Pitiriasis rosada, una reacción exantemática
Pityriasis rosea, an exanthematous reaction
DOI:
https://doi.org/10.15446/cr.v7n2.95527Palabras clave:
Dermatología, Pitiriasis rosada, Exantema (es)Dermatology , Pityriasis Rosea , Exanthema (en)
Descargas
Las urgencias dermatológicas son eventos poco frecuentes que pueden
ser causados por alteraciones agudas de la salud, con o sin afectación
sistémica, o por enfermedades crónicas cuando se presentan cuadros de agudización.
Dermatological emergencies are rare events that can be caused by
acute medical conditions, with or without systemic involvement, or by
chronic diseases when exacerbation is observed.
https://doi.org/10.15446/cr.v7n2.95527
Pityriasis rosea, an exanthematous reaction
Editorial
Michel Faizal-Geagea
Universidad Nacional de Colombia
- Bogotá Campus - Faculty of Medicine -
Department of Internal Medicine
- Bogotá, D.C. - Colombia.
Academia Nacional de Medicina de Colombia - Bogotá, D.C. - Colombia.
Corresponding author
Michel Faizal Geagea.
Facultad de Medicina,
Universidad Nacional de Colombia.
Bogotá, D.C. Colombia.
Email: mfaizalg@unal.edu.co.
Received: 25/03/2021 Accepted: 05/04/2021
Dermatological emergencies are rare events that can be caused by acute medical conditions, with or without systemic involvement, or by chronic diseases when exacerbation is observed.
Exanthematous diseases are one of the leading causes of dermatological emergencies and may include a broad spectrum of diagnoses. Depending on their causes, they are classified as infectious (viral, bacterial, parasitic, and fungal), immunological, inflammatory, neoplastic, or caused by adverse drug reactions. The diagnosis of an exanthem is based on the patient’s medical history; however, in some cases it is necessary to perform complementary laboratory tests and pathology studies to confirm it.
Pityriasis rosea (PR) was first described in 1860 by Dr. Camille Melchior Gibert, a renowned French dermatologist who opposed the iconography of the time by stressing that “to get to know things in depth, you must first see them. Nothing can replace direct observation, which can only be done by a professional physician” (1).
PR is an exanthematous disease of sudden onset that in some cases appears after experiencing mild symptoms similar to those of an upper respiratory infection. It usually begins with a small, fawn-colored, oval-shaped plaque with fine scales along the borders of the ring, which Louis-Anne-Jean Brocq named primitive or herald patch in 1897 (1). Then, 2 weeks after the onset of symptoms, multiple annular or rounded, reddish, scaling plaques, smaller than the initial lesion, appear in a linear pattern or in the shape of a “Christmas tree.” Lesions caused by PR may be vesicular in nature and have hypopigmented macules during the involution phase.
This disease is more common in people between the ages of 15 and 40 and usually has a spontaneous resolution (2-4). Its diagnosis is based on clinical findings and laboratory tests, but syphilis serology (VDRL and FT-ABS) and mycology tests (2-4) should be requested for confirmation; a skin biopsy may also be necessary. The main differential diagnoses of this condition are syphilis, tinea, and other exanthematous diseases (5).
The main cause of PR is reactivation of human herpesviruses 6 and 7 (6), and its treatment is based on topical corticosteroids, UVB phototherapy, emollients, oral acyclovir (7-10) or erythromycin at a dose of 25-40 mg/kg/day or 250mg every 8 hours for 15 days in adults (9).
