Published online Nov 6, 2019. doi: 10.12998/wjcc.v7.i21.3632
Peer-review started: May 3, 2019
First decision: September 9, 2019
Revised: September 27, 2019
Accepted: October 5, 2019
Article in press: October 5, 2019
Published online: November 6, 2019
In children with osteosarcoma around the knee joint without epiphysis involvement, joint-sparing surgery seems to be an ideal way to retain knee joint function. However, there are two points of debate with regard to the technique: How to accurately achieve a safe surgical margin, and how to achieve intercalary reconstruction of the massive bone defect following resection of the tumor.
We present the case of an 8-year-old girl with osteosarcoma of the distal femur without involvement of the epiphysis. Epiphyseal distraction was applied to separate the epiphysis and metaphysis, and this provided a safe surgical margin. The massive bone defect was reconstructed with a custom-made antibiotic-loaded polymethyl methacrylate (PMMA) construct combined with a free non-vascularized fibular graft. Six months after surgery, bone union between the autograft and host bone was confirmed in both the proximal and distal femur by computer tomography (CT) examination. Moreover, considerable callus formation was found around the PMMA construct. After 28 mo of follow-up, there was no sign of recurrence or metastasis. The patient could walk without any aid and carry out her daily life activities satisfactorily.
In cases of osteosarcoma without epiphysis involvement, epiphyseal distraction can be easily applied to obtain a safe margin. Hybrid reconstruction with an antibiotic-loaded PMMA construct combined with a free non-vascularized fibular graft has the advantages of being easy to manufacture, less time-consuming to place, and less likely to get infected, while also ensuring bone union. Our case provides an alternative technique for biological reconstruction after joint-sparing surgery in patients with osteosarcoma around the knee without epiphyseal involvement.
Core tip: Epiphyseal distraction can be applied to obtain a safe margin in the osteosarcoma patient without epiphysis involvement. Hybrid reconstruction with an antibiotic-loaded polymethyl methacrylate construct combined with a free non-vascularized fibular graft has advantages such as easy manufacturing, less time-consuming, lower chances of infection, and better bone union.
- Citation: Liang YH, He HB, Zhang C, Liu YP, Wan J. Epiphyseal distraction and hybrid reconstruction using polymethyl methacrylate construct combined with free non-vascularized fibular graft in pediatric patients with osteosarcoma around knee: A case report. World J Clin Cases 2019; 7(21): 3632-3638
- URL: https://www.wjgnet.com/2307-8960/full/v7/i21/3632.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i21.3632
Osteosarcoma, which is the most common primary malignant bone tumor, often occurs around the knee in children and adolescents. With the advances in neo-adjuvant chemotherapy and radiological techniques, there is no difference in the incidence of local recurrence and metastasis between patients who undergo amputation and those who undergo en bloc resection (wide resection) under a safe surgical margin[1].
In cases of osteosarcoma where the epiphysis is not involved, joint-sparing surgery is considered to be an ideal way to achieve good function. In joint-sparing surgery, there are two issues that must be considered: Having a safe surgical margin and intercalary reconstruction of massive bone defects. Computer-aided navigation and the 3D printing patient-specific instrument are useful for performing precise resection and ensuring a safe tumor margin[2]. However, precise resection could not be easily applied without all of these methods, which could potentially increase the risk of local recurrence.
There are many methods for intercalary reconstruction of massive bone defect resulting from tumor resection. Some surgeons prefer using a massive allograft to fill the defect, but it carries the risk of infection, facture, and absorption[3]. An alternative is to use a free vascularized fibular graft along with it, in a method called the “hot-dog” technique[4]. However, the use of the “hot-dog” technique is limited because it requires a high level of expertise in microsurgery techniques. Additionally, prolonged operation time and reconstruction-related complications may delay adjuvant chemotherapy. Therefore, when considering options for reconstruction after tumor resection, it is important to consider techniques with lower complication rates, and use grafts with sufficient biological strength and durability.
We present here an interesting case of a girl with osteosarcoma in the distal femur without epiphysis involvement. Epiphyseal distraction was applied to ensure a safe surgical margin, and the massive bone defect after en bloc resection was reconstructed with a custom-made antibiotic-loaded polymethyl methacrylate (PMMA) construct combined with a free non-vascularized fibular graft.
An 8-year-old girl was admitted to our department on December 2, 2015. She presented with pain and a mass in her right thigh.
