Periprosthetic fractures due to a fall may occur even with plate installation reinforcement. From a mechanical perspective, with a total hip arthroplasty (THA) or hip bipolar hemiarthroplasty (BHA) stem inserted, a fall could result in a subtrochanteric fracture.
Dr. Hiroto Taniguchi, Department of Orthopaedic Surgery, Yachiyo Medical Center, Tokyo Women’s Medical University, Chiba, Japan. E-mail: hiroto.taniguchi@dream.com
Introduction: In an aging society, the incidence of periprosthetic fractures will increase owing to the increasing number of patients undergoing joint replacement surgery. We experienced a case of recurrent periprosthetic fracture in a patient who had undergone ipsilateral hip bipolar hemiarthroplasty (BHA) and total knee arthroplasty. Based on our experience, we discuss the treatment strategy for periprosthetic fractures in patients at a high risk of fall.
Case Report: An 84-year-old woman, who had undergone total knee arthroplasty 9 years ago and ipsilateral hip BHA 2 years ago, sustained a knee condylar fracture (Su classification type III) due to fall. This knee periprosthetic fracture posed a challenge for osteosynthesis; therefore, revision total knee arthroplasty was performed using a hinge-type prosthesis. During this surgery, we installed a reinforcement plate on the femoral shaft to prevent fractures because of the short stem tip distance between the hip and knee prosthesis (53 mm). The procedure was successful, and the patient regained her walking ability. However, 6 months after surgery, the patient sustained a hip periprosthetic fracture (Vancouver type B2) due to a fall, despite precautionary plate installation. In case of hip stem insertion, the stress caused by fall is concentrated on the infratrochanteric region, as reflected in her fracture site. From a mechanical perspective, this fracture was not accidental. The plate reinforcement procedure may have been inadequate because the top of the plate was located at the infratrochanteric region.
Conclusion: Periprosthetic fractures may occur despite the installation of a plate for fracture prevention. With a total hip arthroplasty or hip BHA stem inserted, a fall could result in a subtrochanteric fracture.
Keywords: Periprosthetic fracture, interprosthetic fracture, plate reinforcement, stress concentration.
Owing to the progressive population aging, the number of patients receiving treatment for knee osteoarthritis has been increasing. Consequently, the number of patients undergoing total hip arthroplasty (THA) and total knee arthroplasty (TKA) has been steadily increasing. As elderly individuals are vulnerable to falls, the incidence of injuries related to periprosthetic fractures has increased [1, 2, 3]. In a study, patients who had undergone THA or TKA showed a 30% higher risk of sustaining fractures in the same leg, with an associated mortality rate of 31%, and particularly, in interprosthetic fractures occurring between artificial joints, the reported postoperative life expectancy of patients is 3.45 years [1]. Therefore, preventing interprosthetic fractures is important. We experienced a case of recurrent periprosthetic fracture in a patient who had undergone hip bipolar hemiarthroplasty (BHA) and TKA for the ipsilateral femur. Based on this case, we discussed the treatment strategy for periprosthetic fractures in patients at a high risk of falls.
An elderly woman had diabetes mellitus and elderly-onset rheumatoid arthritis (onset at the age of 72 years). The patient had bilateral knee osteoarthritis (Grade 3 of the Kellgren–Lawrence classification) since her 60s, that is, before the onset of rheumatoid arthritis. The patient underwent TKA of her right knee at the age of 75 years at our hospital (Fig. 1a and b); left knee TKA was performed in the following year. The patient had been living independently since the bilateral TKA surgeries; however, 7 years after her right knee TKA, she sustained a Garden IV right femoral neck fracture due to a fall. The patient underwent BHA on her right hip joint (Fig. 1c and d). Postoperatively, she regained the ability to walk and could live independently at home. However, at the age of 84 years, that is, 9 years after the right TKA (2 years after BHA), the patient again suffered a fracture due to a fall. On this occasion, it was a periprosthetic fracture of TKA. It was a right femoral condylar fracture (Type III of the Su classification, Fig. 2) [4].