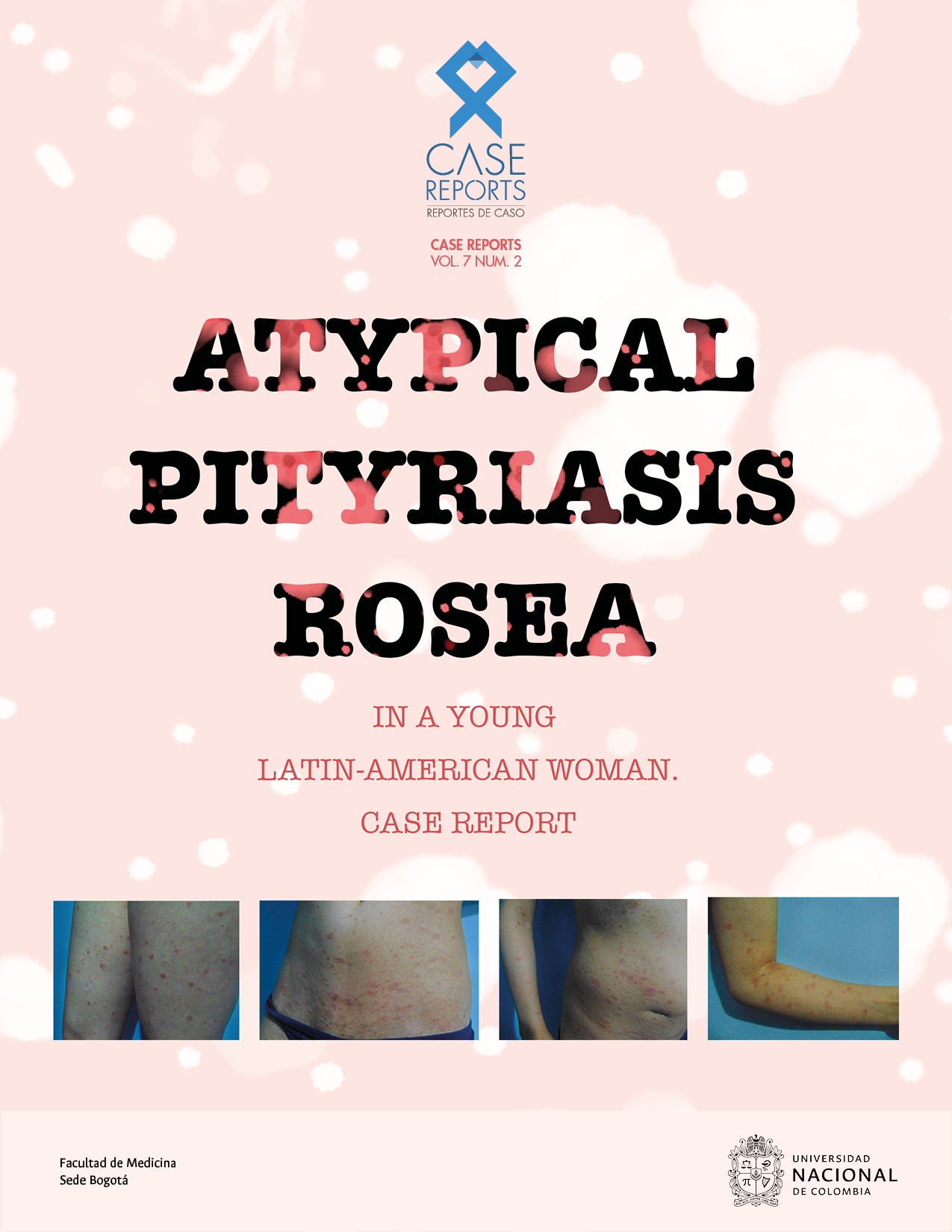
The current issue of Case Reports presents the case of a 28-year-old woman diagnosed with PR and treated with deflazacort 30mg for 21 days, who had a favorable evolution and complete improvement of symptoms after 2 months (11). With this article, the authors stress the relevance of performing an in-depth study of the medical history, the diagnostic difficulties of this condition, and the differential diagnoses to be considered. Likewise, this case report stands out as evidence of the importance of primary care physicians having adequate training in dermatology so that they can recognize and treat PR, since its diagnosis is eminently clinical, and it can have multiple atypical presentations. In this sense, it will surely be a reference text.
References
1.Wallach D, Tilles G. La Dermatología en Francia. Ediciones Privat; 2002
2.Chuang TY, IIstrup DM, Perry HO, Kurland LT. Pityriasis rosea in Rochester, Minnesota, 1969 to 1978: a 10-year epidemiologic study. J Am Acad Dermatol. 1982;7(1): 80-9. https://doi.org/cfw7kr.
3.Hartley AH. Pityriasis rosea. Pediatr Rev. 1999;20(8): 266-9. https://doi.org/cwrdmc.
4.Allen RA, Janniger CK, Schwartz RA. Pityriasis rosea. Cutis. 1995;56(4):198-202.
5.Balci DD, Hakverdi S. Vesicular pityriasis rosea: an atypical presentation. Dermatol Online J. 2008;14(3):6.
6.Drago F, Broccolo F, Rebora A. Pityriasis rosea: an update with a critical appraisal of its possible herpes viral etiology. J Am Acad Dermatol. 2009;61(2):303-18. https://doi.org/bf89nq.
7.Drago F, Rebora A. Treatment for pityriasis rosea. Skin Therapy Lett. 2009;14(3):6-7.
8.Leenutaphong V, Jiamton S. UVB phototherapy for pityriasis rosea: a bilateral comparison study. J Am Acad Dermatol. 1995;33(6):996-9. https://doi.org/fqnmmg.
