International Journal of Otorhinolaryngology
Download PDF
Research Article
*Address for Correspondence: Charles A Elmaraghy, MD, Department of Pediatric Otolaryngology, Nationwide Children’s Hospital, 700 Children’s Drive, Columbus, OH, USA, Tel: 614-722-6804; Fax: 614-722-6609; E-mail: charles.elmaraghy@nationwidechildrens.org
Citation: Elmaraghy CA, Mahida JB, Pluto CP, Minneci PC, Deans KJ, et al. The Utility of a Second CT Scan in the Management of Parapharyngeal and Retropharyngeal Abscesses in Pediatric Patients. Inter J Otorhinolaryngology. 2015;2(1): 7.
Copyright © 2015 Elmaraghy et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Otorhinolaryngology | ISSN: 2380-0569 | Volume: 2, Issue: 1
Submission: 12 February 2015 | Accepted: 27 March 2015 | Published: 01 April 2015
The Utility of a Second CT Scan in the Management of Parapharyngeal and Retropharyngeal Abscesses in Pediatric Patients
Charles A. Elmaraghy1*, Justin B Mahida2, CharlesP Pluto3, Peter C Minneci2, Katherine J Deans2, Nathan Cass4 and Andrew Tompkins2
- 1Department of Pediatric Otolaryngology, Nationwide Children’s Hospital, Columbus, OH, USA
2Center for Surgical Outcomes Research, Nationwide Children’s Hospital, Columbus, OH, USA
3Division of Radiology, Nationwide Children’s Hospital, Columbus, OH, USA
4Department of Otolaryngology, University of Colorado School of Medicine, Denver, USA
5Department of Otolaryngology, US Naval Services, Baltimore, USA
*Address for Correspondence: Charles A Elmaraghy, MD, Department of Pediatric Otolaryngology, Nationwide Children’s Hospital, 700 Children’s Drive, Columbus, OH, USA, Tel: 614-722-6804; Fax: 614-722-6609; E-mail: charles.elmaraghy@nationwidechildrens.org
Citation: Elmaraghy CA, Mahida JB, Pluto CP, Minneci PC, Deans KJ, et al. The Utility of a Second CT Scan in the Management of Parapharyngeal and Retropharyngeal Abscesses in Pediatric Patients. Inter J Otorhinolaryngology. 2015;2(1): 7.
Copyright © 2015 Elmaraghy et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Otorhinolaryngology | ISSN: 2380-0569 | Volume: 2, Issue: 1
Submission: 12 February 2015 | Accepted: 27 March 2015 | Published: 01 April 2015
Abstract
Objective: To evaluate the utility of follow-up CT imaging for predicting the need for surgical intervention in pediatric patients with deep neck infections (DNI) admitted for a trial of observation with medical management.Methods: Pediatric patients admitted with DNI from January 2000 to February 2009 who underwent a CT scan, initial medical management, and repeat CT scan were identified and separated into two cohorts: patients who underwent surgical intervention and patients treated with medical management. Necessity of surgical intervention following the repeat CT scan was determined and the predictive values of CT imaging characteristics and clinical characteristics for identifying necessary surgical interventions were calculated.
Results: 62 patients met inclusion criteria. Of the 32 patients who underwent surgical intervention following their second CT scan, 75% revealed an abscess. Of the 30 patients who continued with medical management following the second CT scan, 10% failed medical management. The combination of increased size, increased peripheral enhancement, and walling off of collections on subsequent CT imaging yielded 83% specificity for identifying patients who needed surgical intervention. Interpretation of the collection as a phlegmon or abscess on the repeat CT scan by the radiologist yielded 96% sensitivity for identifying patients who needed surgical intervention.
Conclusion: Follow-up CT imaging can assist with determining the need for surgical intervention in children with deep neck infections initially managed medically.