The patient reported that she noticed the mass 4 mo before, that she had been experiencing the pain all day and night, and that it was more severe at night. She had taken some traditional Chinese medicine, but there had been no obvious improvement. She denied having a history of trauma.
The family history was unremarkable.
On physical examination, an ill-defined, firm, palpable mass was found in the patient’s right distal thigh. Plain radiography demonstrated a distally destructed femur that had a densely ossified mass and a radiolucent region. A classic Codman triangle could be seen on the surface of the right femur metaphysis, in the median and lateral directions.
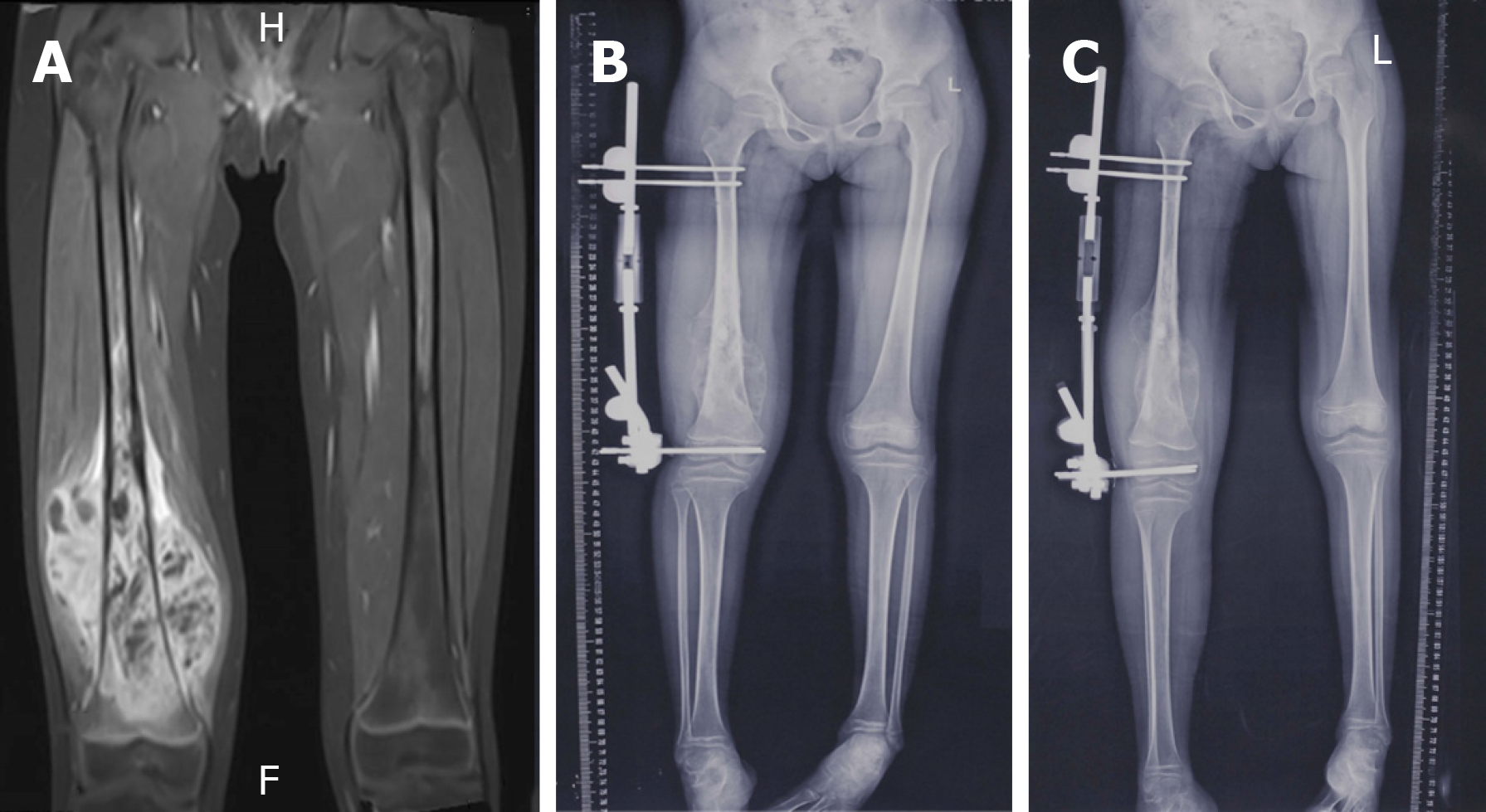
Computed tomography (CT) demonstrated a destructed femoral cortex in her metaphysis with a soft-tissue mass. Magnetic resonance imaging (MRI) revealed a destructed lesion in the middle and distal segments of the femur, and no invasion of the epiphysis (Figure 1A). Subsequent CT of the chest, as well as whole-body single-photon emission computed tomography (SPECT), revealed no metastases of the lesion or other bony abnormalities. Core-needle biopsy was performed, and based on histological evaluation of the sample, osteoblastic osteosarcoma was confirmed.
