Abstracts
PURPOSE: To evaluate the effects of metoclopramide on the formation of adhesion and the healing of left colonic anastomoses in rats. METHODS: Forty rats underwent sectioning of the left colon and end-to-end anastomosis and were divided into two groups of 20 animals for the administration of metoclopramide (experimental group - E) or saline solution (control group - C). Each group was divided into subgroups of 10 animals each to be killed on the third (E3 and C3) or seventh postoperative day (E7 and C7). Adhesion was assessed, and a colonic segment containing the anastomosis was removed for analysis of breaking strength and hydroxyproline concentration. RESULTS: There were no deaths or dehiscence on the 3rd postoperative day. There was one death and one blocked anastomotic dehiscence in the E7 group. No significant differences between groups were found in the analysis of clinical outcome, intra-cavity adhesion, adhesion to the anastomosis or breaking strength on the 3rd and 7th postoperative day. Hydroxyproline concentration was higher in the control group on the 3rd (p=0.006) but not on the 7th postoperative day (p=0.241). CONCLUSION: Metoclopramide did not have harmful effects on the healing of intestinal anastomoses in rats.
Anastomosis, Surgical; Colon; Metoclopramide; Gastrointestinal Motility; Tissue Adhesions; Rats
OBJETIVO: Avaliar os efeitos da metoclopramida sobre a formação de aderências e a cicatrização de anastomoses de cólon esquerdo de ratos. MÉTODOS: 40 ratos distribuídos em dois grupos contendo 20 animais, para administração de metoclopramida (grupo experimental - E) ou solução de NaCl 0,9% (grupo controle - C). Cada grupo foi dividido em subgrupos contendo 10 animais, para eutanásia no terceiro (E3 e C3) ou sétimo dia (E7 e C7) de pós-operatório. Os ratos foram submetidos à secção do cólon esquerdo e anastomose término-terminal. No dia da re-laparotomia foi avaliada a quantidade total de aderências e removido um segmento colônico contendo a anastomose para análise da força de ruptura e concentração de hidroxiprolina. RESULTADOS: Não houve mortes ou deiscências no 3º dia de pós-operatório. No grupo E7 ocorreram uma morte e uma deiscência de anastomose bloqueada. Não houve diferença significativa entre os grupos em relação à evolução clínica, quantidade de aderências intra-cavitárias ou à anastomose e resistência tênsil no 3º ou 7º pós-operatório. A concentração de hidroxiprolina foi maior no grupo metoclopramida no 3º (p=0,006) mas não no 7º dia de pós-operatório (p=0,241) CONCLUSÃO: A metoclopramida não apresenta efeito deletério sobre a cicatrização de anastomoses intestinais em ratos.
Anastomose Cirúrgica; Cólon; Metoclopramida; Motilidade Gastrointestinal; Aderências Teciduais; Ratos
9 - ORIGINAL ARTICLE
ALIMENTARY TRACT
Does metoclopramide impair anastomotic healing of the left colon of rats?1 1 Research performed at Experimental Laboratory of Surgery, School of Medicine, Brasilia University (UnB), Brazil.
A metoclopramida prejudica a cicatrização de anastomoses do cólon esquerdo de ratos?
Silvana Marques e SilvaI; Vânia Maria Moraes FerreiraII; Omar FeresIII; Paulo Gonçalves de OliveiraIV; João Batista de SousaV
IFellow, PhD degree, Postgraduate Program in Medical Sciences, School of Medicine, UnB, Brasilia-DF, Brazil. Project design, implementation of procedures, statistical analyses, data analysis and manuscript writing
IIPhD, Associate Professor, Pharmaceutical Sciences, School of Health Sciences, UnB, Brasilia-DF, Brazil. Project design, data analysis and article revision
IIIPhD, Assistant Professor, Division of Coloproctology, Department of Surgery and Anatomy, Ribeirao Preto School of Medicine, Sao Paulo University, Brazil. Project design, data analysis and article revision
IVPhD, Associate Professor, Surgical Clinics, School of Medicine, UnB, Brasilia-DF, Brazil. Project design, data analysis and article revision
VPhD, Associate Professor, Surgical Clinics, School of Medicine, UnB, Brasilia-DF, Brazil. Main author, project design, implementation of procedures, statistical and data analysis, article revision
Correspondence Correspondence: João Batista de Sousa Campus Universitário Darcy Ribeiro Prédio da Reitoria, 2º pavimento, sala B2-16 70910-900 Brasília - DF Brasil Tel: (55 61)3307-2201 sousajb@unb.br
ABSTRACT
PURPOSE: To evaluate the effects of metoclopramide on the formation of adhesion and the healing of left colonic anastomoses in rats.