9.Drago F, Vecchio F, Rebora A. Use of high-dose acyclovir in pityriasis rosea. J Am Acad Dermatol. 2006;54(1):82-5. https://doi.org/b9sqbv.
10.Sharma PK, Yadav TP, Gautam PK, Taneja N, Satyanarayana L. Erythromycin in pityriasis rosea: a double-blind, placebo-controlled clinical trial. J Am Acad Dermatol. 2000;42(2 Pt 1):241-4. https://doi.org/fvbnmv.
11.Porras-Villamil JF, Hinestroza AG, López-Moreno GA, Parra-Sepúlveda DJ. Atypical pityriasis rosea in a young Colombian woman. Case report. Case Reports. 2021;7(2):8-21.
Referencias
Wallach D, Tilles G. La Dermatología en Francia. Ediciones Privat; 2002
Chuang TY, IIstrup DM, Perry HO, Kurland LT. Pityriasis rosea in Rochester, Minnesota, 1969 to 1978: a 10-year epidemiologic study. J Am Acad Dermatol. 1982;7(1): 80-9. https://doi.org/cfw7kr. DOI: https://doi.org/10.1016/S0190-9622(82)80013-3
Hartley AH. Pityriasis rosea. Pediatr Rev. 1999;20(8): 266-9. https://doi.org/cwrdmc. DOI: https://doi.org/10.1542/pir.20-8-266
Allen RA, Janniger CK, Schwartz RA. Pityriasis rosea. Cutis. 1995;56(4):198-202.
Balci DD, Hakverdi S. Vesicular pityriasis rosea: an atypical presentation. Dermatol Online J. 2008;14(3):6. DOI: https://doi.org/10.5070/D368K916PH
Drago F, Broccolo F, Rebora A. Pityriasis rosea: an update with a critical appraisal of its possible herpes viral etiology. J Am Acad Dermatol. 2009;61(2):303-18. https://doi.org/bf89nq. DOI: https://doi.org/10.1016/j.jaad.2008.07.045
Drago F, Rebora A. Treatment for pityriasis rosea. Skin Therapy Lett. 2009;14(3):6-7.
Leenutaphong V, Jiamton S. UVB phototherapy for pityriasis rosea: a bilateral comparison study. J Am Acad Dermatol. 1995;33(6):996-9. https://doi.org/fqnmmg. DOI: https://doi.org/10.1016/0190-9622(95)90293-7
Drago F, Vecchio F, Rebora A. Use of high-dose acyclovir in pityriasis rosea. J Am Acad Dermatol. 2006;54(1):82-5. https://doi.org/b9sqbv. DOI: https://doi.org/10.1016/j.jaad.2005.06.042
Sharma PK, Yadav TP, Gautam PK, Taneja N, Satyanarayana L. Erythromycin in pityriasis rosea: a double-blind, placebo-controlled clinical trial. J Am Acad Dermatol. 2000;42(2 Pt 1):241-4. https://doi.org/fvbnmv. DOI: https://doi.org/10.1016/S0190-9622(00)90132-4
Porras-Villamil JF, Hinestroza AG, López-Moreno GA, Parra-Sepúlveda DJ. Atypical pityriasis rosea in a young Colombian woman. Case report. Case Reports. 2021;7(2):8-21.
Cómo citar
APA
ACM
ACS
ABNT
Chicago
Harvard
IEEE
MLA
Turabian
Vancouver
Descargar cita
Licencia

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
Los autores al someter sus manuscritos aceptan transferir a Case reports los derechos de autor de los artículos publicados. La editorial tiene el derecho del uso, reproducción, transmisión, distribución y publicación en cualquier forma o medio. Los autores no podrán permitir o autorizar el uso de la contribución sin el consentimiento escrito de la revista.
Formulario de Divulgación Uniforme para posibles Conflictos de Interés, los oficios de cesión de derechos y de responsabilidad deben ser entregadas junto con el original.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as conservarán sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cual estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación esta revista.
Los autores/as podrán adoptar otros acuerdos de licencia no exclusiva de distribución de la versión de la obra publicada (p. ej.: depositarla en un archivo telemático institucional o publicarla en un volumen monográfico) siempre que se indique la publicación inicial en esta revista.
Se permite y recomienda a los autores/as difundir su obra a través de Internet (p. ej.: en archivos telemáticos institucionales o en su página web) antes y durante el proceso de envío, lo cual puede producir intercambios interesantes y aumentar las citas de la obra publicada. (Véase El efecto del acceso abierto).