A high clinical index of suspicion and moreover, proper communication about past medical history is required to approach a non-traumatic triceps’ tendon rupture.
Dr. Ioanna Lianou, Department of Orthopaedics and Trauma, General Hospital of Patras, Patras, Greece. E-mail: jolianou@hotmail.com
Introduction: Triceps’ tendon rupture is thought to be a relatively rare injury, and its exact incidence is unknown. As a result of the rareness of this injury, very few cases of weightlifters or bodybuilders taking androgenic anabolic steroids have been published in the literature to date. In this article, we report a very rare case of non-traumatic triceps tendon rupture in a professional body builder under androgenic anabolic steroids.
Case Report: A 32-year-old male patient, was admitted to our emergency department, reporting that while trying to maneuver his motorbike to avoid collision with another vehicle, he felt sudden pain at the posterior elbow and heard a popping sound. Active extension of the elbow was found to be reduced, raising suspicion of triceps tendon rupture. Ultrasound and magnetic resonance imaging revealed rupture of the triceps, confirming the clinical diagnosis. Intraoperatively, an almost complete rupture of the triceps was noted at its insertion into the olecranon. After the recognition and preparation of the triceps’ footprint, two 3.5 mm titanium bone sutured anchors were placed at the anatomical insertion of the tendon, and the tendon was repaired using a modified double-row technique. Follow-up at 6 months and 1 year postoperatively revealed perfect Mayo Elbow Performance and Oxford Elbow Scores with no residual pain or range of motion deficits; triceps strength had returned to pre-injury levels
Conclusion: Triceps tendon rupture is thought to be a relatively rare injury and among the rarest tendon injuries. It usually occurs in patients with systematic diseases, such as renal disease, or on medication, such as androgenic anabolic steroid use. As a result of its rareness, very few cases of weightlifters or bodybuilders taking steroids have been reported in the literature. To our knowledge, this is the first case of non-traumatic triceps tendon rupture in a bodybuilder under oral androgenic anabolic steroids.
Keywords: Triceps tendon, rupture, non-traumatic, athlete, anabolic, steroids.
The triceps brachii is the main operator of elbow extension and is composed of three different muscle bellies: the long head, which originates from the infraglenoid tuberosity, and the lateral and medial ones, which both originate from the posterior humerus. The muscle is innervated by the radial nerve, and its vascular supply originates from the profunda brachii artery. The insertion to the olecranon consists of the central tendon and the lateral expansion of the triceps in a dome-shaped footprint, which preserves elbow extension when central tendon rupture happens. Triceps tendon rupture (TTR), which is a relatively rare injury as it accounts for approximately 1% of all tendon ruptures, was first described in 1868 by Partridge [1]. Even if it mainly affects patients between 30 and 50 years old, cases in children or patients in the eighth decade have been reported, too. This injury is twice as frequent among male patients compared to women [2]. These ruptures can be a partial tear of the musculotendinous area, a complete tear at the insertional site, or an interstitial tear in luminous shape [3] and can occur in a variety of different mechanisms of injury, which mainly summarize falls on an outstretched arm and eccentric contraction, which is usually described among weightlifters. As a result of the elbow extensor anatomy, even in cases of complete rupture, some strength in the elbow extension can be preserved, which can cause a missed diagnosis and delay treatment. The diagnosis is sometimes confirmed by the presence of the flake sign in the plain radiographs, which is distinctive of an avulsion fracture of the olecranon process. The flake sign is present in 61% of all cases with TTR [4]. The definitive diagnosis and evaluation of the degree of the injury are better achieved using magnetic resonance imaging (MRI). Several risk factors have been reported that may predispose to this condition. Systemic disorders such as osteogenesis imperfecta, Marfan syndrome, renal osteodystrophy, rheumatoid arthritis, type 1 diabetes mellitus, renal hypocalcemia, and liver disease have been related to the injury [5, 6]. Taking into account that this type of injury is most common among athletes, including weightlifters and football players, chronic use of androgenic anabolic steroids (AAS) and corticosteroids is also considered a risk factor. Even if the reduction in the elasticity of the tendons as a result of the use of extreme doses of AAS is widely accepted by the existing literature, which mainly includes a number of case reports [7], the AAS-associated tendon rupture is not well supported. Most cases of TTR in the latter group occur in young adults after strenuous exercise or trauma. To the best of our knowledge, this is the first case of atraumatic TTR in a bodybuilder on AAS use.