METHODS: Forty rats underwent sectioning of the left colon and end-to-end anastomosis and were divided into two groups of 20 animals for the administration of metoclopramide (experimental group - E) or saline solution (control group - C). Each group was divided into subgroups of 10 animals each to be killed on the third (E3 and C3) or seventh postoperative day (E7 and C7). Adhesion was assessed, and a colonic segment containing the anastomosis was removed for analysis of breaking strength and hydroxyproline concentration.
RESULTS: There were no deaths or dehiscence on the 3rd postoperative day. There was one death and one blocked anastomotic dehiscence in the E7 group. No significant differences between groups were found in the analysis of clinical outcome, intra-cavity adhesion, adhesion to the anastomosis or breaking strength on the 3rd and 7th postoperative day. Hydroxyproline concentration was higher in the control group on the 3rd (p=0.006) but not on the 7th postoperative day (p=0.241).
CONCLUSION: Metoclopramide did not have harmful effects on the healing of intestinal anastomoses in rats.
Key words: Anastomosis, Surgical. Colon. Metoclopramide. Gastrointestinal Motility. Tissue Adhesions. Rats.
RESUMO
OBJETIVO: Avaliar os efeitos da metoclopramida sobre a formação de aderências e a cicatrização de anastomoses de cólon esquerdo de ratos.
MÉTODOS: 40 ratos distribuídos em dois grupos contendo 20 animais, para administração de metoclopramida (grupo experimental - E) ou solução de NaCl 0,9% (grupo controle - C). Cada grupo foi dividido em subgrupos contendo 10 animais, para eutanásia no terceiro (E3 e C3) ou sétimo dia (E7 e C7) de pós-operatório. Os ratos foram submetidos à secção do cólon esquerdo e anastomose término-terminal. No dia da re-laparotomia foi avaliada a quantidade total de aderências e removido um segmento colônico contendo a anastomose para análise da força de ruptura e concentração de hidroxiprolina.
RESULTADOS: Não houve mortes ou deiscências no 3º dia de pós-operatório. No grupo E7 ocorreram uma morte e uma deiscência de anastomose bloqueada. Não houve diferença significativa entre os grupos em relação à evolução clínica, quantidade de aderências intra-cavitárias ou à anastomose e resistência tênsil no 3º ou 7º pós-operatório. A concentração de hidroxiprolina foi maior no grupo metoclopramida no 3º (p=0,006) mas não no 7º dia de pós-operatório (p=0,241)
CONCLUSÃO: A metoclopramida não apresenta efeito deletério sobre a cicatrização de anastomoses intestinais em ratos.
Descritores: Anastomose Cirúrgica. Cólon. Metoclopramida. Motilidade Gastrointestinal. Aderências Teciduais. Ratos.
Introduction
The incidence of anastomotic dehiscence, a potential complication of colorectal surgery, is variable and may affect 1.8 to 12% of the cases1. It is associated with increased morbidity and mortality, hospital stay and total treatment costs2.
Adhesion is a consequence of normal healing3. The physiological similarities between healing of intestinal anastomoses and formation of adhesion suggest that the agents affecting adhesion must also modulate healing.
The formation of adhesion has a beneficial effect during the critical period of anastomotic healing. This effect may be explained by the ability of these adhesions, especially those of the omentum, to supply oxygen and nutrients to the area under repair by imbibition or as a result of the development of microscopic vascular connections4. An increased risk of anastomotic dehiscence with the prevention of adhesion formation by hyaluronic acid derivatives has been described5.
