The coronavirus disease 2019 (COVID-19) pandemic has dramatically transformed the healthcare landscape around the world. In US medical education, students, residents, and fellows have experienced significant educational disruptions. Many trainees have been redeployed as frontline clinicians in regions with high COVID-19 case counts, experienced delays and interruptions in formal educational programs and licensing exams, and struggled with the psychological and emotional uncertainty of completing their education during a once-in-a-lifetime infectious pandemic.1 These disruptions have challenged traditional medical education structures to varying degrees at programs around the country, and have also spawned several novel innovations regarding the delivery of medical education and the practice of medicine. Radical curricular transformations, many of which have been received with enthusiasm, have occurred for fellows training in cardiovascular medicine in 2020 and 2021.
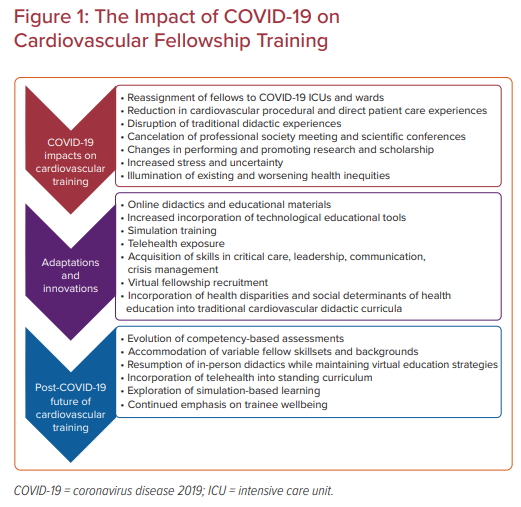
In this article, we describe the impact of the COVID-19 pandemic on education for cardiovascular fellows in training (FITs), provide an overview of the most common adaptations in medical education and care delivery that have occurred during this time, and highlight issues that cardiovascular training programs and FITs must navigate as the COVID-19 pandemic endures (Figure 1).
Impacts of COVID-19 on Cardiology Training
For US cardiovascular FITs, the demands and changes to healthcare delivery wrought by the COVID-19 pandemic have also upended their cardiovascular educations. Across the country, coinciding with temporal COVID-19 case surges, fellows have reported significant and prolonged interruptions to their training pathways.1–5 To accommodate the clinical care of patients with COVID-19 being admitted to academic medical centers, the Accreditation Council for Graduate Medical Education allowed institutions to self-declare Pandemic Emergency Status and reassign trainees from across all disciplines, including cardiovascular FITs, and restructure inpatient care teams to care for patients with COVID-19 as locally necessary.
Under this plan, cardiovascular FITs are allowed, if needed, to spend up to 20% of each academic year functioning as critical care fellows or internal medicine attending physicians, provided hospitals still maintain policies to ensure trainee safety, supervision, and work hour restrictions.6 FITs have therefore traded cardiovascular training opportunities for rotations in pulmonology, infectious disease, critical care medicine, and palliative care through reassignment to intensive care unit and hospitalist roles.7
Cardiovascular Procedural Volumes
Even in programs where redeployment of cardiovascular FITs was not necessary, social distancing mandates, personal protective equipment (PPE) conservation efforts, and anticipatory staffing changes resulted in many FITs being furloughed from their cardiovascular rotations, especially from in-person echocardiography, electrophysiology, and catheterization laboratory services. In a national survey of cardiovascular FITs, with almost 1,000 respondents from around the US, 88% of respondents reported decreased FIT staffing in their echocardiography laboratories and 90% reported decreased FIT staffing in their catheterization laboratories at the start of the pandemic.2
Additionally, many elective cardiovascular procedures and face-to-face clinic visits were canceled or rescheduled during the initial wave of the pandemic, to allow for staff redeployment, reduced COVID-19 exposure for patients and staff, and conservation of hospital resources.8,9 In a highly procedural specialty, such as cardiology, where competency is achieved through repeated practice, these changes significantly impacted the proficiency and confidence of FITs who graduated in 2020.