A 32-year-old male professional bodybuilder athlete presented to the author’s institute’s Emergency Department (ED) complaining of acute-onset pain and swelling of the right elbow (dominant hand). The patient reported that while trying to maneuver his motorbike to avoid a collision with another vehicle, he felt sudden pain at the posterior elbow and heard a popping sound. The patient reported to the ED fully ambulatory and denied falling from the vehicle or any other direct or indirect body contact or collision during the reported event. 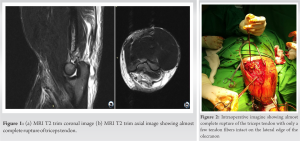 His past medical history was remarkable for a myocardial infarction 6 months ago that was managed with the placement of two coronary stents. The patient has been on dual antiplatelet therapy (aspirin 100 mg daily and clopidogrel 75 mg daily) since. He also reported regular use of oral AAS such as Boldenone, Testosterone, Metenolone, Trenbolone, and Mesterolone in cycles for more than a decade and Stanozolol almost daily, with varying doses, for the last 2½ years. On clinical examination, vital signs were within normal limits, and swelling of the posterior aspect of the right elbow was noted. Active extension of the elbow was reduced to a score of 2 out of 5 in the Medical Research Council Manual Muscle Testing scale [8], raising suspicion for TTR. Radiography did not disclose any fracture or flake sign [4], and subsequent ultrasound and MRI of the elbow were performed. Ultrasound and MRI revealed rupture of the triceps tendon at its insertion, confirming the diagnosis (Figs. 1a, b). The patient was admitted for further surgical management. During the operation, the patient was placed in the left lateral decubitus position with the right arm supported by a padded post; no tourniquet was used during the procedure. The rupture was approached with a linear incision over the posterior elbow, as outlined by Conti Mica et al. [9]. Intraoperatively, almost complete rupture of the triceps was noted at its insertion into the olecranon, with only a few tendon fibers on the lateral side of the muscle intact (Fig. 2). No avulsed fragments were noted. The ulnar nerve was identified and protected. The tendon was debrided at its insertion, the hematoma was removed, and the retraction of the tendon was evaluated (Fig. 3). After the recognition and preparatio
His past medical history was remarkable for a myocardial infarction 6 months ago that was managed with the placement of two coronary stents. The patient has been on dual antiplatelet therapy (aspirin 100 mg daily and clopidogrel 75 mg daily) since. He also reported regular use of oral AAS such as Boldenone, Testosterone, Metenolone, Trenbolone, and Mesterolone in cycles for more than a decade and Stanozolol almost daily, with varying doses, for the last 2½ years. On clinical examination, vital signs were within normal limits, and swelling of the posterior aspect of the right elbow was noted. Active extension of the elbow was reduced to a score of 2 out of 5 in the Medical Research Council Manual Muscle Testing scale [8], raising suspicion for TTR. Radiography did not disclose any fracture or flake sign [4], and subsequent ultrasound and MRI of the elbow were performed. Ultrasound and MRI revealed rupture of the triceps tendon at its insertion, confirming the diagnosis (Figs. 1a, b). The patient was admitted for further surgical management. During the operation, the patient was placed in the left lateral decubitus position with the right arm supported by a padded post; no tourniquet was used during the procedure. The rupture was approached with a linear incision over the posterior elbow, as outlined by Conti Mica et al. [9]. Intraoperatively, almost complete rupture of the triceps was noted at its insertion into the olecranon, with