According to some authors, the stimulation of gastrointestinal motility by administration of prokinetic agents reduces adhesion and changes its type6. These agents are often administered immediately after operation to help gastric emptying and speed up the resolution of the paralytic ileus.
Metoclopramide (methoxy-2-chloro-5-procainamide), an antiemetic prokinetic agent that stimulates gastrointestinal tract motility7, has been used to treat the paralytic ileus and to control vomiting postoperatively.
García-Olmo et al.8 conducted a study to determine the pharmacological effects of manipulating gastrointestinal motility on the resistance of colic anastomosis. The authors concluded that the use of metoclopramide immediately after operation was associated with a significant increase in colonic anastomotic dehiscence and, in the surviving animals, a significant decrease in anastomosis resistance.
The determination of factors detrimental to wound healing is of great clinical relevance because it may contribute to reducing the risk of dehiscence and, consequently, morbidity and mortality associated with surgery.
This study evaluated the effects of metoclopramide on the formation of adhesion and the healing of left colonic anastomoses in rats.
Methods
This study was conducted in the Laboratory of Experimental Surgery, School of Medicine, Brasilia University (UnB) and approved by the Ethics Committee on Animal Use (CEUA) -Institute of Biological Sciences, UnB. The study was conducted in accordance with the guidelines of the Brazilian College of Animal Experiments (COBEA).
Forty healthy male Wistar rats (Rattus norvegicus) aged 90 to 120 days and weighing 361 to 566g were included in the study. Before operation, they were kept for two weeks in cages with five animals each and 12:12-hour artificial light to dark cycles. The rats received standard diet and water ad libitum. There was no preoperative fasting.
The rats were distributed according to block randomization into two groups of 20 animals each for postoperative administration of metoclopramide (experimental group - E) or saline solution (control group - C). Later, another block randomization was conducted to generate subgroups of 10 animals each to be killed on the third or seventh postoperative day (Figure 1).
General anesthesia was achieved using IM administration of 10 mg/kg xylazine hydrochloride and 75 mg/kg of ketamine hydrochloride. All surgeries were performed by the same surgeon. A midline incision of 4.0 cm in length started 1.0 cm above the external genitalia of animals. The distal colon was exposed, and a 0.5 cm segment of the left colon was resected at about 2.5 above the peritoneal reflection, and end-to-end segment anastomosis was performed in a single transmural layer using 6.0-nylon suture in running stitches and a cylindrical needle. The abdominal wall was closed in two planes using 3.0-silk continuous stitches.
After the operations, metoclopramide was administered to the corresponding subgroups in doses of 1 mg/100 g subcutaneously every 12 hours until the animal was killed. The control animals received identical volumes of 0.9% NaCl subcutaneously every 12 hours.
After operation, clinical patterns of apathy, bristling hair, diarrhea, abdominal distension and wound complications, such as hematomas and signs of infection at the surgical site, were evaluated.
Re-operation was performed on the day determined for each subgroup. After exposure of the abdominal cavity, signs of peritonitis, abscess, or anastomotic dehiscence were evaluated. The total amount of intra-abdominal adhesion was evaluated using the Nair score9:
0- no adhesion;
1-single band between viscera or between viscera and abdominal wall;
2 - two bands between viscera or between viscera and abdominal wall;
3 - more than two bands between viscera or between viscera and abdominal wall, or the entire intestine forming a mass adhering to the abdominal wall;
4 - viscera directly attached to the abdominal wall, regardless of number or extent of bands.
A colonic segment of 4.0 cm in length containing the anastomosis in its central portion was removed together with the structures attached to it. After that, the type of structure attached to the anastomosis was evaluated. The amount of adhesion was evaluated according to the proportion of anastomosis covered by it.
