Abstract
Background
Cardiovascular risk factors are associated with Alzheimer’s Disease (AD) development. However, few studies compare the overall cardiovascular risk with AD biomarkers, and when done, they are mainly performed in moderate cardiovascular risk regions.
Objectives
To determine whether cardiovascular risk in older adults is associated with pathological cerebrospinal fluid (CSF) biomarkers of AD in a low cardiovascular risk population.
Design
This is a cross-sectional study performed between 2017 and 2020.
Participants
The present work included patients between 50 and 75 years old who were negative for CSF AD biomarkers and had minimum cognitive alterations (controls) and patients with positive CSF AD biomarkers and in early stages of AD (cases).
Measurements
CSF biomarkers included total tau, phosphorylated tau 181 and amyloid β42 (Aβ42). Analytical variables were obtained. ERICE, SCORE2 and Framingham scales were used to calculate the overall patient’s cardiovascular risk. The Aβ42/Aβ40 ratio and neurofilaments were explored when available.
Results
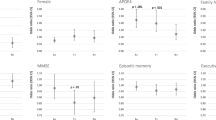
Two hundred and thirty-three patients were included. Nearly 76% of the sample had AD. AD patients had higher cardiovascular risk than controls (p-value < 0.05). ERICE and SCORE2 were associated with AD presence. Framingham was not. A correlation between elevated cardiovascular risk and higher total tau and NfL levels was observed when adjusted by age.
Conclusion
Cardiovascular risk assessment may be helpful in neurodegenerative disorders detection, as it is associated with CSF total tau and NfL. ERICE and SCORE2 may be useful scales in low cardiovascular risk regions to improve cardiovascular control and prevent neurodegenerative pathologies.




Similar content being viewed by others
Data Availability Statement: The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
References
Ribeiro VT, de Souza LC, Simões e Silva AC. Renin-Angiotensin System and Alzheimer’s Disease Pathophysiology: From the Potential Interactions to Therapeutic Perspectives. Protein Pept Lett. 2020;27(6):484–511. doi:https://doi.org/10.2174/0929866527666191230103739
Jack CR, Bennett DA, Blennow K, et al. NIA-AA Research Framework: Toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14(4):535–562. doi:https://doi.org/10.1016/J.JALZ.2018.02.018
Affleck AJ, Sachdev PS, Stevens J, Halliday GM. Antihypertensive medications ameliorate Alzheimer’s disease pathology by slowing its propagation. Alzheimer’s Dement (New York, N Y). 2020;6(1). doi:https://doi.org/10.1002/TRC2.12060
Dubois B, Feldman HH, Jacova C, et al. Advancing research diagnostic criteria for Alzheimer’s disease: the IWG-2 criteria. Lancet Neurol. 2014;13(6):614–629. doi:https://doi.org/10.1016/S1474-4422(14)70090-0
Blennow K, Zetterberg H. Biomarkers for Alzheimer’s disease: current status and prospects for the future. J Intern Med. 2018;284(6):643–663. doi:https://doi.org/10.1111/JOIM.12816
Arriagada J, Villalobos RÁ. Proteína tau como biomarcador en Alzheimer preclinico: Tau protein as a biomarker in preclinical Alzheimer’s disease. ARS MEDICA Rev Ciencias Médicas. 2022;47(2):56–67. doi:https://doi.org/10.11565/arsmed.v47i2.1892
Xiong YL, Meng T, Luo J, Zhang H. The Potential of Neurofilament Light as a Biomarker in Alzheimer’s Disease. Eur Neurol. 2021;84(1):6–15. doi:https://doi.org/10.1159/000513008
Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413–446.doi:https://doi.org/10.1016/S0140-6736(20)30367-6
Leszek J, Mikhaylenko E V, Belousov DM, et al. The Links between Cardiovascular Diseases and Alzheimer’s Disease. Curr Neuropharmacol. 2020;19(2):152–169. doi:https://doi.org/10.2174/1570159x18666200729093724