only a few tendon fibers on the lateral side of the muscle intact (Fig. 2). No avulsed fragments were noted. The ulnar nerve was identified and protected. The tendon was debrided at its insertion, the hematoma was removed, and the retraction of the tendon was evaluated (Fig. 3). After the recognition and preparatio n of the triceps’s footprint, two 3.5 mm titanium bone suture anchors (DORATEK PIEX®, TIAN-0351) were placed at the anatomical insertion of the tendon, and the tendon was repaired using a modified double-row technique. Two sutures from each anchor were passed in a Krackow-type whipstitch fashion through the tendon, and each strand from the whipstitch was tied down to the matched suture anchor. Mattress sutures from each pair of stitches were placed in the distal tendon approximately 2 cm proximal to the end. A 2.5 mm transosseous tunnel was made on the proximal ulna, and the sutures’ tails of the lateral anchor were passed through it in a figure-of-eight configuration and tied securely to the remaining sutures’ tails of the medial anchor, providing near complete coverage of the anatomic footprint (Fig. 4). Full range of motion (ROM) was documented intraoperatively. The arm was initially placed in 30° elbow flexion with a plaster splint. The postoperative period was uneventful, and the patient was subsequently discharged. Close follow-up ensued; 30° elbow flexion was maintained for 2 weeks postoperatively. Subsequently, the patient was moved to a hinged brace with adjustable elbow flexion and extension. The rehabilitation protocol followed Kocialkowski et al. [10]. In the first 2 weeks, the elbow was placed in a 30° plaster splint until the soft tissue and hematoma subsided. At 2–4 weeks, active elbow flexion and extension to 0–60° with supination and pronation exercises were allowed. Up to 6 weeks, active elbow flexion was permitted to 90° and advanced to 120° at 8 weeks postoperatively, when the hinged brace was removed (Fig. 5). Further rehabilitation protocols included isometric exercises at varying elbow angles in both open and closed chain mode, with a gradual return to normal activities. Follow-up at 6 months and 1 year postoperatively revealed perfect Mayo Elbow Performance and Oxford Elbow Scores [11] in both appointments with no residual pain or ROM deficit; triceps strength had returned to the pre-injury levels (Fig. 6 a, b). Written consent was given by the patient for the publication of this case and the images that accompanied this article on his last follow-up visit.
n of the triceps’s footprint, two 3.5 mm titanium bone suture anchors (DORATEK PIEX®, TIAN-0351) were placed at the anatomical insertion of the tendon, and the tendon was repaired using a modified double-row technique. Two sutures from each anchor were passed in a Krackow-type whipstitch fashion through the tendon, and each strand from the whipstitch was tied down to the matched suture anchor. Mattress sutures from each pair of stitches were placed in the distal tendon approximately 2 cm proximal to the end. A 2.5 mm transosseous tunnel was made on the proximal ulna, and the sutures’ tails of the lateral anchor were passed through it in a figure-of-eight configuration and tied securely to the remaining sutures’ tails of the medial anchor, providing near complete coverage of the anatomic footprint (Fig. 4). Full range of motion (ROM) was documented intraoperatively. The arm was initially placed in 30° elbow flexion with a plaster splint. The postoperative period was uneventful, and the patient was subsequently discharged. Close follow-up ensued; 30° elbow flexion was maintained for 2 weeks postoperatively. Subsequently, the patient was moved to a hinged brace with adjustable elbow flexion and extension. The rehabilitation protocol followed Kocialkowski et