Osteoblastic osteosarcoma was confirmed.
The staging was regarded as IIB according to the Enneking classification[1], and both neoadjuvant chemotherapy [cisplatin (120 mg/m2) and ifosfamide (3 g/m2/d) were administered for 5 d, followed by doxorubicin (30 mg/m2/d) for 2 d]. After two cycles of chemotherapy, the response was evaluated at a multidisciplinary oncology meeting. According to RECIST 1.1, there was evidence of good response based on the sclerotic changes, good margination of the tumor observed on the radiography and CT images, marked shrinkage of any extension of the tumor into soft tissue demonstrated by MRI, and disappearance of abnormal accumulation on SPECT. This was further confirmed to be a complete response upon histological examination, which revealed a 100% tumor necrosis rate.
As there was no involvement of the epiphysis, a joint-sparing strategy was designed to treat this patient. As the distance between the tumor and the epiphysis was not sufficient for a safe surgical margin (Figure 1A), a two-stage surgery was planned. First, an epiphyseal distraction was made to separate the epiphysis and the diaphysis. It is imperative that the screws of the external fixator not be inserted into the tumor or reaction area, as this would result in iatrogenic contamination. Gradual distraction was started 3 d after the surgery, and it was performed at a rate of 1 mm/d (Figure 1B). During the period of distraction, the third cycle of chemotherapy was administered. The separation was confirmed by a plain radiograph taken 3 wk after the distraction period (Figure 1C).