SCORE2-OP working group and ESC Cardiovascular risk collaboration, SCORE2-OP risk prediction algorithms: estimating incident cardiovascular event risk in older persons in four geographical risk regions, European Heart Journal, Volume 42, Issue 25, 1 July 2021, Pages 2455–2467, https://doi.org/10.1093/eurheartj/ehab312
Tini G, Scagliola R, Monacelli F, et al. Alzheimer’s Disease and Cardiovascular Disease: A Particular Association. Cardiol Res Pract. 2020;2020. doi:https://doi.org/10.1155/2020/2617970
D’Agostino RB, Vasan RS, Pencina MJ, et al. General Cardiovascular Risk Profile for Use in Primary Care. Circulation. 2008;117(6):743–753. doi:https://doi.org/10.1161/aRCULATIONAHA.107.699579
SCORE2 working group and ESC Cardiovascular risk collaboration, SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe, European Heart Journal, Volume 42, Issue 25, 1 July 2021, Pages 2439–2454, https://doi.org/10.1093/eurheartj/ehab309
Zhao YL, Ou YN, Ma YH, et al. Association between Life’s Simple 7 and cerebrospinal fluid biomarkers of Alzheimer’s disease pathology in cognitively intact adults: the CABLE study. Alzheimer’s Res Ther. 2022;14(1):1–9. doi:https://doi.org/10.1186/S13195-022-01019-2/FIGURES/3
Marrugat J, Vila J, Baena-Diez JM, et al. Relative Validity of the 10-Year Cardiovascular Risk Estimate in a Population Cohort of the REGICOR Study. Rev Espanola Cardiol (English Ed. 2011;64(5):385–394. doi:https://doi.org/10.1016/J.REC.2010.12.017
Gabriel R, Brotons C, Tormo MJ, et al. The ERICE-score: the new native cardiovascular score for the low-risk and aged Mediterranean population of Spain. Rev Esp Cardiol (Engl Ed). 2015;68(3):205–215. doi:https://doi.org/10.1016/J.REC.2014.03.019
Kaptoge S, Penneils L, De Bacquer D, et al. World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Heal. 2019;7(10):e1332. doi:https://doi.org/10.1016/S2214-109X(19)30318-3
Rabin JS, Schultz AP, Hedden T, et al. Interactive Associations of Vascular Risk and p-Amyloid Burden With Cognitive Decline in Clinically Normal Elderly Individuals: Findings From the Harvard Aging Brain Study. JAMA Neurol. 2018;75(9):1124. doi:https://doi.org/10.1001/JAMANEUROL.2018.1123
Song R, Xu H, Dintica CS, et al. Associations Between Cardiovascular Risk, Structural Brain Changes, and Cognitive Decline. J Am Coll Cardiol. 2020;75(20):2525–2534. doi:https://doi.org/10.1016/J.JACC.2020.03.053
Pettigrew C, Soldan A, Wang J, et al. Association of midlife vascular risk and AD biomarkers with subsequent cognitive decline. Neurology. 2020;95(23):e3093. doi:https://doi.org/10.1212/WNL.0000000000010946
Peña-Bautista C, López-Cuevas R, Cuevas A, Baquero M, Cháfer-Pericás C. Lipid peroxidation biomarkers correlation with medial temporal atrophy in early Alzheimer Disease. Neurochem Int. 2019;129:104519. doi:https://doi.org/10.1016/J.NEUINT.2019.104519
R-studio. Accessed December 21, 2022. https://posit.co/
Erdfelder E, FAul F, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. doi:https://doi.org/10.3758/BRM.41.4.1149/METRICS
Viticchi G, Falsetti L, Buratti L, et al. Framingham risk score can predict cognitive decline progression in Alzheimer’s disease. Neurobiol Aging. 2015;36(ll):2940–2945. doi:https://doi.org/10.1016/J.NEUROBIOLAGING.2015.07.023
Bangen KJ, Nation DA, Delano-Wood L, et al. Aggregate effects of vascular risk factors on cerebrovascular changes in autopsy-confirmed Alzheimer’s disease. Alzheimers Dement. 2015;11(4):394. doi:https://doi.org/10.1016/J.JALZ.2013.12.025
Sans S, Fitzgerald AP, Royo D, Conroy R, Graham I. Calibrating the SCORE Cardiovascular Risk Chart for Use in Spain. Rev Española Cardiol (English Ed. 2007;60(5):476–485. doi:https://doi.org/10.1016/S1885-5857(07)60188-1
