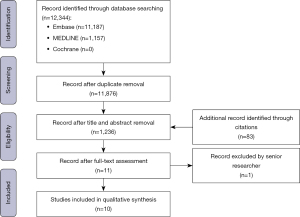
A review of the primary literature was undertaken in a systematic manner to ensure all relevant articles were considered. MEDLINE, Embase, and Cochrane databases were searched by two researchers independently from inception until February 1st, 2023 (1,157 for MEDLINE and 11,187 for Embase; Cochrane is a composite of multiple databases and thus does not report a standard inception date). Articles examining proximal femoral reconstruction with megaprosthesis or allograft prosthesis were considered. The search terms used are reported in Table 1. Articles examining proximal femoral reconstruction with megaprosthesis or allograft prosthesis, in English, French or German language were included.
Table 1
| Items | Specification |
|---|---|
| Date of search | February 1st, 2023 |
| Databases and other sources searched | MEDLINE, Embase, Cochrane |
| Search terms used | (total hip AND (reconstruction OR replacement OR megaprosthes* OR revision OR resection)) OR (hip AND (reconstruction OR replacement OR megaprosthes* OR revision OR resection)) OR (proximal femur AND (reconstruction OR replacement OR megaprosthes* OR revision OR resection)) OR (intertrochanteric AND (reconstruction OR replacement OR megaprosthes* OR revision OR resection)) OR (pertrochanteric AND (reconstruction OR replacement OR megaprosthes* OR revision OR resection)) OR (hip fracture AND (reconstruction OR replacement OR megaprosthes* OR revision OR resection)) OR (femoral infection AND (reconstruction OR replacement OR megaprosthes* OR revision OR resection)) OR (periprosthetic AND (reconstruction OR replacement OR megaprosthes* OR revision OR resection)) AND (plate OR cable OR abductor OR gluteus OR cerclage) |
| Timeframe | Inception to February 1st, 2023 |
| Inclusion and exclusion criteria | Inclusion criteria: proximal femoral reconstruction with megaprosthesis or allograft prosthesis; English, French or German language |
| Exclusion criteria: cadaver and oncologic patients; studies without full-text availability; revision THA with the use of revision stems | |
| Selection process | Two independent researchers |
THA, total hip arthroplasty.
Studies concerning cadaver and oncologic patients, and studies without full-text availability, as well as studies reporting abductor apparatus reconstruction techniques in patients undergoing revision THA with the use of revision stems instead of megaprosthesis or allograft prosthesis were excluded. Firstly, duplicate publications removal was managed with Mendeley library. After duplicate removal, references not fulfilling the inclusion and exclusion criteria were excluded by title and abstract. The full text of the included study was then analyzed and studies not satisfying the inclusion and exclusion criteria were excluded. Once the evidence was screened, the articles were selected and ultimately searched for relevant literature throughout the citations section. All the authors were contacted to obtain missing data concerning the articles they produced, but no answer was received back.
Data were extracted and stored, and qualitative synthesis was performed. The research strategy flowchart initially used to summarize the research is shown in Figure 1. The search strategy summary was also used to summarize the research as shown in Table 1.
Statistical analyses
No statistical analysis was required, but a qualitative list of the evidence is provided. This study occurs to present a narrative review since the prior aim of this publication was to perform a meta-analysis of the current literature about the available treatment option to repair the abductor mechanism after a proximal femoral reconstruction with megaprosthesis. This was not possible due to an insufficient number of studies concerning the argument, the lack of data about clinical or radiological outcomes and the poor current standardize evidence when present.
Results
The different techniques described in the current literature can be summarized in four different types: direct reattachment, trochanter sleeve osteotomy, tendon-to-muscle suture, and synthetic augmentation. The references included in the study are provided in Table 2 reporting indications, included population, and surgical techniques for each reference.