In the second stage of the surgery, an incision was made along the extension of the medial thigh. A 2 cm cuff of healthy tissue was retained along the biopsy track, which was left in continuity with the specimen. The femur was osteotomized 20 cm away from the upper edge of the epiphysis according to the extent in MRI. Histopathological examination of the excised specimen was indicative of osteosarcoma with tumor-free margins all around. Then, the massive bone defect of the femoral diaphysis was reconstructed with a custommade intercalary PMMA construct combined with a free non-vascularized fibular graft. The custom-made PMMA construct was created as described in our previous studies[5,6].
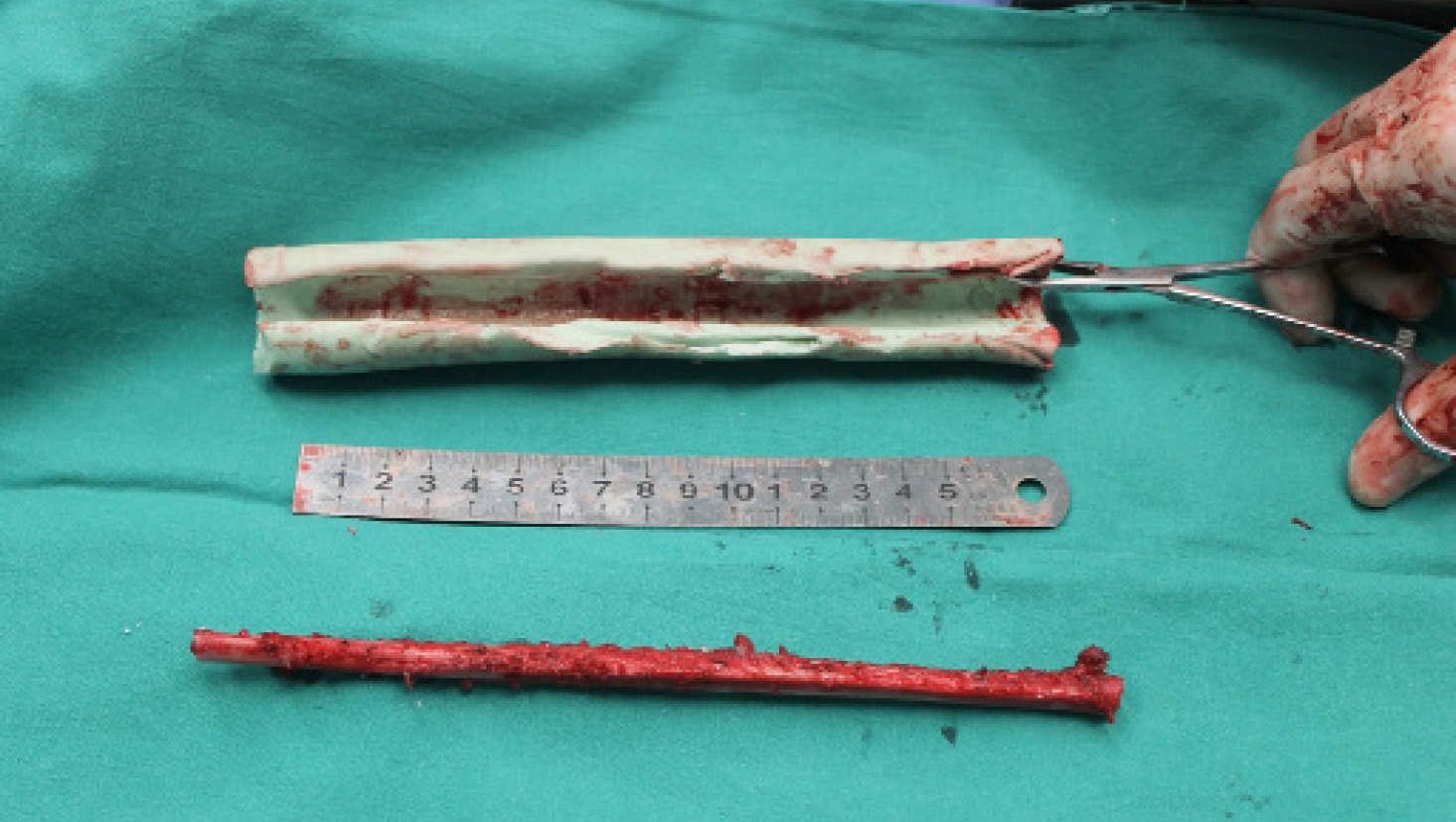
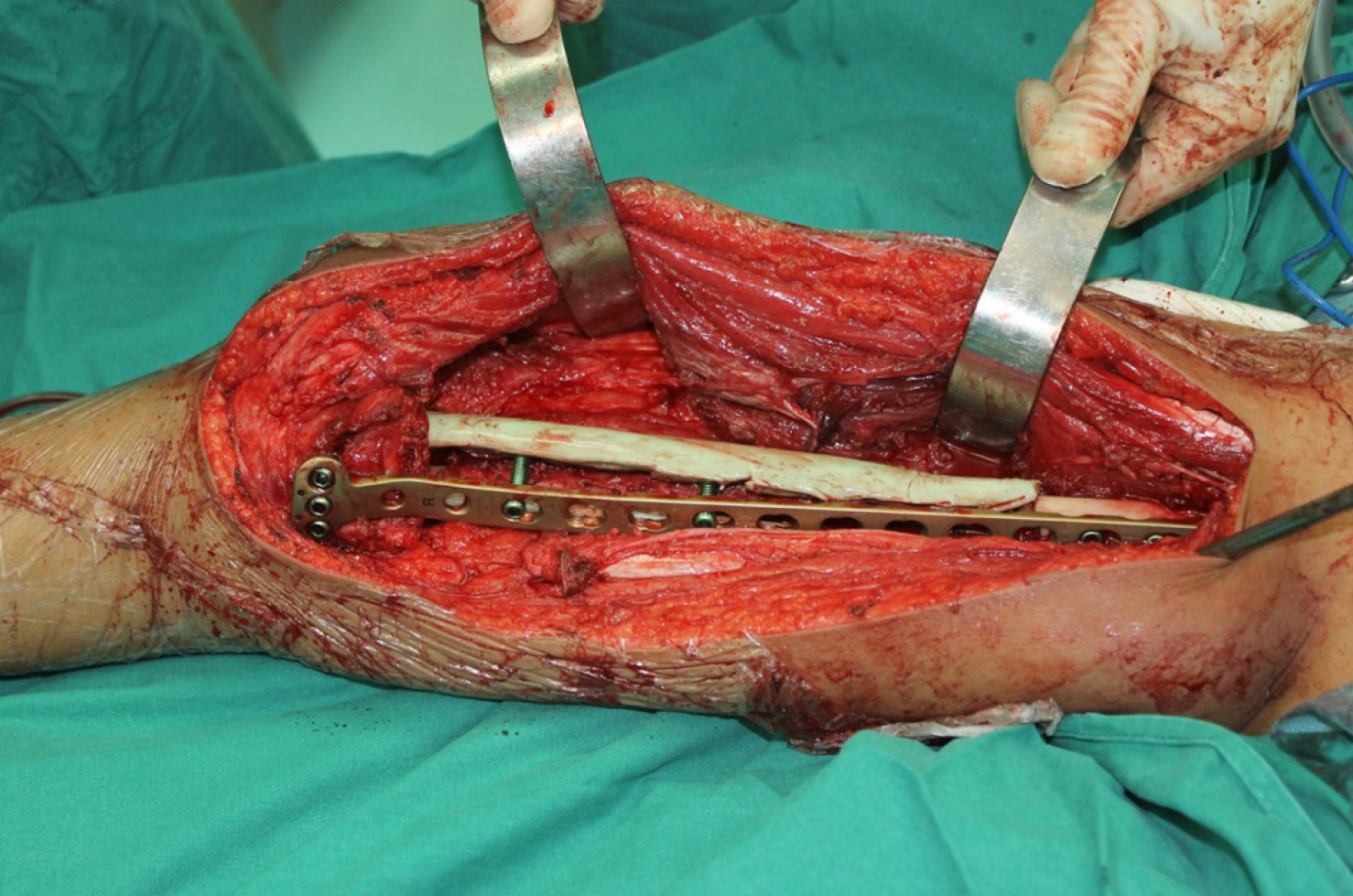
Briefly, two syringes (volume, 50 mL) were connected together and tailored according to the length of the bone defect (20 cm in this case). Two more syringes (volume, 20 mL) were placed in the 50 mL one with one of the edges attached. Then, PMMA bone cement was pressed into the space between the 50 mL and 20 mL syringes as much as possible after taking on the status of wiredrawing. After the cement had hardened, the syringe tubes were removed and the PMMA construct was thus successfully created. The free non-vascularized fibular graft was harvested using conventional methods and placed in the PMMA construct (Figure 2). For the sake of immediate stability, a locking compress plate was used medially as additional inner support (Figures 3 and 4).
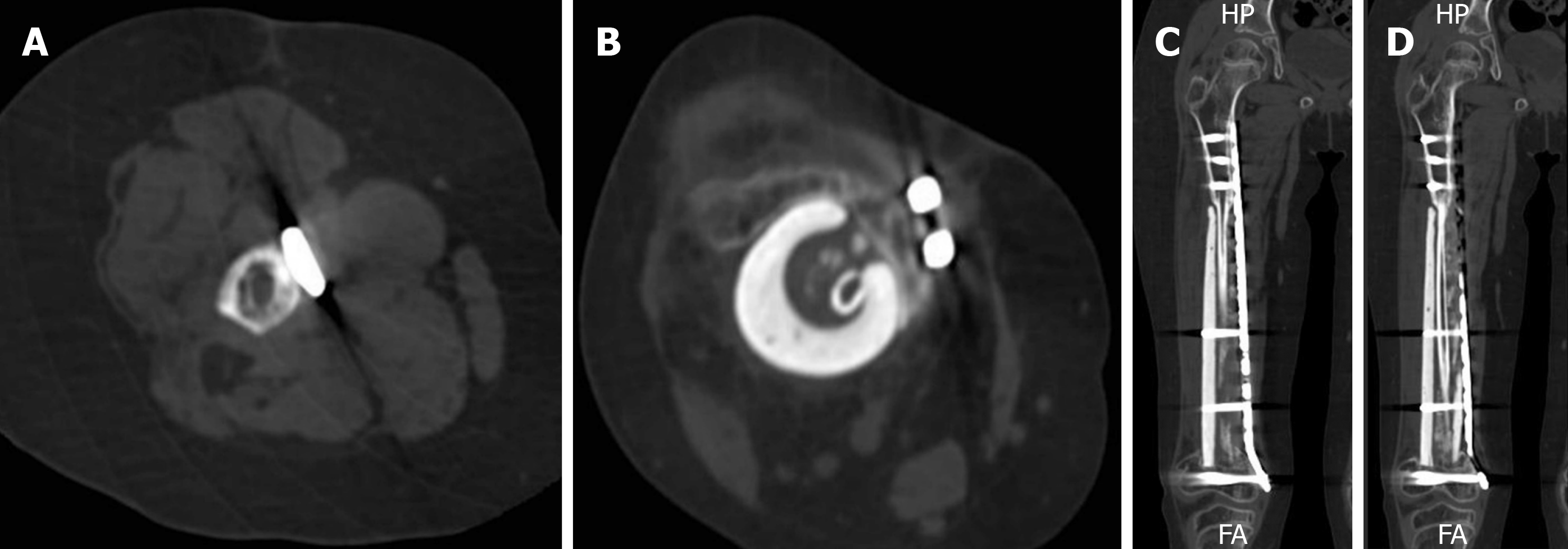
Prophylactic antibiotics were prescribed twice a day for 3 d. Two weeks after surgery, adjuvant chemotherapy was started; the protocol was the same as the preoperative one, and four cycles were administered. Two weeks after surgery, non-weight bearing mobilization was started with the help of a hinged knee brace. Full weight bearing with the brace was started after 6 wk and continued without the brace after 12 wk. Follow-up examination included clinical examination, ultrasound scanning, plain radiography, CT, MRI and SPECT for