Charts were reviewed for the following variables: age at presentation, sex, anatomic location of infection (RP or PP) as documented by the evaluating otolaryngology attending physician and using billing data when this was not clearly documented, duration of symptoms prior to presentation, symptoms described on presentation, presenting white blood cell (WBC) count, antibiotic treatment given, number of days between CT scans, positive symptoms immediately preceding second CT scan, whether the patient was taken to the operating room, and, if so, whether pus was obtained at surgery. Patients who continued on medical treatment after follow-up CT scan but who ultimately underwent surgery for worsening clinical condition were identified as medical treatment failures.
Considering the benefits of repeat CT imaging in evaluating patients with DNI, we considered the optimal time for CT imaging. Waiting a longer time before obtaining the follow-up CT scan was suggestive of a difference in whether or not an abscess was found at surgery. This is consistent with clinical expectations; by allowing more time for the infection to define itself, the ability of the CT scan to detect clinically significant increases in size or peripheral enhancement grows.
Keywords
Deep neck infection; Retropharyngeal abscess; Parapharyngeal abscess; Surgery; Computed tomography; Antibiotic resistanceIntroduction
Retropharyngeal (RP) and parapharyngeal (PP) infections are the most common deep neck infections (DNI) treated in children. Unless airway compromise or signs of instability are present, current treatment recommendations include diagnostic imaging, hospital admission with empiric IV antibiotics, and clinical monitoring of progress for 24-72 h before considering surgery [1].CT scan is currently the imaging study of choice for initial evaluation of pediatric DNIs [1-4]. CT imaging is often obtained upon presentation to confirm presence of infection, to determine its stage on the spectrum between cellulitis and abscess, and to provide the surgeon with anatomic guidance in order to plan for surgery. For those patients in whom clinical response to antibiotics remains uncertain after a trial period of medical management, CT imaging may also be employed to assess for progression of the infectious process.
Multiple studies have evaluated the utility of CT imaging for the initial evaluation of pediatric DNIs [3,5,6]. However, no study to date has analyzed the utility of follow-up CT imaging for pediatric DNIs. The purpose of this study was to determine the utility of repeat CT imaging in pediatric patients with DNIs for predicting the need for surgical intervention following a trial of medical management.
Materials and Methods
After securing institutional review board approval, a retrospective review was performed of the medical records of pediatric (age<18 years) patients with RP or PP infections discharged between January 2000 and February 2009 from a large pediatric hospital. Patients with International Classification of Disease 9 (ICD-9) diagnosis codes 478.22 (PP abscess) and 478.24 (RP abscess) were included. The charts of patients discharged with any of the other ICD-9 diagnosis codes listed in Table 1 were reviewed, and patients with either RP or PP infections as documented by an otolaryngology attending physician were included. Patients who received at least two CT scans during their hospital stay for which imaging was available for review were included in the study.Charts were reviewed for the following variables: age at presentation, sex, anatomic location of infection (RP or PP) as documented by the evaluating otolaryngology attending physician and using billing data when this was not clearly documented, duration of symptoms prior to presentation, symptoms described on presentation, presenting white blood cell (WBC) count, antibiotic treatment given, number of days between CT scans, positive symptoms immediately preceding second CT scan, whether the patient was taken to the operating room, and, if so, whether pus was obtained at surgery. Patients who continued on medical treatment after follow-up CT scan but who ultimately underwent surgery for worsening clinical condition were identified as medical treatment failures.