Senior fellows approaching graduation and sub-specialized fellows in interventional cardiology (IC) and electrophysiology were likely the most negatively affected by reductions in case volumes. Since these fellows work with increasing independence and mastery toward the end of their training, case cancelations or redeployment of fellows off of cardiac services entirely decreased the number of supervised cases these trainees were able to complete. In addition, for graduating fellows, there were no opportunities to recompense for missed training in subsequent years of fellowship. Currently, interventional cardiology fellows are required to perform 250 percutaneous interventions (PCIs) by the end of their year of training, as per the Fourth Core Cardiology Training Symposium (COCATS 4).10
In an early survey of 21 IC fellowship programs within the New York City metropolitan area, 95% of the responding IC fellows reported moderate (72%) or severe (24%) concern that the COVID-19 pandemic would have an adverse impact on their procedural training. Nearly 25% of IC fellows reported performing <250 PCIs by March 1, 2020, indicating concern that they would not achieve their COCATS 4 recommended PCI volume before the end of their IC fellowship year.3 Further, in a national survey of IC fellows and programs, only 43% of the responding 135 IC fellows reported performing >250 PCIs by March 2020, and 49% of IC fellows felt that their developing procedural skills were negatively impacted by the COVID-19 pandemic.10
Not unexpectedly, many fellows reported concerns that these reductions in case loads and direct care experiences would leave them underprepared for independent practice. In one study, 47% of surveyed IC FITs reported concerns that COVID-19-related alterations to their training programs would leave them less proficient independent operators by the end of training.10 This group of fellows also reported concerns about limited job opportunities after graduation, citing hiring freezes, inability to travel for in-person interviews, delayed employment start dates, and fewer available positions as other reasons for unstable postgraduation plans.10
In another study, fellows cited the cancellation of in-person national meetings and academic conferences, and the networking opportunities provided by these meetings as potential causes of fewer job prospects and advanced fellowship opportunities after graduation.2
Didactics and Academic Conferences
In addition to reductions in procedural case loads and exposure to patients, cardiovascular FITs also saw interruptions and changes to their protected didactic time. Based on the 2020 survey of US cardiovascular FITs, the vast majority of training programs canceled in-person didactic lectures entirely or transitioned their lecture series to online-only formats.2
All professional society conferences and academic meetings were similarly canceled or transitioned to an online-only format, leaving many without the opportunity to network in advance of their job searches or advanced training opportunities.11 Furthermore, many fellows also reported postponing planned learning of cardiovascular disease topics to stay up-to-date on the rapidly growing body of evidence in COVID-19 pathophysiology and treatments, hospital policies, and other COVID-19-associated topics.5,6
Trainee Wellbeing and Safety
These rapid and drastic changes to learning environments, reduced opportunities for the development of cardiovascular competencies, illumination of health inequities and systemic racism in medicine, and new and unfamiliar patient care roles have caused many FITs understandable mental strain and personal stress.12 In addition, fellows have reported concern for the health of their families and loved ones, financial stressors and uncertainty, social isolation, and disruptions in childcare.12,13 Finally, PPE rationing, ethical dilemmas regarding allocation of limited healthcare resources, repeated exposure to COVID-19-related morbidity and mortality, and overall concerns about personal health and COVID-19 exposures have all added to the emotional burdens of FITs during the past year.13,14
In a national survey of almost 1,000 cardiovascular FITs, 81% reported concern about personally contracting COVID-19, and 87% were worried about exposing their family or roommates to COVID-19. A total of 74% of FITs reported reusing N95 masks due to PPE rationing, and almost one-third of respondents reported difficulty obtaining PPE at their training institutions.2 While medical training is itself a time of potential stress for FITs, the changes created as a result of the COVID-19 pandemic ushered in unprecedented challenges to FITs’ physical and mental health.
Research and Scholarships
The COVID-19 pandemic also disrupted FITs’ participation in research, scholarly activities, and journal clubs and conferences.12 With the sudden and mandatory closures of non-essential operations, basic and translational research efforts were suspended, and clinical research operations, such as in-person clinical trial enrollment visits and follow-ups, have similarly suffered.12,13 More generally, social distancing mandates have limited mentorship opportunities for FITs pursuing research, and significantly reduced their options for presenting academic research and networking at conferences and academic meetings.1
Adaptations to Cardiology Training During COVID-19
Despite these disruptions, cardiovascular FITs, cardiovascular training programs, and national organizations have reaffirmed the importance of protecting trainees from COVID-19 exposure, and continuing to provide cardiovascular FITs with sufficient education in cardiovascular topics and core tenets.13,15 In line with these missions, a majority of programs pivoted their didactic programs and lecture series to online formats, and others embraced simulation training to continue procedural education. Most programs are providing training and exposure to telehealth care delivery, and some have advocated for a temporary relaxation of the COCATS 4 certification recommendations.