The patient had been living independently since the bilateral TKA surgeries; however, 7 years after her right knee TKA, she sustained a Garden IV right femoral neck fracture due to a fall. The patient underwent BHA on her right hip joint (Fig. 1c and d). Postoperatively, she regained the ability to walk and could live independently at home. However, at the age of 84 years, that is, 9 years after the right TKA (2 years after BHA), the patient again suffered a fracture due to a fall. On this occasion, it was a periprosthetic fracture of TKA. It was a right femoral condylar fracture (Type III of the Su classification, Fig. 2) [4].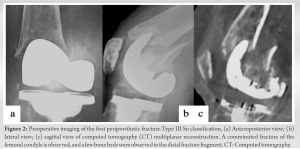 This was not only a knee periprosthetic fracture but also an interprosthetic fracture. In this case, the possibility of osteosynthesis was quite bleak because computed tomography (CT) analysis showed almost no remnant bone tissue in the distal bone fragments (Fig. 2c). Therefore, we planned a revision TKA surgery with a hinge-type prosthesis. However, a BHA stem was already installed in the proximal femur; therefore, the implantation of a hinged prosthesis stem would have increased the stress on the femoral diaphysis between the stem tips. According to the protocol described elsewhere [1, 5, 6, 7], we installed a locking compression plate (LCP) to prevent interprosthetic fractures. The length of the plate was designed to ensure the overlap of the BHA stem by a certain distance [8]. We used more monocortical screws for plate fixation to stabilize the plate on the surface of the bone. Therefore, only one cerclage positioning pin and one metal cable were installed; and, several 5-mm ultra-high-molecular-weight polyethylene cables (Nesplon cable®) were used to bind the LCP to the diaphysis (Fig. 3).
This was not only a knee periprosthetic fracture but also an interprosthetic fracture. In this case, the possibility of osteosynthesis was quite bleak because computed tomography (CT) analysis showed almost no remnant bone tissue in the distal bone fragments (Fig. 2c). Therefore, we planned a revision TKA surgery with a hinge-type prosthesis. However, a BHA stem was already installed in the proximal femur; therefore, the implantation of a hinged prosthesis stem would have increased the stress on the femoral diaphysis between the stem tips. According to the protocol described elsewhere [1, 5, 6, 7], we installed a locking compression plate (LCP) to prevent interprosthetic fractures. The length of the plate was designed to ensure the overlap of the BHA stem by a certain distance [8]. We used more monocortical screws for plate fixation to stabilize the plate on the surface of the bone. Therefore, only one cerclage positioning pin and one metal cable were installed; and, several 5-mm ultra-high-molecular-weight polyethylene cables (Nesplon cable®) were used to bind the LCP to the diaphysis (Fig. 3). 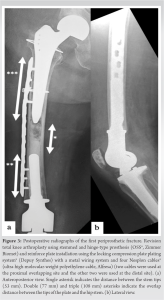 The rehabilitation period was uneventful, and the patient was discharged 12 weeks after surgery after rehabilitation at a rehabilitation specialty hospital. After discharge, the patient lived an independent life. However, at the age of 85 years, that is, 6 months after returning to her home life, the patient again sustained a fracture due to a fall at home. It was an infratrochanteric fracture of her right femur (Vancouver type B2) [9], which occurred near the upper edge of the previously installed preventive plate (Fig. 4).
The rehabilitation period was uneventful, and the patient was discharged 12 weeks after surgery after rehabilitation at a rehabilitation specialty hospital. After discharge, the patient lived an independent life. However, at the age of 85 years, that is, 6 months after returning to her home life, the patient again sustained a fracture due to a fall at home. It was an infratrochanteric fracture of her right femur (Vancouver type B2) [9], which occurred near the upper edge of the previously installed preventive plate (Fig. 4).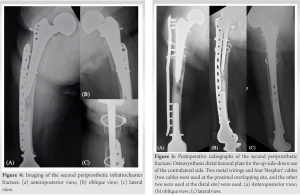 Owing to her old age, we considered total femoral replacement to be highly invasive and opted for osteosynthesis. Intraoperative findings showed that the BHA Zweymuller-type stem was stable after fracture reduction and was preserved; therefore, we could complete osteosynthesis. We installed an up-side-down plate using a left-side distal femur fixation LCP for the right proximal femur. As a previous surgery, we used several polyethylene and metal cables to bind the plate and diaphysis. The range of plate fixation was extended from the infratrochanter to the greater trochanter (Fig. 5). The patient could get out of bed 3 weeks after this surgery; however, she did not adequately recover her walking ability and was confined to a wheelchair. The patient was not discharged to home and ended up living in a medical facility.