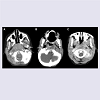
Blinded review of the initial and follow-up CT scans was performed by two independent pediatric radiology fellows who then reached agreement in measurements and coding by reviewing the images together. Volume was calculated based on measurement of axial major and minor axis lengths to 1 mm and cranio-caudal length to 2.5 mm; these volumes were then used to determine if the lesion had increased in size. Peripheral enhancement was compared between initial and follow-up CT scans for each patient and judged to be either increased or not increased. The second CT was evaluated for presence of wall thickening of the lesion. The radiologists also categorized their interpretation of each CT into one of four categories: no pathologic findings, edema or developing phlegmon, phlegmon or developing abscess, and abscess (Figure 1). Progression was defined as a change from one category to a more advanced category on the second CT.Comparisons were made between the population who went to the operating room and those who did not, and also between patients who needed surgery and those who did not. Needing surgery was defined as those patients who underwent surgery and revealed purulent drainage and those patients who did not initially undergo surgery but then presented as medical treatment failures [6-9]. Not needing surgery was defined as those patients who underwent surgery but did not reveal purulent drainage and those patients who underwent medical treatment with resolution of their DNI. To examine the effect of the time interval between the initial and repeat CT scan, we divided patients into groups undergoing repeat imaging within 2.5 days compared to longer than 2.5 days. Leukocytosis was defined as WBC >14,000/mm3 for under 2 years, >12,000/mm3 for 2-9 years, and >10,500/mm3 for over 10 years [10]. Continuous variables were compared using t-tests with 95% confidence intervals, and categorical variables were compared using Fisher’s exact tests.
Figure 1: Examples of diagnostic labels used by radiology for categorizing each lesion. White arrowheads point to the pathologic finding on each CT image. Panel A demonstrates an example of focal edema without mass effect and with preservation of the fascial planes, and was categorized as edema or a developing phlegmon. Panel B demonstrates an example of a partial peripherally enhancing phlegmon with regional inflammatory fatty infiltration and partial obscuration of the adjacent fascial planes and was categorized as a phlegmon or developing abscess. Panel C demonstrates an example of a completely circumscribed, thick walled, peripherally enhancing abscess with central necrosis, mass effect and obliteration of the regional fascial planes, and was categorized as an abscess.
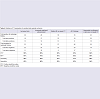
Sensitivities and specificities for predicting a need for surgery were calculated for five different radiologic profiles of follow-up CT scans: increased size, increased peripheral enhancement, presence of wall thickening of the lesion on repeat CT, evidence of all three of these findings, and characterization of the lesion as a phlegmon or abscess by the radiologist on repeat imaging. Sensitivity was calculated as those patients with positive CT findings who needed surgical intervention as a fraction of the combination of patients with the positive CT findings who needed surgery and those with negative CT findings who needed surgery. Specificity was calculated as those patients with negative CT findings who did not need surgery as a fraction of the combination of patients with negative CT findings who did not need surgery and those with positive CT findings who did not need surgery.
Results
During the study period, 276 children were treated for DNI with 162 having an RP abscess, 104 having a PP abscess, and 10 having both types of abscesses. Of these patients, 35 underwent immediate operation, 50 were discharged without observation, and 191 were admitted for observation and trial medical management (Figure 2). At the end of trial observation, 29 patients underwent surgery and 78 patients were discharged without repeat imaging prior to discharge. Of the remaining 84 patients, 62 patients met inclusion criteria and were included in this study (Figure 2); 32 of these patients underwent surgery prior to discharge in addition to receiving IV antibiotics, and 30 patients were treated with IV antibiotics alone (Table 2), of whom 3 (10%) were re-admitted for surgery yielding purulent drainage.Compared to patients who did not undergo surgery, the second CT scan in patients undergoing surgery more frequently demonstrated increased peripheral enhancement of the collection (63% vs. 30%, p= 0.008), discrete wall thickening on the second CT (75% vs. 37%, p=0.002), progression (59% vs. 30%, p=0.014), and categorization of the lesion as a phlegmon or abscess on both the first (63% vs. 37%, p=0.027) and second CT (88% vs. 47%, p<0.001). There were no significant differences in the antibiotic regiments; of the patients who neither received clindamycin nor Unasyn, one patient received vancomycin and piperacillin-tazobactam and the other received linezolid and meropenem.Table 3 compares features of those patients in whom purulent drainage was encountered at surgery (n=27) to those who did not need surgery (n=35), either because they successfully completed medical treatment or because they did not reveal purulent drainage intraoperatively. Variables significantly associated with needing surgery were walling off of the lesion on the second CT (81% vs. 37%, p<0.001), presence of a phlegmon or abscess on the second (96% vs. 68%, p<0.001) and the first CT scan (70% vs. 34%, p=0.004), waiting ≥2.5 days between CT scans (59% vs. 26%, p=0.006), increased peripheral enhancement (63% vs. 34%, p=0.017), progression (59% vs. 34%, p=0.031), and increased size (59% vs. 37%, p=0.047).
