Abstract
Background
Although studies have examined the geographic distribution of dementia among the general population in order to develop geographically targeted interventions, no studies have examined the geographic distribution of subjective cognitive decline (SCD) among military veterans specifically.
Objectives
To map the geographic distribution of subjective cognitive decline from 2011–2019 in the United States among military veterans.
Design
Cross-sectional.
Setting
United States.
Participants
Individuals reporting previous service in the United States Armed Forces.
Measurements
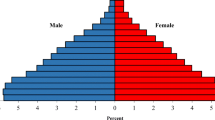
Using 2011 Behavioral Risk Factor Surveillance System (BRFSS) data, which is last year for which geocoded SCD data is publicly available, we estimated the survey-weighted county-level prevalence of veteran SCD for counties with >30 veterans (43 counties in 7 states). We then developed a Fay-Herriot small area estimation linear model using auxiliary data from the Census, with county-level veteran-specific covariates including % >65 years old, % female, % college educated, and median income. Following model validation, we created beta-weighted predictions of veteran SCD for all USA counties for 2011–2019 using relevant time-specific Census auxiliary data. We provide choropleth maps of our predictions.
Results
Results of our model on 43 counties showed that county-level rates of SCD were significantly associated with all auxiliary variables except annual income (F = 1.49, df = 4, 38). Direct survey-weighted rates were correlated with model-predicted rates in 43 counties (Pearson r = 0.32). Regarding predicted rates for the entire USA, the average county-level prevalence rate of veteran SCD in 2011 was 13.83% (SD = 7.35), but 29.13% in 2019 (SD = 14.71) — although variation in these rates were evident across counties.
Conclusions
SCD has increased since 2011 among veterans. Veterans Affairs hospitals should implement plans that include cognitive assessments, referral to resources, and monitoring patient progress, especially in rural areas.


Similar content being viewed by others
Availability of data and material: https://www.cdc.gov/brfss/annual_data/annual_2011.htm
Code availability: Not applicable.
References
Alzheimer’s Association. 2018 Alzheimer’s disease facts and figures. Alzheimer’s and Dementia. 2018;14:367–429 1. https://doi.org/10.1016/j.jalz.2018.02.001.
Crous-Bou M, Minguillón C, Gramunt N, et al. Alzheimer’s disease prevention: From risk factors to early intervention. Alzheimer’s Research and Therapy. 2017; 9:71 2. https://doi.org/10.1186/s13195-017-0297-z.
Alzheimer’s Association. 2021 Alzheimer’s disease facts and figures. Special report. Race, ethnicity and Alzheimer’s in America. Chicago, IL: Alzheimer’s Association. Retrieved 03/292021 from https://www.alz.org/media/Documents/alzheimers-facts-and-figures.pdf.
Rajan KB, Weuve J, Barnes LL, McAninch EA, Wilson RS, Evans DA. Population estimate of people with clinical AD and mild cognitive impairment in the United States (2020–2060). Alzheimer’s & Dementia. In press.
Alzheimer’s Association. Fact sheet. 2020. Retrieved 03/29/2021 from https://www.alz.org/media/Documents/subjective-cognitive-decline-in-us.pdf
Centers for Disease Control and Prevention. Subjective cognitive decline — a public health issue. 2019. Retrieved 03/29/2021 from https://www.cdc.gov/aging/agingdata/docs/subjective-cognitive-decline-508.pdf
Taylor CA, Bouldin ED, McGuire LC. Subjective cognitive decline among adults aged >45 years — United States, 2015–2016. Morbidity and Mortality Weekly Report. 2018;67(27):753–757 7. https://doi.org/10.15585/mmwr.mm6727a1.
Weiner MW, Friedl KE, Pacifico A, et al. Military risk factors for Alzheimer’s disease. Alzheimer’s and Dementia. 2013;9(4):445–451 8. https://doi.org/10.1016/j.jalz.2013.03.005.
Kirson NY, Meadows ES, Desai U, Smith BP, Cheung HC, Zuckerman P, Matthews BR. Temporal and geographic variation in the incidence of Alzheimer’s disease diagnosis in the US between 2007–2014. Journal of the American Geriatrics Society. 2019;68(2): 346–353 9. https://doi.org/10.1111/jgs.16262.