Table 2
| Lead author | Year of publication | Indication | No. of patients | Intervention | Surgical technique |
|---|---|---|---|---|---|
| Thaler et al. | 2022 | Periprosthetic fracture | 3 | Direct reattachment; sleeve osteotomy | #5 Ethibond to attach the gluteus medius muscle to the lateral and medial aspects of the prosthesis with sutures running through the muscles or the tendons of the muscles and the predefined holes at the implant site |
| If severe instability, the connection between the proximal femoral replacement and the acetabulum can be fortified using a mesh reinforcement. Either an 8-mm Dacron vascular graft or mesh can be looped around the proximal femoral replacement body and secured using #5 Ethibond. The other end of the Dacron vascular graft is secured to the ilium proximal to the acetabular component using 4.5-mm cortical large fragment screws with washers, that is two to four monofilament wires, with different techniques of tunnels in a vertical and horizontal plane through the osteotomized fragment, eventually with claw plates, cables or standard plates | |||||
| Shih et al. | 2007 | Hip fracture; OA; osteonecrosis | 5; 3; 3 | Direct reattachment; sleeve osteotomy | Non adsorbable sutures to fix tendons to the modular megaprosthesis. If the bone stock of the greater trochanter is poor or absent, abductors are attached to the megaprosthesis using Mersilene tape. Onlay allografts can be used to reconstruct the junction of the host femur and the porous surface of the prosthesis in some cases |
| Wire fixation of the greater trochanter to the megaprosthesis | |||||
| Bickels et al. | 2000 | Renal osteodystrophy | 2 | Direct reattachment; sleeve osteotomy | If the trochanter is resected on the first place, a metal loop with Dacron tape to secure the tendons to the implant |
| Reattachment of the trochanter with a cable grip system | |||||
| Parvizi et al. | 2004 | No report | 49 | Sleeve osteotomy; tendon to muscle | The tendon complex is around the prosthesis with multiple loops of nonabsorbable sutures passing around the remnant of trochanter and the attached soft tissue. The trochanter is fixed onto the proximal portion of the prosthesis by passing the sutures through the holes in the prosthesis or around the proximal body and the deep tissues |
| The abductors are sutured to the vastus lateralis, the tensor fascia lata, or the host greater trochanter, if available. Abductors mechanism can be attached to the vastus lateralis or the tensor fascia lata muscle | |||||
| Amanatullah et al. | 2014 | Infection; periprosthetic fracture; aseptic loosening; combination | 1; 2; 3; 13 | Sleeve osteotomy | Wagner type transtrochanteric osteotomy wrapped around the implant with wires or cables |
| Christ et al. | 2021 | Infection; periprosthetic fracture; aseptic loosening; combination | 2; 5; 5; 4 | Sleeve osteotomy | Detachment and fixation of the trochanteric bone and the abductors to the prosthesis |
| Giurea et al. | 1998 | Revision THA | 3 | Direct reattachment; Tendon to muscle suture | Fixation of the gluteus medius tendon and a its bony insertion to the prosthesis with a polyethylene spiked plate and screws |
| Reattachment of gluteus medius to the iliotibial band | |||||
| Ward et al. | 1995 | Failed megaprosthesis; non-unions | 1; 2 | Tendon to muscle suture | The abductor mechanism was reattached with a suture of the abductors to the prosthesis, providing additional continuity by tenodesing the abductor and short external rotator tendons to the undersurface of the overlying iliotibial band, tensor muscle, and gluteus maximus tendon |
| Innocenti et al. | 2021 | IM nail failure | 15; 6 | Tendon to tendon suture; synthetic augmentation | Tendon to tendon or tendon to muscle suture “bridge” between the abductors and the vastus lateralis and/or tensor fascia lata muscle without complementary devices |
| If residual instability or laxity of the joint, insert the Trevira tube around the neck segments of the implant to both directly connect the proximal body of the prostheses with the remained native hip capsule and wrap the remaining fragments of the trochanter or the abductor tendons themself with the synthetic tube with the use of multiple loop non-adsorbable sutures | |||||
| Gosheger et al. | 2001 | Pseudoarthrosis; failed megaprosthesis | 1; 1 | Synthetic augmentation | The tube is fixed to the megaprosthesis and the muscles are reattached to the prosthesis. Use non-absorbable sutures for attachments to the Trevira tube |
OA, osteoarthritis; THA, total hip arthroplasty.
Direct reattachment
Direct reattachment of the abductor musculature to the proximal body of the megaprosthesis that often come with multiholes. This is a relatively quick and easily accessible method to recreate abductor mechanism continuity if tendons were spared on the first instance (21,23,24).
Trochanter sleeve osteotomy
If a fragment of the greater trochanter remains in place, a trochanteric sleeve osteotomy can be performed with the trochanteric fragment mounted on the PFR prosthesis during reconstruction. The reattachment can be performed throughout claw plates, standard plates, or just cables or non-adsorbable sutures (8,21,25,26).