al. [10]. In the first 2 weeks, the elbow was placed in a 30° plaster splint until the soft tissue and hematoma subsided. At 2–4 weeks, active elbow flexion and extension to 0–60° with supination and pronation exercises were allowed. Up to 6 weeks, active elbow flexion was permitted to 90° and advanced to 120° at 8 weeks postoperatively, when the hinged brace was removed (Fig. 5). Further rehabilitation protocols included isometric exercises at varying elbow angles in both open and closed chain mode, with a gradual return to normal activities. Follow-up at 6 months and 1 year postoperatively revealed perfect Mayo Elbow Performance and Oxford Elbow Scores [11] in both appointments with no residual pain or ROM deficit; triceps strength had returned to the pre-injury levels (Fig. 6 a, b). Written consent was given by the patient for the publication of this case and the images that accompanied this article on his last follow-up visit.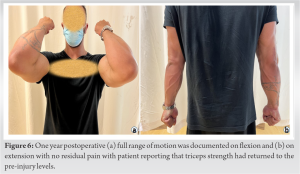
TTR is a relatively rare injury. Their exact incidence is unknown; however, Anzel et al., in a series of more than 1000 patients with tendon injuries, reported the occurrence of TTR in <1% of the cases [12]. As a result of the rareness of this injury, very few TTR cases of weightlifters or bodybuilders taking AAS have been reported in the literature to date (Table 1). 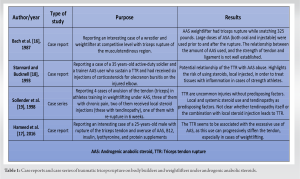 However, most of them occurred during strenuous exercise workouts or after direct impact or a fall [4]. Various risk factors have been recognized, such as systemic conditions or substances, which most often occur in amateur or professional weightlifters. Medical conditions such as renal, thyroid, and parathyroid disease have been associated with TTR and systemic steroids; IM-injected steroids and oral AAS use have also been reported. Specifically, renal disease and AAS are the most common medical conditions associated with TTR [4]. A combination of a weightlifter who is using oral and/or IM-injected anabolic steroids is even more worrisome for the occurrence of TTR, as in our case. AAS may exert deleterious effects on the tendons, and therefore, these patients may be more prone to TTR. One of the two main hypotheses about the association between the use of AAS and the TTR summarizes muscle hypertrophy without concomitant strengthening of the tendon, causing rupture under stress loading, as a result of the AAS. In other words, the use of AAS blocks the beneficial effects of exercise [13]. According to the alternative hypothesis, which is based on the dysplasia of the collagen and proved in animal models, the combination of excessive doses of AAS with muscle training can change the tendon structure and make them stiffer and weaker than usual [11, 12, 13, 14]. However, the AAS effect weans off completely after substance discontinuation [14]. Even if no clear evidence exists about the destructive effect of AAS use on human tendons, the association between high risk of upper limb tendons rupture and AAS use is supported by studies (Table 2), especially when the exposed population is compared with subjects not on an AAS training program [15]. TTR may be more common in weightlifters or bodybuilders on AAS [16, 17, 18, 19]. Stannard and Bucknell [18] reported a young active-duty military trainer and power weightlifter with history of prior oral and IM AAS use that presented with TTR after weightlifting. However, the patient had also been treated with IM steroids for olecranon bursitis the year prior to the TTR. Therefore, it is unknown whether the use of AAS or IM steroids for the bursitis was the culprit for the TTR. Furthermore, in our case, the TTR occurred after an abrupt upper extremity move and was not the result of weightlifting or any other exercise or trauma. Bach et al.