Fowler M, DiBlasio C, Crowe M, Kennedy RE. Geographic disparities in county-level prevalence of Alzheimer’s disease across the United States. Innovations in Aging. 2019;3(1):S782.
Centers for Disease Control and Prevention. BRFSS 2011 survey data and documentation. 2011. Retrieved 1/2/2021 from https://www.cdc.gov/brfss/annual_data/annual_2011.htm.
Fay RE, Herriot RA. Estimates of income for small places: An application of James-Stein procedures to census data. Journal of the American Statistical Association. 1979;74:269–277 12. https://doi.org/10.2307/2286322.
Li H, Lahiri P. An adjusted maximum likelihood method for solving small area estimation problems. J Multivariate Analysis. 2010;101(4):882–982 13. https://doi.org/10.1016/j.jmva.2009.10.009.
Parker JD, Talih M, Malec DJ, et al. National Center for Health Statistics data -presentation standards for proportions. National Center for Health Statistics. Vital Health Statistics. 2017;2(175):1–22 14. https://www.cdc.gov/nchs/data/series/sr_02/sr02_175.pdf.
United States Census Bureau. Advanced search. 2021. Retrieved 1/5/2021 from https://data.census.gov/cedsci/advanced.
Evans DA, Hebert LE, Beckett LA, Scherr PA, Albert MS, Chown MJ, Pilgrim DM, Taylor JO. Education and other measures of socioeconomic status and risk of incident Alzheimer disease in a defined population of older persons. Archives of Neurology. 1997;54:1399–1405. 16. https://doi.org/10.1001/archneur.1997.00550230066019
VanHoorhis CRW, Morgan BL. Understanding power and rules of thumb for determining sample sizes. Tutorials in Quantitative Methods for Psychology. 2017;3(2):43–50. 17. https://doi.org/10.20982/tqmp.03.2.p043
Zhang X, Holt JB, Yun S, Lu H, Greenlund KJ, Croft JB. Validation of multilevel regression and poststratification methodology for small area estimation of health indicators from the Behavioral Risk Factor Surveillance System. American Journal of Epidemiology. 2015;182(2):127–137. 18. https://doi.org/10.1093/aje/kwv002
Barnett JH, Lewis L, Blackwell AD, Taylor M. Early intervention in Alzheimer’s disease: A health economic study of the effects of diagnostic timing. BMC Neurology. 2014;14,101. 19. https://doi.org/10.1186/1471-2377-14-101
Lopez C, Caputo A, Liu F, Riviere ME, Rouzade-Dominguez ML, Thomas RG, Langbaum JB, Lenz R, Reiman EM, Graf A, Tariot PN. The Alzheimer’s prevention initiative generation program: Evaluating CNP520 efficacy in the prevention of Alzheimer’s disease. Journal of the Prevention of Alzheimer’s Disease. 2017;4(4):242–246. 20. https://doi.org/10.14283/jpad.2017.37
Norton S, Matthews FE, Barnes DE, Yaffe K, Brayne C. Potential for primary prevention of Alzheimer’s disease: An analysis of population based data. Lancet Neurology. 2014;13:788–794. 21. https://doi.org/10.1016/S1474-4422(14)70136-X
United States Department of Veterans Affairs. MOVE! Weight management program. 2021. Retrieved 3/9/2021 from https://www.move.va.gov/.
Haun JN, Paykel J, Alman AC, Patel N, Melillo C. A complementary and integrative health group-based program pilot demonstrates positive health outcomes with female veterans. EXPLORE. 2020;16(2):85–89. 23. https://doi.org/10.1016/j.explore.2019.08.001
Funding
Funding: No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest/Competing interests: The authors have no conflicts of interest to disclose.
Ethical standards: Because this study used de-identiied data freely available on the web, this study was considered exempt from IRB review.
Rights and permissions
About this article
Cite this article
McDaniel, J.T., McDermott, R.J. & Schneider, T. A Fay-Herriot Model for Estimating Subjective Cognitive Decline among Military Veterans. J Prev Alzheimers Dis 8, 457–461 (2021). https://doi.org/10.14283/jpad.2021.28
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.14283/jpad.2021.28