Tendon-to-muscle suture
The abductor tendons/musculature are sutured to the other surrounding hip muscle groups in a sort of elastic slingshot conformation. This method does not compel touching the bone or the prosthesis and is a pure tendon-to-muscle suture technique (9,25,27,28).
Synthetic augmentation
A synthetic porous structure made of polyethylene terephthalate can be wrapped around the proximal portion of the megaprosthesis running as the attachment for both the gluteus musculature and the other muscles surrounding the hip joint as well as the remaining hip capsular structures (9,29).
Discussion
The majority of the current evidence about techniques for hip abductor mechanism reconstruction comes from oncological reports or describes methods for chronic abductor mechanism deficiency in total hip revision surgery with the use of revision stems and not proximal femur megaprosthesis. Hereafter, for the thoroughness of this work, different methods for abductor reattachment in revision arthroplasty not mentioning megaprosthesis are reported.
Whiteside et al. (30) describe a surgical technique to restore the hip stability based on the factual assumption that deficiency of the abductor muscle group does not generally affect the gluteus maximus, allowing the muscle transfer. The gluteus maximus is detached anteriorly from the fascia lata as far proximally as the iliac crest and posteriorly from its insertion to the iliotibial band as far proximally as half of the length of the muscle. This muscle flap can be attached directly to the greater trochanter and vastus lateralis muscle in a tendon-to-muscle suture fashion. In situations involving capsular deficiency, posterior instability, or absence of the short external rotator muscles, an additional triangular flap can be raised from the posterior portion of the gluteus maximus muscle and transferred under the main anterior gluteus maximus flap and greater trochanter to attach to the anterior capsule. This flap substitutes for the gluteus minimus muscle and short external rotators and capsules and helps limit excessive internal rotation and adduction of the hip.
Fehm et al. (31) report a surgical reconstruction technique with fresh-frozen Achilles tendon and calcaneal bone allograft for the treatment of severe abductor deficiency after total hip arthroplasty. The tendinous portion of the allograft is passed through the gluteus medius muscle and then is looped back on itself while the osseous block is press-fit into an ad-hoc recess on the femoral bone and fixed with a 16-gauge wire or with a cable passed around the bone block and the femur itself. Finally, the two end extremities of the tendinous portion of the allograft are suture one to the other, to the gluteus minimus, to the capsule anteriorly and to the intact area of the gluteus medius tendon in similar manner posteriorly.
Drexler et al. (32) describe a similar method to the ones proposed before with the gluteus minimus and the posterior half of the gluteus medius sutured together and then sutured to the upper edge of the vastus lateralis using nonabsorbable #2 Ticron and #5 Ticron wires. Additionally, the anterior half of the gluteus medius is repaired both to the greater trochanter and to the vastus lateralis with intraosseous sutures. Once the repair of the abductor muscles is obtained, an augmentation with tensor fascia lata (TFL) is performed. The posterior aspect of TFL is sutured to the abductor musculature and to the superior margin of the vastus lateralis insertion. Ultimately, the anterior aspect of TFL is sutured to the iliotibial band and the gluteus maximus.
Acute and chronic tears abductor mechanism deficiency secondary to primary THA open treatment algorithm was attempted to be built by Kenanidis et al. (33). The group found no sufficient data through the literature to draw any conclusion for the primary purpose of the study, but the resulting surgical technique does not deviate from the ones this article presents. Direct suturing of the tendon defect can be resolved with drilled holes and suture anchors through the greater trochanter. Kenanidis propose the use of anchors of smaller tears of the gluteus tendon, while transosseous tunnels can be performed to repair stout posterior fibers of the abductor muscle with the number of the bone tunnel directly proportional to the extent of the tendon tear. Direct open augmented repair with synthetic grafts or allografts can also be achieved using suture anchors and a non-resorbable collagen patch. Kenanidis found this technique to be presented in studies including patients with a higher grade of deficiency of the tendon compared to the one supporting direct suturing. Lastly, reconstruction for chronic end-stage abductor tears is preferably treated with muscle transfer.
Limitations
A limitation of this review is the non-standardized pre- and post-operative evaluation of patients and their clinical and radiological outcomes described in the presented literature. Another limitation is the lack of an explicit and reproducible methodology by which the evidence has been reviewed with quantitative means.