detecting any signs of recurrence or metastasis. The patient achieved bone union 6 mo after the surgery, as confirmed by CT (Figure 5). At the 28 mo follow-up, no local recurrence or metastasis was observed. The patient could walk without any aid and carry out her daily life activities satisfactorily (supplementary file 1).
In cases in which the tumor is adjacent to the growth plate, Cho et al[7], Cañadell et al[8], and Betz et al[9] recommend applying an epiphyseal distraction; they use this as a simple distraction technique for separating the growth plate from the degenerative layers of cells, and not as a routine lengthening procedure. This procedure entails the possibility of regeneration and some potential suppression effect on the tumor[10]. In our case, we used this technique to ensure a safe surgical margin, which was confirmed by histological evaluation. Moreover, no local recurrence had occurred up to the 28 mo follow-up. We therefore think that the technique used here is a feasible way of achieving a safe surgical margin in patients with an open growth plate.
There are many methods chosen in our department for intercalary reconstruction of massive bone defect[11,12]. However, biological reconstruction remains a challenge in osteosarcoma patients because chemotherapy has proven to have a negative effect on healing and revascularization of the allograft, which means that it could delay the union of the allograft and host bone. Many studies have shown that chemotherapy can decrease cell numbers and suppress cell proliferation at the junction of the allograft and host bone. Cañadell et al[8] described a technique that combined the use of an allograft shell and a free vascularized fibular flap for intercalary reconstruction of the lower limb. This technique provided good primary stability and protected the flap from