Online Education
To comply with social distancing guidelines, many cardiovascular training programs transitioned their in-person didactic series into online educational formats. A report from cardiovascular FITs at one academic center described their program-specific efforts to transition to online education, using a combination of Zoom (Zoom Video Communications) and Microsoft Teams (Microsoft Corporation) to provide lectures and educational activities for their fellows. They noted that the new online format promoted participation, and could potentially improve access to teaching for fellows who were at home on leave or otherwise not able to attend an in-person lecture.16
Other platforms, such as WebEx (Cisco Webex) and BlueJeans (BlueJeans Network), are also being frequently used at training centers around the country.6 Cardiovascular fellowship program directors at many programs established protocols for remote reading of cardiovascular imaging studies and other laboratory-based learning opportunities with a supervising physician via online platforms.12
The transition to online learning has had many benefits. Virtual lectures allow FITs at multiple training sites and multiple institutions to participate, and involve furloughed and quarantined fellows from home.6 These online platforms facilitate recording and asynchronous access to lectures, permitting FITs to learn on their own schedules or revisit lectures as desired.
Embedded tools, such as polling, screen sharing, and screen annotation, also foster a collaborative and engaging learning environment, with some reporting improved fellow participation in lectures since transitioning to an online format.12,17 In the national survey of almost 1,000 FITs, 73% reported enjoying virtual learning and voiced interest in continuing with online lectures after the resolution of the COVID-19 pandemic and social distancing mandates.2
Professional societies have also had to adapt to the COVID-19 pandemic, and many of them have offered free or cost-reduced online conferences and training materials to supplement FIT education. The virtual American College of Cardiology/World Congress of Cardiology Scientific Sessions in March 2020 provided an opportunity for >38,000 attendees from >157 different countries to participate and learn from the conference, which highlighted the success of online education as an opportunity to promote diversity and inclusion, especially for trainees who would not have been able to attend an in-person conference for logistical or financial reasons.7,18 In addition, the American College of Cardiology, the American Heart Association, the American Society of Nuclear Cardiology, and other cardiovascular professional societies have produced free training materials for FITs during the COVID-19 pandemic.19,20
Simulation-based Training
Simulation training is also being leveraged to continue procedural training in programs where case volumes have decreased or FITs are unable to achieve the recommended numbers of procedures. Task trainers in cardiac catheterization procedures and echocardiography, both transthoracic and transesophageal, are available and highly rated for both learner experience and also reduction in procedural complications, although they are expensive and not available at all institutions across the country.21,22
For those fellows that do have access, simulation trainers can be powerful tools to improve proficiency in technical skills in cardiology. The University of Texas Southwestern Medical Center recently detailed their success in using a simulation trainer to develop a training program for transthoracic echocardiography, noting that the program was successfully able to differentiate the skills of early FITs from experienced sonographers and allowed for easy and rapid feedback to trainees. This study concluded that simulation learning should be viewed as a powerful tool complementary to the traditional models of hands-on transthoracic echocardiography training.23 Some educators note that during the COVID-19 pandemic, simulation learning may be more useful for junior FITs who are still learning foundational procedural skills, as opposed to senior FITs who are hoping to refine their skills with the additional variables of patient-related differences, in-room distractions, PPE considerations, and other time pressures.13 In situations where live cases are limited, then, senior FITs could be assigned to in-person procedures and junior FITs to simulation sessions instead, so as to guarantee continued learning of fellows at different levels of competency.
Telehealth
With the conversion of much of ambulatory cardiology to telephone or video-based clinic visits, FITs have been able to hone their skills in the provision of remote care to patients.24 This transition has allowed FITs to continue their education in ambulatory cardiovascular medicine, but it also poses unique learning opportunities for FITs who must now also assess patient suitability for a telehealth, rather than in-person, visit. FITs must also conduct patient assessments without the aid of an in-person physical examination, and develop follow-up plans and testing recommendations while staying conscious of limited hospital resources.24
Supervising physicians are able to join FIT video conference or telephone call patient encounters to assess and provide feedback on FIT history gathering and communication skills immediately after a visit, an opportunity that is not as regularly available during normal in-person cardiovascular FIT clinics.6 Of note, prior to COVID-19, many fellowship programs did not provide formal telehealth training for their FITs, and so FITs’ experiences with and opinions of telehealth will likely be shaped by the amount of support or training they receive in this care modality moving forward.