Owing to her old age, we considered total femoral replacement to be highly invasive and opted for osteosynthesis. Intraoperative findings showed that the BHA Zweymuller-type stem was stable after fracture reduction and was preserved; therefore, we could complete osteosynthesis. We installed an up-side-down plate using a left-side distal femur fixation LCP for the right proximal femur. As a previous surgery, we used several polyethylene and metal cables to bind the plate and diaphysis. The range of plate fixation was extended from the infratrochanter to the greater trochanter (Fig. 5). The patient could get out of bed 3 weeks after this surgery; however, she did not adequately recover her walking ability and was confined to a wheelchair. The patient was not discharged to home and ended up living in a medical facility.
The number of periprosthetic fractures will increase in an aging society, owing to the increased resort to artificial joint replacement. According to Solarino et al. [1], the incidence of periprosthetic fracture in patients who underwent THA and BHA increased from 0.1–3.2% in 2003 to 0.1–18.0% in 2011; the corresponding increase in the number of patients with TKA was from 0.3% to 5.5%. Additionally, the reported fracture risk increased by 30% in cases where THA and TKA were performed on the ipsilateral lower limb, with an associated mortality rate of 31%; the reported postoperative life expectancy of patients with interprosthetic fractures occurring between artificial joints is 3.45 years. Therefore, fractures occurring after THA or TKA represent a major problem for patients and the society. The first periprosthetic fracture in our patient was a Su classification type III fracture. Some reports have described attempts to perform osteosynthesis for Su type III fractures [4]. However, CT analysis indicated that osteosynthesis was extremely difficult with both intramedullary nails and plates. Additionally, considering bone fragility due to diabetes mellitus and rheumatoid arthritis, strong and tight fixation was unlikely even if osteosynthesis was completed. Furthermore, early ambulation would not have been obtained. In this context, hinge-type TKA contributed to early ambulation. In fact, the patient could regain her walking ability after surgery. Because the risk of interprosthetic fracture increases after the placement of hip and knee prostheses with a stem on the ipsilateral femur, a plate for fracture prevention was installed during hinge-type TKA. Lehmann et al. [6] have conducted a strength simulation study in which a cemented hip stem was inserted into the ipsilateral femur; they compared an intact knee, a knee with a retrograde intramedullary nail, and a knee with a retrograde intramedullary nail and a preventive plate implanted on the lateral side. The results of the four-point bending test showed that the strength of the model with a preventive plate was superior to that of the other two models. Moreover, Walcher et al. [8] have reported that a minimal gap and/or overlap of at least 6 cm between the tips of a plate and a stem is recommended to avoid stress risers. In our patient, the distance between the stem tips was 53 mm (Fig. 3a). The distinct possibility of an interprosthetic fracture caused by a fall was considered; therefore, installing a plate as a preventive measure was necessary. In particular, our patient was at a high risk of falling. Plate installation prevented an interprosthetic fracture caused by repeated falls. The second periprosthetic fracture was diagnosed as Vancouver classification type B2. Revision surgery using a long stem is generally recommended for this type of fracture [10]. However, highly invasive procedures, such as stem revision surgery, should be avoided in this setting. Osteosynthesis was completed in this case; however, the patient’s walking ability could not be regained. In the literature, osteosynthesis is considered acceptable for this type of fracture in patients with low activity [11]. Therefore, osteosynthesis is relevant in particular cases. Our plate positioning was >6 cm overlapping (108 mm) (Fig. 3a); therefore, there seemed to be no problem with the overlapping distance; however, periprosthetic fractures could not be prevented, although interprosthetic fractures could be prevented. Soenen et al. [7] have developed a model in which a femoral implant of TKA with a stem was inserted into the ipsilateral femur with the THA or BHA stem inserted in the proximal site of the femur. Simulation studies were conducted to replicate walking, lateral fall, and four-point bending loads to evaluate the stress applied to the femoral shaft between the stems by changing the length of the stems for TKA. The results showed that during walking, the stress is dispersed throughout the femur bone without hip and knee prostheses; however, upon installation of the hip joint stem and the elongation of the femoral stem of TKA, the stress is concentrated at the diaphysis between the stem tips. Additionally, in the four-point bending test, the risk of fracture increased as the cutoff value was set to 110 mm between the stems. Therefore, the authors recommended securing a stem tip distance of ≥110 mm. Furthermore, on simulation of lateral fall, the stress was found to be concentrated on the femoral neck in the absence of any hip stem; however, after the insertion of a hip stem, the stress was largely concentrated on the infratrochanter. Considering that the fracture site at the proximal end of the plate was in the infratrochanter (an area with a high propensity for stress concentration according to Soenen’s study [7]), the occurrence of fractures at this site may not have been entirely accidental. Considering that in a case of hip stem installation, the stress caused by a fall is concentrated on the infratrochanter, this plate reinforcement should have extended to a more upper level to the trochanter; this is a point to reflect in the future. However, this fracture may have occurred even if the range of the plate was long enough. In a study by Zuurmond et al. [3], 14% of patients who underwent surgery for periprosthetic fracture were reoperated due to refracture or implant failure. Generally, periprosthetic fractures in elderly patients will lead to complications, such as infection, pseudoarthrosis, rupture of the fixation site, and re-fall; thus, highly invasive surgeries should be avoided in elderly patients [1, 2]. Therefore, it is considered that the surgical procedure and the degree of invasion must be customized according to the characteristics of each case. Lastly, familiarity of the surgeons with the mechanism and site of stress concentration is a key imperative from the perspective of prevention and treatment of periprosthetic or interprosthetic fractures.