excessive mechanical stress, and thus simultaneously provided both mechanical and biological strength. Moreover, vascularized fibular flaps for the reconstruction of bone defects can fuse with the host bone and result in remodeling and hypertrophy in response to mechanical stress[13]. However, the high level of expertise required for microsurgery techniques limits their use. Further, the considerable operation time required for reconstruction could delay the recovery of patients and the postoperative chemotherapy regimen. Studies have shown that non-vascularized fibular grafts have the ability of remodeling and integrating with the host bone as well[14,15]. However, other studies have reported a high nonunion rate and the limitations of using lengthy grafts, and the recommended length is less than 12 cm according to previous work[16].
Recently, the Masquelet technique has become popular for the reconstruction of massive bone defects after tumor resection[17,18]. Biau et al[19] reported that they had successfully used the Masquelet technique in a case of Ewing sarcoma with a 16 cm bone defect after tumor resection. According to them, this technique is also reliable for massive intercalary reconstruction after tumor resection. Villemagne et al[20] carried out a retrospective study on the use of the Masquelet technique in treating bone defects after surgical resection of malignant bone tumors in 12 children. They concluded that the Masquelet technique does not require very high microsurgical skills and carries a lower rate of infection. However, they also mentioned that the two invasive surgeries are drawbacks to the use of this technique. Some studies have explored the possibility of a one-stage procedure for the Masquelet technique in non-infectious cases, and some of them have reported better outcomes and lower morbidity[21].