The surgical specimen was opened through the antimesenteric border and divided into longitudinal segments for further analysis of the tensile strength by means of a digital test apparatus named Versa Test (Mecmesin Versa Test, United Kingdom) coupled to a digital dynamometer AGF (Mecmesin Versa Test, United Kingdom). The rectangular fragment of tissue was fixed at both ends by the upper clamp of the dynamometer and the bottom clamp of the Versa Test, with the anastomotic region equidistant and parallel to the clamps. The speed used during the test was 30 mm/min10. The breaking value was reported in Newtons (N).
The hydroxyproline concentration was determined using the modified technique described by Stegemann & Stalder 10,11.
The SPSS® software was used for statistical analyses. The Student t test for independent samples was used to compare breaking strength and hydroxyproline concentration between groups at each time point. The Fisher exact test was used to compare categorical variables (adhesion). The level of statistical significance was set at p<0.05.
Results
There were no deaths or dehiscence in either group on the 3rd postoperative day. Clinical progression was similar for apathy, bristling hair and diarrhea. No animal had abdominal distention, hematoma or surgical site infection. There was one death in the E7 group. Clinical outcomes were similar between groups on the 7th postoperative day.
No animal had signs of peritonitis in the abdominal cavity according to the evaluation during re-operation. One animal of the E7 group had anastomotic dehiscence blocked by adjacent organs and noticed only after the opening of the surgical specimen. No animals of the C3, E3 and C7 groups had anastomotic dehiscence.
Intra-abdominal adhesion was similar between groups on the 3th postoperative day, but lower in the metoclopramide group on the 7th postoperative day, but the difference was not statistically significant (Table 1).
The percentage of anastomosis covered by adhesion was lower in the metoclopramide group on the 3rd, but not on the 7th, postoperative day, but the difference was not statistically significant (Table 2).
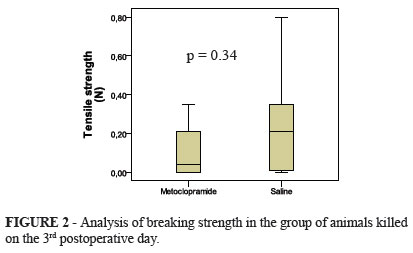
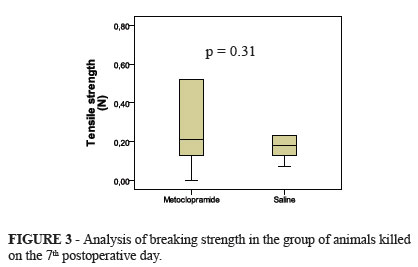
In the E3 group there was a lower anastomotic breaking strength value than in the C3 group (p=0.34), but the difference was not statistically significant (Figure 2). However, breaking strength was higher, but not statistically different, in the E7 group (p=0.31) (Figure 3).
Hydroxyproline concentrations were higher in the metoclopramide group on the 3rd postoperative day (p=0.006). There were no significant differences in hydroxyproline concentration between groups on the 7th postoperative day (p=0.241).
Discussion
Metoclopramide is a prokinetic agent used postoperatively to treat gastroesophageal reflux, nausea, vomiting and gastrointestinal motility disorders. Its action is associated with blocking the dopamine receptor-2 (D2) in the central nervous system and gastrointestinal tract.
Dopamine antagonists decrease the activity of the vomiting center and the activation of visceral nerves12. Moreover, there is inhibition of the gastrointestinal tract, and relaxation or inhibition of the smooth muscle contraction from esophagus to colon13. Thus, the inhibition of dopamine receptors has a prokinetic effect. Specific dopamine receptors have been described in the gastrointestinal tract14, particularly the stomach and the exocrine pancreas, as well as in the renal, mesenteric, coronary and cerebral vasculature. D2 receptors are both pre- and postjunctional and exert negative modulation on the acetylcholine release in the terminals of the intrinsic cholinergic nerves13.
Stimulation of the gastrointestinal tract using metoclopramide, similarly to other benzamide derivatives, appears to be mediated, at least in part, by its indirect cholinergic activity, partly dependent on its anticholinesterase properties.
Stimulation of the gastrointestinal motility using prokinetic agents may be deleterious if it affects anastomotic healing by direct mechanical action or by reducing adhesion formation4.