However, most of them occurred during strenuous exercise workouts or after direct impact or a fall [4]. Various risk factors have been recognized, such as systemic conditions or substances, which most often occur in amateur or professional weightlifters. Medical conditions such as renal, thyroid, and parathyroid disease have been associated with TTR and systemic steroids; IM-injected steroids and oral AAS use have also been reported. Specifically, renal disease and AAS are the most common medical conditions associated with TTR [4]. A combination of a weightlifter who is using oral and/or IM-injected anabolic steroids is even more worrisome for the occurrence of TTR, as in our case. AAS may exert deleterious effects on the tendons, and therefore, these patients may be more prone to TTR. One of the two main hypotheses about the association between the use of AAS and the TTR summarizes muscle hypertrophy without concomitant strengthening of the tendon, causing rupture under stress loading, as a result of the AAS. In other words, the use of AAS blocks the beneficial effects of exercise [13]. According to the alternative hypothesis, which is based on the dysplasia of the collagen and proved in animal models, the combination of excessive doses of AAS with muscle training can change the tendon structure and make them stiffer and weaker than usual [11, 12, 13, 14]. However, the AAS effect weans off completely after substance discontinuation [14]. Even if no clear evidence exists about the destructive effect of AAS use on human tendons, the association between high risk of upper limb tendons rupture and AAS use is supported by studies (Table 2), especially when the exposed population is compared with subjects not on an AAS training program [15]. TTR may be more common in weightlifters or bodybuilders on AAS [16, 17, 18, 19]. Stannard and Bucknell [18] reported a young active-duty military trainer and power weightlifter with history of prior oral and IM AAS use that presented with TTR after weightlifting. However, the patient had also been treated with IM steroids for olecranon bursitis the year prior to the TTR. Therefore, it is unknown whether the use of AAS or IM steroids for the bursitis was the culprit for the TTR. Furthermore, in our case, the TTR occurred after an abrupt upper extremity move and was not the result of weightlifting or any other exercise or trauma. Bach et al. 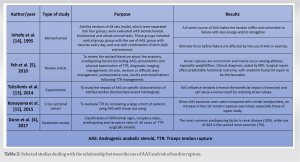 reported a 3-time Olympic weightlifter on AAS who was diagnosed with a missed chronic TTR; he was diagnosed almost 2½ years after the initial insult and had a good postoperative outcome [16]. Hameed et al. also reported a late TTR diagnosis in a young bodybuilder; however, he admitted to using oral and IM AAS as well as IM enhancement oil, IM vitamin B12, and rapid-acting insulin as adjuvants for his training sessions and competitions [17]. Therefore, it is not certain whether the use of AAS was the major cause of the TTR. Lastly, Sollender et al. reported four bodybuilders on AAS who presented with TTR after vigorous exercise [19]. In our case, on the contrary, the patient only admitted to abusing AAS, rendering them a major possible cause of the TTR, denying recent exercise or trauma as a cause of his injury. The treatment of the TTR is based on the remaining extension strength of the affected upper limb and the location of the tear, considering the role of lateral triceps expansion and anconeus on elbow extension and patients’ functional status [5]. Partial tears <50%, more than 50% in sedentary patients, or complete tears of the muscle belly are usually treated with splinting. The splint immobilization at 30° flexion ranges from 3–4 weeks and is followed by gradual elbow flexion mobilization. All cases of complete distal triceps tear or partial tears >50% of the tendon with extension weakness in active patients eligible for surgery should be operatively treated [2, 5]. Acute tears should be treated with early primary repair within 2–3 weeks (cases treated at 8 months have also been described) [20]. All different treatment techniques are summarized in the advance of the acute tear, which attaches the olecranon with heavy sutures through tunnels, which pass throughout it. Moreover, the lateral triceps expansion should be used as an augmentation, and any disruption should be repaired. The postoperative care includes immobilization at 30–45° for 2 weeks and then replacement of the immobilization with a hinged brace or static thermoplastic splint at 30–60° of flexion. According to the published protocols, active gentle smooth flexion and passive or gravity-assisted extension starts at 2 weeks, while active elbow extension should be encouraged at 4 weeks [21]. Moreover, gentle strengthening begins at 6 weeks until 3 months, and weightlifting not before 4–6 months after surgical treatment. More accelerated protocols have been recommended when strong reconstruction is achieved. To our knowledge, this is the first case of non-traumatic TTR in a male bodybuilder patient taking oral AAS.