Clinical Competency and Wellness
Although no formal changes have yet been made, to address concerns regarding clinical competency for graduating fellows, there have been some calls to temporarily relax the COCATS 4 procedural volume recommendations prior to graduation to account for the disruptions in training experienced by FITs across the country.4,13 Extensions in training duration, left to the discretion of program directors and clinical competency committees, have also been raised as a strategy to support graduating FITs who may not be prepared for independent practice by the expected graduation date.7 These changes would have potential domino effects on future employers, who might have to delay start times to allow fellows to complete additional months of training or provide extended periods of supervision at the start of new graduates’ practice to ensure that they are competent to practice independently.3
In addition to addressing issues regarding clinical competency, fellowship programs and their trainees have openly discussed increased efforts to promote FIT wellbeing. In a statement in the Journal of the American College of Cardiology, 10 cardiovascular fellowship program directors (PDs) from around the US called on all cardiovascular PDs to acknowledge the psychological stressors their FITs have encountered throughout the pandemic and to encourage FITs to prioritize self-care activities, including regular exercise, a regular sleep schedule, and dedicate time to loved ones and hobbies.12 In response, many programs have opened forums for FITs to express their concerns about redeployment, and communicate directly with program and hospital leadership. Other programs have offered hazard pay to redeployed fellows, provided financial support for childcare and mental health counseling, and have prioritized securing sufficient PPE and instruction in infection control for their FITs.1
To combat issues of social isolation and to allow for the rapid transmission of useful information, FITs have been encouraged to connect over social media platforms, such as Twitter and WhatsApp (Facebook).6 Virtual happy hours and office hours have been scheduled at many training programs.12 FITs also report regular virtual meetings with PDs to discuss trainee wellbeing, develop new support networks, and involve FITs in program decisions that will directly affect them, all of which help to cultivate a supportive work environment in the midst of a period of significant personal and institutional stress.12
Development of New Skills and Interests
Other potential benefits of curricular changes for cardiovascular FITs are the abilities to hone new skills, collaborate in multidisciplinary teams, and learn non-clinical competencies of leadership and crisis management within a healthcare environment.1 As noted in one report on cardiology training during the COVID-19 pandemic, FITs are also learning to practice medicine within resource-limited settings, and are relying on limited physical examination and point-of-care ultrasound skills to make diagnoses in situations where more advanced diagnostics would have previously been obtained.1 FITs are also learning about the cardiovascular impacts of COVID-19 infection and its therapies in real time as the evidence base surrounding its diagnosis, management, and prognosis rapidly evolves.25
Although these skills and topics were not included in pre-pandemic cardiovascular training curricula, FITs are now being offered opportunities to develop skills and knowledge that may prove essential in their future careers.7 The rapid generation of knowledge relating to COVID-19 has created plentiful opportunities for interested FITs to become involved in new research projects, including many studies investigating the short- and long-term cardiovascular impacts of COVID-19.
Virtual Fellowship Recruitment
Cardiovascular fellowship programs have rapidly adapted and innovated to continue training their current FITs, efforts to recruit future generations of cardiovascular FITs were also significantly revamped. In line with the Coalition for Physician Accountability’s Work Group on Medical Students in the Class of 2021 Moving Across Institutions for Post Graduate Training’s recommendation that all medical school and residency applications be conducted via online interviews and virtual visits, all US-based cardiology fellowship programs similarly transitioned to a fully online interview season.26,27
Programs and applicants alike adjusted to online interviews and virtual site visits. Anecdotal reports from PDs across the country in mid-2020 claimed that the number of applications to individual programs significantly increased for application year 2020 compared with prior years. These sentiments were ultimately corroborated by data released by the National Resident Matching Program which demonstrated that 1,575 individuals applied for 1,042 training slots in Cardiovascular Disease, a notable increase from the 1,395 applicants in 2020.
Programs and applicants faced new challenges, such as a higher volume of interviews over a shorter period of time, ensuring effective communication across electronic platforms, technological malfunctions, and, especially for applicants, limited understanding of a program’s physical location.28 However, for both interviewers and interviewees, an online-only format provided the benefits of avoiding unnecessary travel during the pandemic, decreased financial burden for applicants who otherwise would be responsible for travel and hotel costs, and fewer work days lost to travel.29 Enduring travel limitations may hinder newly-matched fellows who are unable to visit their new cities and secure housing ahead of matriculation.1
The Post-pandemic Future of Training in Cardiovascular Medicine
As much as cardiology training programs were faced with urgent decisions regarding how and when to alter their educational programs in the face of a novel and surging infectious disease pandemic, they will also lead the creation of new post-pandemic educational structures.