Table 4 notes sensitivity and specificity for various radiologic findings and their ability to predict the need for surgery in all patients. Presence of a phlegmon or abscess on the second CT as determined by a radiologist is associated with 96% sensitivity but only 54% specificity. The combination of increased size, increased peripheral enhancement, and walling off of the lesion, while only 37% sensitive, is 83% specific for needing surgery, as is expected for criteria in which multiple radiologic findings are evaluated instead of just one.
Discussion
Accurate determination of the need for surgical intervention in patients with DNI being managed medically could greatly improve care. Our results demonstrate that preoperative information from repeat CT imaging are more predictive in identifying patients who should undergo surgery following unclear outcomes from a trial of medical management than clinical information alone. Our study population does not include those patients for whom the decision to operate or to discharge was made on initial evaluation, nor does it include those patients for whom the decision to operate or to discharge following trial management with IV antibiotics and observation was made without repeat imaging. Instead, focusing on those remaining patients for whom the need to operate is still unclear, identification of the DNI as a phlegmon or abscess on repeat CT imaging is associated with excellent sensitivity for identifying patients who will require surgery. Additional CT findings that are conventionally used by otolaryngologists to evaluate DNIs, such as increased size, increased peripheral enhancement, and walling off of the lesion, demonstrate reasonable specificity for determining which patients should undergo surgery.Although antibiotic therapy has been a contributor to the decreased morbidity and mortality seen in pediatric DNIs in the last half-century, it does not preclude the need for surgery. Widespread use of antibiotics has allowed for a shift in practice from operative management for all suspected abscesses to use of initial medical management in treating DNI. Some trials have demonstrated a limited ability to resolve abscesses with antibiotics alone [2,7,9,11-13], especially in older children [1]. A larger study of empiric antibiotic trials showed 75% resolution without surgery, with no subjects having adverse outcomes (death, major complications, or recurrence), leading the authors to recommend a trial of initial IV antibiotic therapy for all stable patients with DNIs [15]. At the same time, surgical management is still clinically relevant. In our data set, we note three children who underwent and failed medical management. If children with radiologically evident DNIs are increasingly managed medically, the number of patients in whom the treatment course is unclear after 48 h will likely increase; it is in this group of patients that repeat CT imaging characteristics may provide valuable information assist with clinical decision making.
The clinical acumen of the otolaryngologist is important in observing these patients and determining whether to operate. However, our analysis did not identify clinical patterns significantly associated with patients needing surgery. As noted in Table 2 and Table 3, use of clinical factors as an alternative to repeat CT imaging is not predictive of the need for surgery or presence of an abscess at surgery. Previous studies have noted correlation between the duration of fever prior to presentation and the need for surgical drainage in only PP infections [16]. However, our lack of clinical predictors matches findings of other studies: Elden et al. found that initial WBC count and temperature was not helpful in differentiating abscess versus cellulitis [4], and Wong et al found that no symptoms or signs reliably help distinguish which children will yield purulent material at surgery [12]. In light of this, our identification of predictive findings on CT scans may be helpful in determining the need for operative intervention.
Other imaging modalities are available but have not demonstrated similar utility to CT imaging. Ultrasound is valuable for screening on initial presentation, but demonstrates a limited ability to define deep neck spaces [17]. Previous studies demonstrate that CT imaging upon presentation is helpful in delineating between cellulitis and abscess and for guiding initial management in the treatment of pediatric DNIs [2-4,6,8,13]. Some findings on initial CT, such as diameter of abscess above 2 cm and presence of peripheral enhancement, correlate with a higher likelihood of failing medical management [18,19]. Furthermore, CT imaging is useful for other reasons besides determining the need for surgery, as it also provides anatomic guidance to the surgeon during surgery.