We report a patient who sustained repeated periprosthetic fracture of the femur. A periprosthetic fracture can occur despite the installation of a fracture prevention plate. With a THA or BHA stem inserted, a fall could result in a subtrochanteric fracture. After the insertion of a hip prosthesis, the infratrochanteric area is most susceptible to the stress caused by a fall; surgeons should be careful when performing plate reinforcement to the femur.
Plate installation reinforcement for preventing an interprosthetic fracture is recommended, as shorter stem tip distance in patients with hip and knee stems inserted into the ipsilateral femur. Re-falls of elderly patients are common; therefore, periprosthetic refractures can inevitably occur, and this case report’s fracture occurred even with a plate reinforcement. However, from a mechanical viewpoint, there are some stress concentration points where peri- or interprosthetic fractures can be occur, and the surgeon should be aware of this fact.
References
- 1.Solarino G, Vicenti G, Moretti L, Abate A, Spinarelli A, Moretti B. Interprosthetic femoral fractures--A challenge of treatment. A systematic review of the literature. Injury 2014;45:362-8. [Google Scholar]
- 2.Ebraheim NA, Kelley LH, Liu X, Thomas IS, Steiner RB, Liu J. Periprosthetic distal femur fracture after total knee arthroplasty: A systematic review. Orthop Surg 2015;7:297-305. [Google Scholar]
- 3.Zuurmond RG, Van Wijhe W, Van Raay JJ, Bulstra SK. High incidence of complications and poor clinical outcome in the operative treatment of periprosthetic femoral fractures: An analysis of 71 cases. Injury 2010;41:629-33. [Google Scholar]
- 4.Su ET, DeWal H, Di Cesare PE. Periprosthetic femoral fractures above total knee replacements. J Am Acad Orthop Surg 2004;12:12-20. [Google Scholar]
- 5.Ochs B, Stockle U, Gebhard F. Interprosthetic fractures--a challenge of treatment. Eur Orthop Traumatol 2012;4:1-7. [Google Scholar]
- 6.Lehmann W, Rupprecht M, Hellmers N, Sellenschloh K, Briem D, Püschel K, et al. Biomechanical evaluation of peri- and interprosthetic fractures of the femur. J Trauma Acute Care Surg 2010;68:1459-63. [Google Scholar]
- 7.Soenen M, Baracchi M, De Corte R, Labey L, Innocenti B. Stemmed TKA in a femur with a total hip arthroplasty: Is there a safe distance between the stem tips? J Arthroplasty 2013;28:1437-45. [Google Scholar]
- 8.Walcher MG, Giesinger K, Sart RD, Day RE, Kuster MS. Plate positioning in periprosthetic or interprosthetic femur fractures with stable implantsd - A biomechanical study. J Arthroplasty 2016;31:2894-9. [Google Scholar]
- 9.Brady OH, Garbuz DS, Masri BA, Duncan CP. The reliability of validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplasty 2000;15:59-62. [Google Scholar]
- 10.Masri BA, Meek RM, Duncan CP. Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res 2004;420:80-95. [Google Scholar]
- 11.Niikura T, Lee SY, Sakai Y, Nishida K, Kuroda R, Kurosaka M. Treatment results of a periprosthetic femoral fracture case series: Treatment method for Vancouver type b2 fractures can be customized. Clin Orthop Surg 2014;6:138-45. [Google Scholar]