García-Olmo et al.8 conducted a study to determine the pharmacological effects of manipulating gastrointestinal motility on the resistance of colic anastomosis. Seventy-two rats underwent colon anastomosis and were randomized into three groups that received 1 ml of saline solution, metoclopramide (1.2 mg/100 g body weight) or hyoscine (2 mg/100 g body weight) administered subcutaneously. Animals were killed on the fourth postoperative day. The authors concluded that the use of metoclopramide immediately after the operation was associated with a significant increase in colonic anastomotic dehiscence, and in the surviving animals, a significant decrease in anastomotic resistance. Hyoscine, an inhibitor of gastrointestinal motility, did not improve healing. They found a strong correlation between anastomosis resistance and its proportion covered by adjacent organs. The group of animals administered prokinetic agents had greater intra-abdominal adhesion; however, less adhesion was beneficial, as found between adjacent organs and the anastomosis on the fourth postoperative day.
Springall and Spitz15 studied the effect of cisapride on postoperative adhesion and anastomotic strength. Twenty Wistar rats receiving cisapride subcutaneously were compared with twenty control animals that received saline solution using a similar protocol. The treated group had significantly less adhesion, but the enhanced motility did not affect anastomotic strength on the 7th postoperative day. Mortality rates were not reported.
In our study, there were no deaths or dehiscence in either group on the 3rd postoperative day. Animals receiving metoclopramide or saline solution had similar abdominal adhesions scores on the 3rd postoperative day, but the experimental group had less adhesion between adjacent organs and the anastomosis. This might explain the decrease in anastomotic breaking strength in the study group when compared to the control group. During healing, the initial anastomotic resistance depends on the suture, because, up to the fourth day, the anastomosis is filled with loose and disorganized collagen fibers. This resistance might also be dependent on blocking by adjacent organs, which act as a protective factor for anastomosis. Between the fifth and seventh days, the peak of collagen synthesis by fibroblasts occurred and the anastomotic strength was primarily dependent on these new organized fibers16. The statistically significant decrease of hydroxyproline levels of anastomosis evaluated on the third postoperative day might, therefore, have no clinical importance.
On the 7th postoperative day, we had one death in group E7, but it was not associated with anastomotic insufficiency. However, this group had only one blocked anastomotic dehiscence. In the metoclopramide group, there was less abdominal adhesion, but the number of adhesion bands between adjacent organs and the anastomosis was similar between groups. There were no statistical differences in anastomotic breaking strength, but it was higher in the study group. Although unexpected, the metoclopramide group had lower hydroxyproline levels than the control group, though the difference was not significant. However, hydroxyproline levels need not always be parallel to other parameters of wound healing17-20. Treatment with metoclopramide may mediate healing via a different pathway without affecting hydroxyproline levels.
The differences between groups were not statistically significant, and there was no major interference in clinical parameters. Animals had a similar postoperative clinical progression and no cases of peritonitis or deaths associated with anastomotic insufficiency were found in either group. Furthermore, anastomotic dehiscence that occurred in the study group was blocked by adjacent organs and was detected only after the opening of the surgical specimen. Therefore, these animals showed no clinical consequences of this complication.
Conclusion
The metoclopramide had no harmful effects on the healing of intestinal anastomosis in rats.
Received: December 10, 2010
Review: February 14, 2011
Accepted: March 15, 2011
Conflict of interest: none
Financial source: none
- 1. Uzun MA, Koksal N, Ozkan OF, Kayahan M, Gumrukcu G. Salvage repair of anastomotic dehiscence following colon surgery using an expanded polytetrafluoroethylene graft. Tech Coloproctol. 2010 Aug 6 [Epub ahead of print]
- 2. Eberl T, Jagoditsch M, Klingler A, Tschmelitsch J. Risk factors for anastomotic leakage after resection for rectal cancer. Am J Surg. 2008;196(4):592-8.
- 3. Liakakos T, Thomakos N, Fine PM, Dervenis C, Young RL. Peritoneal adhesions: etiology, pathophysiology, and clinical significance. Recent advances in prevention and management. Dig Surg. 2001;18(4):260-73.