Core Cardiovascular Experiences
For procedural fellows, the reduction in COVID-19 cases locally has been accompanied by a resurgence of elective or less urgent cardiovascular procedures. Already, in regions that have experienced a reduced prevalence of patients with COVID-19, programs have managed relative resurgences in cardiac procedure volumes, as providers reschedule those cases that were previously delayed, provide care to those patients who delayed medical evaluation during prior COVID-19 surges, and also continue to provide care for patients who were already scheduled for routine care throughout 2020 and 2021.30 While fellows regain the ability to perform more cardiac procedures, if volume is far above normal capacity, providers should remain mindful of maintaining a balance of service and education for fellows.
Program directors should be alert to different learning needs for their incoming general cardiology fellows and new interests for their current FITs. First year fellows who matriculate into training programs from 2020 onward may have missed opportunities for cardiology electives or procedural experiences due to pandemic-related redeployments and changes to their residency educations. Additionally, cardiology programs may see an increased interest from cardiovascular FITs in additional training in critical care. While this additional exposure must be balanced against the issues of increased risk and proper access to PPE, for some FITs, this increased exposure to critical care concepts may spark interest in dedicated cardiac critical care training.5 Cardiac critical care was an emerging stand-alone field within cardiology before the start of the pandemic, and it would be not unexpected if this field’s popularity continues to rise as cardiovascular FITs return from their redeployments from COVID-19 wards with a newfound interest in critical care training opportunities.31
Remote Patient Care and Didactics
Similarly, for many FITs, the COVID-19 pandemic has provided novel opportunities for training and experience in telehealth. While reimbursement decisions will likely dictate the extent of telehealth’s continued use at the conclusion of the pandemic, the abilities to provide care to patients who live a long distance from hospitals and to closely monitor patients via remote monitoring devices may prove to be winning arguments for the continued support of telehealth clinics and focused training for FITs in telehealth skills and management.
Decisions about when and how to return to in-person lectures or in-person academic conferences should be led by local and national guidelines on social distancing and safe infection control practices. Prior to holding meetings in person, cardiology PDs could consider soliciting feedback from their FITs on the preferred methods of didactic delivery. Online lectures have thus far proven to be well-liked by trainees and have provided the additional benefits of allowing FITs at satellite hospitals or at home, on non-clinical rotations, or on parental or personal leave to participate in the didactic curriculum. Most likely, some combination of online and in-person lectures, or in-person lectures that are live-streamed online, will be embraced by most programs. Training program leaders should consider conducting formal assessments of the effectiveness of education in such hybrid models to inform future graduate medical education strategies. The remote learning resources produced and promoted by cardiovascular professional societies have proven to be popular methods of instruction for FITs around the country, and these initiatives should be supported for future trainees.
Simulation Learning
Simulation learning, although it has previously been touted as useful and effective, is, for many reasons, still inconsistently used, and its post-pandemic use will likely still be variable. Programs that have had access to simulation training models and incorporated them into their socially-distanced education plan may well choose to continue to use them, especially for junior fellows looking to develop and refine their foundational skills.
Conclusion
Whether any of the pandemic-associated changes to cardiology medical education are carried forward, FITs and educators have proven their willingness to adapt, quickly assimilate new technologies and learning platforms, and find new ways to maintain their own and their colleagues’ education during a time of significant upheaval, stress, and uncertainty.
There remains great opportunity for formal investigation into the effectiveness and durability of the novel educational strategies inspired by the COVID-19 pandemic. Cardiovascular medicine is a dynamic and innovative field, and both educators and trainees have aptly demonstrated their abilities to remain nimble in the face of crisis.
Clinical Perspective
- The cardiovascular education of current fellows in training was impacted greatly by cancellation of in-person didactics and conferences, re-deployment of trainees to front line non-cardiac services, and decreases in cardiovascular case volumes during the coronavirus 2019 pandemic.
- Cardiology training programs have quickly adapted their educational structures, with most now offering online lectures, simulation learning opportunities, training in telehealth medicine, and consideration of relaxed procedural requirements prior to fellowship graduation.
- Moving forward, programs will have to safely and effectively coordinate the transitions back to in-person formats, and maintaining hybrid educational formats, such as online lectures and other methods of remote and asynchronous instruction, should be considered.