reported a 3-time Olympic weightlifter on AAS who was diagnosed with a missed chronic TTR; he was diagnosed almost 2½ years after the initial insult and had a good postoperative outcome [16]. Hameed et al. also reported a late TTR diagnosis in a young bodybuilder; however, he admitted to using oral and IM AAS as well as IM enhancement oil, IM vitamin B12, and rapid-acting insulin as adjuvants for his training sessions and competitions [17]. Therefore, it is not certain whether the use of AAS was the major cause of the TTR. Lastly, Sollender et al. reported four bodybuilders on AAS who presented with TTR after vigorous exercise [19]. In our case, on the contrary, the patient only admitted to abusing AAS, rendering them a major possible cause of the TTR, denying recent exercise or trauma as a cause of his injury. The treatment of the TTR is based on the remaining extension strength of the affected upper limb and the location of the tear, considering the role of lateral triceps expansion and anconeus on elbow extension and patients’ functional status [5]. Partial tears <50%, more than 50% in sedentary patients, or complete tears of the muscle belly are usually treated with splinting. The splint immobilization at 30° flexion ranges from 3–4 weeks and is followed by gradual elbow flexion mobilization. All cases of complete distal triceps tear or partial tears >50% of the tendon with extension weakness in active patients eligible for surgery should be operatively treated [2, 5]. Acute tears should be treated with early primary repair within 2–3 weeks (cases treated at 8 months have also been described) [20]. All different treatment techniques are summarized in the advance of the acute tear, which attaches the olecranon with heavy sutures through tunnels, which pass throughout it. Moreover, the lateral triceps expansion should be used as an augmentation, and any disruption should be repaired. The postoperative care includes immobilization at 30–45° for 2 weeks and then replacement of the immobilization with a hinged brace or static thermoplastic splint at 30–60° of flexion. According to the published protocols, active gentle smooth flexion and passive or gravity-assisted extension starts at 2 weeks, while active elbow extension should be encouraged at 4 weeks [21]. Moreover, gentle strengthening begins at 6 weeks until 3 months, and weightlifting not before 4–6 months after surgical treatment. More accelerated protocols have been recommended when strong reconstruction is achieved. To our knowledge, this is the first case of non-traumatic TTR in a male bodybuilder patient taking oral AAS.
TTR is a rare injury that is usually reported in patients with renal disease or AAS users and, in most cases, occurs after strenuous exercise or trauma. TTR without trauma or as a result of exercise is even rarer, and therefore, a high clinical index of suspicion is required to diagnose this condition in order to provide appropriate care for the patients. The meticulous clinical evaluation, the proper diagnostic imaging, and moreover, the proper communication with the patient are essential. particularly when we have to deal with young bodybuilders. The quest for muscle hypertrophy at any cost has increased the use of AAS among this group, so we need to be suspicious and aware in order to recognize the potential “hidden” and “rare” injuries in these demanding patients, and furthermore, we should inform patients under AAS of the potential dangers that this “habit” involves.
It seems to be common knowledge that competitive athletes under AAS are susceptible to non-traumatic tendon ruptures, including TTR. Taking into account the hypothesized impact of this usage on tendon strength and structure, a strong augmented tendon repair accompanied by a meticulous rehabilitation program is thought to be the “gold standard” for a good clinical outcome. Of equal importance is patients’ compliance with postoperative guidelines and rehabilitation programs in order to diminish rerupture risk.