Even though diagnostic CTs are considered to be in the low-level radiation range (under 100 mSv) [20], radiation from medical exams is a particularly important issue in children because they are up to ten times more susceptible to the ionization secondary to their smaller mass and longer lifetime [21]. This is especially true of the thyroid gland [22] Radiation from a single pediatric neck CT is estimated to be in the range of 2-6 mSv [23,24], as compared to the average annual background radiation exposure at sea level, which is estimated to be 3mSv. At these doses, the increased risk of developing thyroid cancer has been estimated at up to 390 per million children [25]. MRI provides an alternative, non-ionizing form of imaging the head and neck and is becoming more popular for imaging DNIs [26]. However, MRI is more expensive and young patients may require sedation.
Considering the benefits of repeat CT imaging in evaluating patients with DNI, we considered the optimal time for CT imaging. Waiting a longer time before obtaining the follow-up CT scan was suggestive of a difference in whether or not an abscess was found at surgery. This is consistent with clinical expectations; by allowing more time for the infection to define itself, the ability of the CT scan to detect clinically significant increases in size or peripheral enhancement grows.
Existing literature already demonstrates the value of CT imaging in identifying patients with DNIs who do not need to undergo surgery on initial presentation. This study adds to the existing literature by supporting repeat use of CT imaging in patients who have undergone an initial trial of inpatient medical management and did not have rapid resolution of symptoms. It suggests that radiologist interpretation of a phlegmon or abscess is highly sensitive for identifying patients who need surgical intervention. This study also supports the use of other common CT findings such as increased size, increased peripheral enhancement, and walling off of the lesion that are useful for further characterizing patients who need surgery.
Limitations of the study include its format as a retrospective case control at a single institution over a nine year period. Over this time period, we did not observe any clinical changes in the management of patients with deep neck infections. Also, clinical characteristics of our DNI patient population are consistent with those of other studies. The percentage of RP versus PP abscesses in this study (71% vs.26%) and in the 306 total cases of DNI presenting at our institution over this time period (59% versus 41%) are similar to previously reported proportions of 50-85% RP and 11-44% PP [4,6,9]. In addition, only associations can be reported, as each decision to proceed to surgery was made using both clinical and radiologic data. Also, reviewing charts for the symptoms the clinician believes are pertinent and has decided to report, instead of asking specific questions about whether or not each symptom is present, introduces inconsistency into the data. Additionally, we defined those patients who underwent surgery but did not reveal purulent drainage as patients who did not need surgery; this is not a perfect identifier of those patients who needed surgery, but is consistent with prior studies of DNI [6-9].
Conclusion
Patients with DNI for whom the best treatment approach is unclear even after CT imaging on presentation will frequently undergo an initial trial of medical management and observation. This study suggests that patients who do not demonstrate a phlegmon or abscess on repeat imaging should not undergo surgery. Future endeavors could include comparing CT with MRI for predicting surgical necessity.Acknowledgements
The authors would like to thank Andrew Tompkins, MD, for his work in data collection.Funding support: This project is supported by intramural funding from the Department of Otolaryngology and the Center for Surgical Outcomes Research at Nationwide Children’s Hospital.
References
- Jaryszak E, Choi S (2012) Deep Neck Space Infections, in Schoem SR and Darrow DH (eds): Pediatric Otolaryngology. Elk Grove Village, IL, Am Acad Pediatr, pp. 272-299.
- Nagy M, Backstrom J (1999) Comparison of the sensitivity of lateral neck radiographs and computed tomography scanning in pediatric deep‐neck infections. Laryngoscope 109: 775-779.
- Stone ME, Walner DL, Koch BL, Egelhoff JC, Myer CM (1999) Correlation between computed tomography and surgical findings in retropharyngeal inflammatory processes in children. Int J Pediatr Otorhinolaryngol 49: 121-125.
- Elden LM, Grundfast KM, Vezina G (2001) Accuracy and usefulness of radiographic assessment of cervical neck infections in children. J Otolaryngol 30: 82-89.