New scientific evidence should be produced with rigorous and standardized methods in order to systematically synthesize data to develop a better treatment algorithm of which surgical technique should be chosen in complex hip revision surgery or catastrophic proximal femur fracture fixation failures with massive proximal femoral bone loss.
Conclusions
In this review, the abductor mechanism reattachment in PFR with megaprosthesis for non-oncological reasons is presented with different techniques that can be divided and summarized into four different groups: direct suture to the prosthesis, trochanteric sleeve osteotomy, muscle-to-muscle suture, and synthetic tube augmentation suture. To the author’s knowledge, no review dealing with such topic has ever been reported before.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Giuseppe Solarino and Giuseppe Marongiu) for the series “Modular Implants for Revision Arthroplasty in Orthopedics” published in Annals of Joint. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-26/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-26/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-26/coif). The series “Modular Implants for Revision Arthroplasty in Orthopedics” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [Crossref] [PubMed]
- Gwam CU, Mistry JB, Mohamed NS, et al. Current Epidemiology of Revision Total Hip Arthroplasty in the United States: National Inpatient Sample 2009 to 2013. J Arthroplasty 2017;32:2088-92. [Crossref] [PubMed]
- Innocenti M, Smulders K, Willems JH, et al. Patient-reported outcome measures, complication rates, and re-revision rates are not associated with the indication for revision total hip arthroplasty: a prospective evaluation of 647 consecutive patients. Bone Joint J 2022;104-B:859-66. [Crossref] [PubMed]
- Haentjens P, Casteleyn PP, Opdecam P. Hip arthroplasty for failed internal fixation of intertrochanteric and subtrochanteric fractures in the elderly patient. Arch Orthop Trauma Surg 1994;113:222-7. [Crossref] [PubMed]
- Haidukewych GJ, Berry DJ. Salvage of failed treatment of hip fractures. J Am Acad Orthop Surg 2005;13:101-9. [Crossref] [PubMed]
- Hassankhani EG, Omidi-Kashani F, Hajitaghi H, et al. How to Treat the Complex Unstable Intertrochanteric Fractures in Elderly Patients? DHS or Arthroplasty. Arch Bone Jt Surg 2014;2:174-9. [PubMed]
- Vaishya R, Thapa SS, Vaish A. Non-neoplastic indications and outcomes of the proximal and distal femur megaprosthesis: a critical review. Knee Surg Relat Res 2020;32:18. [Crossref] [PubMed]
- Amanatullah DF, Trousdale RT, Hanssen AD, et al. Non-oncologic total femoral arthroplasty: retrospective review. J Arthroplasty 2014;29:2013-5. [Crossref] [PubMed]
- Innocenti M, Guido D, Cozzi Lepri A, et al. Proximal femoral replacement: A salvage treatment of cephalomedullary nails' mechanical failures in the elderly population. Injury 2021;52:1868-74. [Crossref] [PubMed]
- Rasouli MR, Porat MD, Hozack WJ, et al. Proximal femoral replacement and allograft prosthesis composite in the treatment of periprosthetic fractures with significant proximal bone loss. Orthop Surg 2012;4:203-10. [Crossref] [PubMed]
- Sakellariou VI, Babis GC. Management bone loss of the proximal femur in revision hip arthroplasty: Update on reconstructive options. World J Orthop 2014;5:614-22. [Crossref] [PubMed]
- Klein GR, Parvizi J, Rapuri V, et al. Proximal femoral replacement for the treatment of periprosthetic fractures. J Bone Joint Surg Am 2005;87:1777-81. [PubMed]
- Sim FH. CORR Insights®: Upshifting the Ipsilateral Proximal Femur May Provide Satisfactory Reconstruction of Periacetabular Pelvic Bone Defects After Tumor Resection. Clin Orthop Relat Res 2018;476:1771-2. [Crossref] [PubMed]