- 4. Garcia-Olmo D, Lucas FJ, Paya J. Relationship between peritoneal adhesion phenomena and the experimental resistance of colonic anastomoses: influence of omentoplasty. Eur Surg Res. 1996;28(4):315-22.
- 5. Beck DE, Cohen Z, Fleshman JW, Kaufman HS, van Goor H, Wolff BG. A prospective, randomized, multicenter, controlled study of the safety of Seprafilm adhesion barrier in abdominopelvic surgery of the intestine. Dis Colon Rectum. 2003;46(10):1310-9.
- 6. Springall RG, Spitz L. Prevention of post-operative adhesions using a gastrointestinal prokinetic agent. J Pediatr Surg. 1989;24(6):530-3.
- 7. Tonini M, Cipollina L, Poluzzi E, Crema F, Corazza GR, De Ponti F. Review article: clinical implications of enteric and central D2 receptor blockade by antidopaminergic gastrointestinal prokinetics. Aliment Pharmacol Ther. 2004;19(4):379-90.
- 8. Garcia-Olmo D, Paya J, Lucas FJ, Garcia-Olmo DC. The effects of the pharmacological manipulation of postoperative intestinal motility on colonic anastomoses. An experimental study in a rat model. Int J Colorectal Dis. 1997;12(2):73-7.
- 9. Nair SK, Bhat IK, Aurora AL. Role of proteolytic enzyme in the prevention of postoperative intraperitoneal adhesions. Arch Surg. 1974;108(6):849-53.
- 10. Stegemann H, Stalder K. Determination of hydroxyproline. Clin Chim Acta. 1967;18:267-73.
- 11. Medugorac I. Collagen content in different areas of normal and hypertrophied rat myocardium. Cardiovasc Res. 1980;14(9):551-4.
- 12. Oksuz H, Zencirci B, Ezberci M. Comparison of the effectiveness of metoclopramide, ondansetron, and granisetron on the prevention of nausea and vomiting after laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2007;17(6):803-8.
- 13. Tonini M. Recent advances in the pharmacology of gastrointestinal prokinetics. Pharmacol Res. 1996;33(4-5):217-26.
- 14. Zizzo MG, Mule F, Mastropaolo M, Serio R. D1 receptors play a major role in the dopamine modulation of mouse ileum contractility. Pharmacol Res. 2010;61(5):371-8.
- 15. Sparnon AL, Spitz L. Pharmacological manipulation of postoperative intestinal adhesions. Aust N Z J Surg. 1989;59(9):725-9.
- 16. Haciyanli M, Fuzun M, Unek T, Tokgoz Z. Does the administration route of leucovorin have any influence on the impairment of colonic healing caused by intraperitoneal 5-fluorouracil treatment? Eur Surg Res. 2001;33(2):80-5.
- 17. Sousa JB, Soares EG, Aprilli F. Effects of diclofenac sodium on intestinal anastomotic healing. Experimental study on the small intestine of rabbits. Dis Colon Rectum. 1991;34(7)613-7.
- 18. Oliveira PG, Soares EG, Aprilli F. Influence of misoprostol, a synthetic prostaglandin E1 analog, on the healing of colonic anastomoses in rats. Dis Colon Rectum. 1994;37(7)660-3.
- 19. Agalar F, Hamaloglu E, Daphan C, Tarim A, Onur R, Renda N, Sayek I. Effects of CO2 insufflation and laparotomy on wound healing in mice. Aust N Z J Surg. 2000;70(10):739-42.
- 20. Karataş A, Kocael A, Aytaç E, Gökcal F, Salihoğlu Z, Uzun H, Paksoy M. Amelogenin (an extracellular matrix protein) application on ischemic colon anastomosis in rats. Ulus Travma Acil Cerrahi Derg. 2010;16(6):487-90.
Publication Dates
-
Publication in this collection
25 July 2011 -
Date of issue
Aug 2011
History
-
Reviewed
14 Feb 2011 -
Received
10 Dec 2010 -
Accepted
15 Mar 2011