Borràs C, Mercer A, Sirisi S, et al. HDL-like-Mediated Cell Cholesterol Trafficking in the Central Nervous System and Alzheimer’s Disease Pathogenesis. Int J Mol Sci. 2022;23(16). doi:https://doi.org/10.3390/IJMS23169356
Iwagami M, Qizilbash N, Gregson J, et al. Blood cholesterol and risk of dementia in more than 1–8 million people over two decades: a retrospective cohort study. Lancet Heal Longev. 2021;2(8):e498–e506. doi:https://doi.org/10.1016/S2666-7568(21)00150-1
Abdulrahman H, van Dalen JW, den Brok M, Latimer CS, Larson EB, Richard E. Hypertension and Alzheimer’s disease pathology at autopsy: A systematic review. Alzheimer’s Dement. Published online 2022. doi:https://doi.org/10.1002/ALZ.12707
García-Lluch G, Peña-Bautista C, Moreno Royo L, Baquero M, José Cañada-Martínez A, Chüfer-Pericüs C. Angiotensin II Receptor Blockers Reduce Tau/AB42 Ratio: A Cerebrospinal Fluid Biomarkers’ Case-Control Study. Pharm 2023, Vol 15, Page 924. 2023;15(3):924. doi:https://doi.org/10.3390/PHARMACEUTICS15030924
Gottesman RP, Schneider ALC, Zhou Y, et al. Association Between Midlife Vascular Risk Factors and Estimated Brain Amyloid Deposition. JAMA. 2017;317(14):1443–1450. doi:https://doi.org/10.1001/JAMA.2017.3090
Lo RY, Jagust WJ. Vascular burden and Alzheimer disease pathologic progression. Neurology. 2012;79(13):1349. doi:https://doi.org/10.1212/WNL.0B013E31826C1B9D
Barro C, Chitnis T, Weiner HL. Blood neurofilament light: a critical review of its application to neurologic disease. Ann Clin Transi Neurol. 2020;7(12):2508–2523. doi:https://doi.org/10.1002/ACN3.51234
Acknowledgments
CC-P acknowledges a postdoctoral “Miguel Servet” grant CPII21/00006 and a FIS PI19/00570 grant from the Health Institute Carlos III (Spanish Ministry of Economy, Industry and Innovation), and a predoctoral “PFIS” grant FI20/00022 from the Health Institute Carlos III. The authors are grateful to Cathedra DeCo Micof-UCH, to GINEA’s team and to all of the participants and caregivers of the study participants.
Funding
Funding: This research was funded by Cathedra DeCo Micof-UCH and by Instituto de Salud Carlos III through the project PI19/00570 (Co-funded by European Union, «A way to make Europe»). The Instituto de Salud Carlos III had no role in the design and conduct of the study; in the collection, analysis, and interpretation of data; in the preparation of the manuscript; or in the review or approval of the manuscript. All the manuscript was performed by members of the Cathedra DeCo Micof-UCH.
Author information
Authors and Affiliations
Contributions
Author Contributions: C.C-P, L.M, M.B and G.G-L designed this study. G.G-L drafted the manuscript. G.G-L, C.P-B and M.B contributed to data collection. J.P and G.G-L contributed to data analysis. C.C-P, L.M, M.B and G.G-L contributed to the interpretation of the data. C.C-P, L.M, J.P, M.B and G.G-L contributed to the final version of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest: The authors declare that they have no conflict of interest.
Additional information
How to cite this article: G. García-Lluch, J. Pardo, L. Moreno, et al. Cardiovascular Risk Scales Association with Cerebrospinal Fluid Alzheimer’s Disease Biomarkers in Cardiovascular Low Cardiovascular Risk Regions. J Prev Alz Dis 2024; https://doi.org/10.14283/jpad.2024.16
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
García-Lluch, G., Pardo Albiach, J., Moreno, L. et al. Cardiovascular Risk Scales Association with Cerebrospinal Fluid Alzheimer’s Disease Biomarkers in Cardiovascular Low Cardiovascular Risk Regions. J Prev Alzheimers Dis 11, 453–462 (2024). https://doi.org/10.14283/jpad.2024.16
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.14283/jpad.2024.16