- Fahad S, Nawaz Khan MZ, Khattak MJ, et al. Primary Proximal femur replacement for unstable osteoporotic intertrochanteric and subtrochanteric fractures in the elderly: A retrospective case series. Ann Med Surg (Lond) 2019;44:94-7. [Crossref] [PubMed]
- Innocenti M, Muratori F, Foschi L, et al. Salvage of limb salvage in oncological reconstructions of the lower limb with megaprosthesis: how much to push the boundaries? Arch Orthop Trauma Surg 2023;143:763-71. [Crossref] [PubMed]
- Ahlmann ER, Menendez LR, Kermani C, et al. Survivorship and clinical outcome of modular endoprosthetic reconstruction for neoplastic disease of the lower limb. J Bone Joint Surg Br 2006;88:790-5. [Crossref] [PubMed]
- Lee SH, Oh JH, Lee KS, et al. Infection after prosthetic reconstruction in limb salvage surgery. Int Orthop 2002;26:179-84. [Crossref] [PubMed]
- Henderson ER, Groundland JS, Pala E, et al. Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. J Bone Joint Surg Am 2011;93:418-29. [Crossref] [PubMed]
- Elbuluk AM, Coxe FR, Schimizzi GV, et al. Abductor Deficiency-Induced Recurrent Instability After Total Hip Arthroplasty. JBJS Rev 2020;8:e0164. [Crossref] [PubMed]
- Brooks PJ. Dislocation following total hip replacement: causes and cures. Bone Joint J 2013;95-B:67-9. [Crossref] [PubMed]
- Bickels J, Meller I, Henshaw RM, et al. Reconstruction of hip stability after proximal and total femur resections. Clin Orthop Relat Res 2000;218-30. [Crossref] [PubMed]
- Ritschl P, Capanna R, Helwig U, et al. KMFTR (Kotz Modular Femur Tibia Reconstruction System) modular tumor endoprosthesis system for the lower extremity. Z Orthop Ihre Grenzgeb 1992;130:290-3. [Crossref] [PubMed]
- Thaler M, Manson TT, Holzapfel BM, et al. Proximal femoral replacement using the direct anterior approach to the hip. Oper Orthop Traumatol 2022;34:218-30. [Crossref] [PubMed]
- Shih ST, Wang JW, Hsu CC. Proximal femoral megaprosthesis for failed total hip arthroplasty. Chang Gung Med J 2007;30:73-80. [PubMed]
- Parvizi J, Sim FH. Proximal femoral replacements with megaprostheses. Clin Orthop Relat Res 2004;169-75. [Crossref] [PubMed]
- Christ AB, Fujiwara T, Fabbri N, et al. Compliant Compression Reconstruction of the Proximal Femur Is Durable Despite Minimal Bone Formation in the Compression Segment. Clin Orthop Relat Res 2021;479:1577-85. [Crossref] [PubMed]
- Giurea A, Paternostro T, Heinz-Peer G, et al. Function of reinserted abductor muscles after femoral replacement. J Bone Joint Surg Br 1998;80:284-7. [Crossref] [PubMed]
- Ward WG, Dorey F, Eckardt JJ. Total femoral endoprosthetic reconstruction. Clin Orthop Relat Res 1995;195-206. [Crossref] [PubMed]
- Gosheger G, Hillmann A, Lindner N, et al. Soft tissue reconstruction of megaprostheses using a trevira tube. Clin Orthop Relat Res 2001;264-71. [Crossref] [PubMed]
- Whiteside LA. Surgical technique: Transfer of the anterior portion of the gluteus maximus muscle for abductor deficiency of the hip. Clin Orthop Relat Res 2012;470:503-10. [Crossref] [PubMed]
- Fehm MN, Huddleston JI, Burke DW, et al. Repair of a deficient abductor mechanism with Achilles tendon allograft after total hip replacement. J Bone Joint Surg Am 2010;92:2305-11. [Crossref] [PubMed]
- Drexler M, Dwyer T, Kosashvili Y, et al. Acetabular cup revision combined with tensor facia lata reconstruction for management of massive abductor avulsion after failed total hip arthroplasty. J Arthroplasty 2014;29:1052-7. [Crossref] [PubMed]
- Kenanidis E, Lund B, Christofilopoulos P. A roadmap to develop clinical guidelines for open surgery of acute and chronic tears of hip abductor tendons. Knee Surg Sports Traumatol Arthrosc 2021;29:1420-31. [Crossref] [PubMed]
Cite this article as: Innocenti M, Leggieri F, Stimolo D, Carminati M, Christian C, Civinini R. Techniques for abductor reattachment in proximal femoral replacement for non-oncological reconstructions: a narrative review. Ann Joint 2024;9:20.