- Fédérici S, Silva C, Maréchal C, Laporte E, Sévely A, et al. (2009) Retro- and parapharyngeal infections: standardization of their management. Arch Pediatr 16: 1225-1232.
- Vural C, Gungor A, Comerci S (2003) Accuracy of computerized tomography in deep neck infections in the pediatric population. Am J Otolaryngol 24: 143-148.
- Nagy M, Pizzuto M, Backstrom J, Brodsky L (1997) Deep neck infections in children: a new approach to diagnosis and treatment. Laryngoscope 107: 1627-1634.
- Boucher C, Dorion D, Fisch C (1999) Retropharyngeal abscesses: a clinical and radiologic correlation. J Otolaryngol 28: 134-137.
- Daya H, Lo S, Papsin BC, Zachariasova A, Murray H, et al. (2005) Retropharyngeal and parapharyngeal infections in children: the Toronto experience. Int J Pediatr Otorhinolaryngol 69: 81-86.
- Kliegman R, Nelson WE (2011) Nelson textbook of pediatrics. Philadelphia, PA, Elsevier/Saunders.
- McClay JE, Murray AD, Booth T (2003) Intravenous antibiotic therapy for deep neck abscesses defined by computed tomography. Arch Otolaryngol Head Neck Surg 129: 1207-1212.
- Wong DK, Brown C, Mills N, Spielmann P, Neeff M (2012) To drain or not to drain - management of pediatric deep neck abscesses: a case-control study. Int J Pediatr Otorhinolaryngol 76: 1810-1813.
- Craig FW, Schunk JE (2003) Retropharyngeal abscess in children: clinical presentation, utility of imaging, and current management. Pediatrics 111: 1394-1398.
- Bolton M, Wang W, Hahn A, Ramilo O, Mejias A, et al. (2013) Predictors for successful treatment of pediatric deep neck infections using antimicrobials alone. Pediatr Infect Dis J 32: 1034-1036.
- Al-Sabah B, Bin Salleen H, Hagr A, Choi-Rosen J, Manoukian JJ, et al. (2004) Retropharyngeal abscess in children: 10-year study. J Otolaryngol 33: 352-355.
- Page C, Biet A, Zaatar R, Strunski V (2008) Parapharyngeal abscess: diagnosis and treatment. Eur Arch Otorhinolaryngol 265: 681-686.
- Maroldi R, Farina D, Ravanelli M, Lombardi D, Nicolai P (2012) Emergency imaging assessment of deep neck space infections. Semin Ultrasound CT MR 33: 432-442.
- Hoffmann C, Pierrot S, Contencin P, Morisseau-Durand MP, Manach Y, et al. (2011) Retropharyngeal infections in children. Treatment strategies and outcomes. Int J Pediatr Otorhinolaryngol 75: 1099-1103.
- Cheng J, Elden L (2013) Children with deep space neck infections: our experience with 178 children. Otolaryngol Head Neck Surg 148: 1037-1042.
- Strom DJ, Cameron JR (2002) Is it useful to assess annual effective doses that are less than 100 mSv? Radiat Prot Dosimetry 98: 239-245.
- (2007) The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Annals of the ICRP 37: 1-332.
- Stone R (2001) Living in the Shadow of Chernobyl. Science 292: 420-426.
- Huda W, Atherton JV, Ware DE, Cumming WA (1997) An approach for the estimation of effective radiation dose at CT in pediatric patients. Radiology 203: 417-422.
- Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, et al. (2009) Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Int Med 169: 2078-2086.
- Mazonakis M, Tzedakis A, Damilakis J, Gourtsoyiannis N (2007) Thyroid dose from common head and neck CT examinations in children: is there an excess risk for thyroid cancer induction? Eur Radiol 17: 1352-1357.
- Wang B, Gao BL, Xu GP, Xiang C (2013) Images of deep neck space infection and the clinical significance. Acta Radiol 55: 945-951.