References
- 1.Partridge A. A case report of a case of ruptured triceps cubiti. Med Times Gaz 1868;1:175. [Google Scholar]
- 2.Tom JA, Kumar NS, Cerynik DL, Mashru R, Parrella MS. Diagnosis and treatment of triceps tendon injuries: A review of the literature. Clin J Sport Med 2014;24:197-204. [Google Scholar]
- 3.Morrey B. Rupture of the triceps tendon. In: Morrey B, editor. The Elbow and Its Disorders. 4th ed. Philadelphia; Saunders; 2009. p. 536-46. [Google Scholar]
- 4.Dunn JC, Kusnezov N, Fares A, Rubin S, Orr J, Friedman D, et al. Triceps tendon ruptures: A systematic review. Hand (N Y) 2017;12:431-8. [Google Scholar]
- 5.Yeh PC, Dodds SD, Smart LR, Mazzocca AD, Sethi PM. Distal triceps rupture. J Am Acad Orthop Surg 2010;18:31-40. [Google Scholar]
- 6.Clayton ML, Thirupathi RG. Rupture of the triceps tendon with olecranon bursitis. A case report with a new method of repair. Clin Orthop Relat Res 1984;184:183-5. [Google Scholar]
- 7.Jones IA, Togashi R, Hatch GF 3rd, Weber AE, Vangsness CT Jr. Anabolic steroids and tendons: A review of their mechanical, structural, and biologic effects. J Orthop Res 2018;36:2830-41. [Google Scholar]
- 8.Shahgholi L, Bengtson KA, Bishop AT, Shin AY, Spinner RJ, Basford JR, et al. A comparison of manual and quantitative elbow strength testing. Am J Phys Med Rehabil 2012;91:856-62. [Google Scholar]
- 9.Conti Mica M, van Riet R. Triceps tendon repair. JBJS Essent Surg Tech 2018;8:e4. [Google Scholar]
- 10.Kocialkowski C, Carter R, Peach C. Triceps tendon rupture: Repair and rehabilitation. Shoulder Elbow 2018;10:62-5. [Google Scholar]
- 11.Giannaka M, Andrigiannakis A, Dimitriadis Z, Fandridis E, Kapreli E, Strimpakos N. Cross-cultural validation of the oxford elbow score and mayo elbow performance score in greek. Musculoskelet Sci Pract 2022;57:102499. [Google Scholar]
- 12.Anzel SH, Covey KW, Weiner AD, Lipscomb PR. Disruption of muscles and tendons; an analysis of 1, 014 cases. Surgery 1959;45:406-14. [Google Scholar]
- 13.Tsitsilonis S, Chatzistergos PE, Mitousoudis AS, Kourkoulis SK, Vlachos IS, Agrogiannis G, et al. Anabolic androgenic steroids reverse the beneficial effect of exercise on tendon biomechanics: An experimental study. Foot Ankle Surg 2014;20:94-9. [Google Scholar]
- 14.Inhofe PD, Grana WA, Egle D, Min KW, Tomasek J. The effects of anabolic steroids on rat tendon. An ultrastructural, biomechanical, and biochemical analysis. Am J Sports Med 1995;23:227-32. [Google Scholar]
- 15.Kanayama G, DeLuca J, Meehan WP 3rd, Hudson JI, Isaacs S, Baggish A, et al. Ruptured tendons in anabolic-androgenic steroid users: A cross-sectional cohort study. Am J Sports Med 2015;43:2638-44. [Google Scholar]
- 16.Bach BR Jr, Warren RF, Wickiewicz TL. Triceps rupture. A case report and literature review. Am J Sports Med 1987;15:285-9. [Google Scholar]
- 17.Hameed M, Sahu A, Johnson MB. Muscle mania: The quest for the perfect body. BMJ Case Rep 2016;2016:bcr2016217208. [Google Scholar]
- 18.Stannard JP, Bucknell AL. Rupture of the triceps tendon associated with steroid injections. Am J Sports Med 1993;21:482-5. [Google Scholar]
- 19.Sollender JL, Rayan GM, Barden GA. Triceps tendon rupture in weight lifters. J Shoulder Elbow Surg 1998;7:151-3. [Google Scholar]
- 20.Inhofe PD, Moneim MS. Late presentation of triceps rupture. A case report and review of the literature. Am J Orthop (Belle Mead NJ) 1996;25:790-2. [Google Scholar]
- 21.van Riet RP, Morrey BF, Ho E, O'Driscoll SW. Surgical treatment of distal triceps ruptures. J Bone Joint Surg Am 2003;85:1961-7. [Google Scholar]