In our previous studies, we used an antibiotic-loaded PMMA construct combined with an autograft for reconstruction of the thoracic and lumbar spine. There was no sign of infection, and bone-graft union was achieved in all patients; the functional results were also satisfactory[5,6]. We have therefore extended this method for biological reconstruction after en bloc resection in the presented case. In order to ensure better support and reduce the operating time, we used a 20 cm free non-vascularized fibula flap. Unlike the methods mentioned in other studies, we did not remove the periosteum of the fibular graft for the sake of better callus formation. As observed in our previous studies, the PMMA construct adequately mimicked the effect of induced membrane using the Masquelet technique, and therefore facilitated the revascularization of the fibular flap with the intact periosteum. Six months after surgery, bone union was clearly confirmed in both the proximal and distal femur by CT scanning. Moreover, considerable bone formation was observed around the PMMA construct. No signs of fracture of the fibular flap nor breakage of the inner fixation were observed up to the 28 mo follow-up. However, unlike reports in the literature, hypertrophy of the fibular flap could not be observed at the end of follow-up. The possible reason is that the PMMA construct and inner fixation have some stress-shielding effect on it. A long-term follow-up is needed to make this clarification.
Epiphyseal distraction can be easily applied to obtain a safe margin in cases of osteosarcoma around the knee where the epiphysis is not involved. Hybrid reconstruction with an antibiotic-loaded PMMA construct combined with a free non-vascularized fibular graft has several advantages, such as easy manufacturing, less time-consuming, lower chances of infection and better bone union. Our case report provides an alternative technique for biological reconstruction after joint-sparing surgery in osteosarcoma patients.
We would like to thank Mrs. Jing Wan (the wife of Dr. Jun Wan) for her hard work in language editing and selfless support for this study.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anand A, Bergen CJ, Vosoughi AR S-Editor: Zhang L L-Editor: Filipodia E-Editor: Qi LL
| 1. | Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res. 1980;106-120. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 890] [Cited by in F6Publishing: 704] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 2. | Wong KC, Kumta SM. Joint-preserving tumor resection and reconstruction using image-guided computer navigation. Clin Orthop Relat Res. 2013;471:762-773. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 72] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 3. | Li J, Wang Z, Pei GX, Guo Z. Biological reconstruction using massive bone allograft with intramedullary vascularized fibular flap after intercalary resection of humeral malignancy. J Surg Oncol. 2011;104:244-249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Capanna R, Bufalini C, Campanacci M. A new technique for reconstructions of large metadiaphyseal bone defects: a combined graft (allograft shell plus vascularized fibula). Orthop Traumatol. 1993;2:159-177. [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 116] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Jun W, Yi-Jun K, Fei C, Guo-Hua L, Dong-Zhe L. Application of an antibiotic crescent-shaped polymethylmethacrylate strut in thoracic vertebral tuberculosis. Turk Neurosurg. 2013;23:107-112. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Jun W, Yi-Jun K, Fei C. Application of a crescent-shaped PMMA strut in anterior spinal reconstruction of thoracolumbar and lumbar burst fractures: a new technique. Turk Neurosurg. 2012;22:161-166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Cho HS, Oh JH, Han I, Kim HS. The outcomes of navigation-assisted bone tumour surgery: minimum three-year follow-up. J Bone Joint Surg Br. 2012;94:1414-1420. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 8. | Cañadell J, Forriol F, Cara JA. Removal of metaphyseal bone tumours with preservation of the epiphysis. Physeal distraction before excision. J Bone Joint Surg Br. 1994;76:127-132. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 92] [Cited by in F6Publishing: 75] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Betz M, Dumont CE, Fuchs B, Exner GU. Physeal distraction for joint preservation in malignant metaphyseal bone tumors in children. Clin Orthop Relat Res. 2012;470:1749-1754. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Liu W, He HB, Zhang C, Liu YP, Wan J. Distraction-suppression effect on osteosarcoma. Med Hypotheses. 2018;121:4-5. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Wan J, Ling L, Zhang XS, Li ZH. Femoral bone transport by a monolateral external fixator with or without the use of intramedullary nail: a single-department retrospective study. Eur J Orthop Surg Traumatol. 2013;23:457-464. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Li Z, Zhang X, Duan L, Chen X. Distraction osteogenesis technique using an intramedullary nail and a monolateral external fixator in the reconstruction of massive postosteomyelitis skeletal defects of the femur. Can J Surg. 2009;52:103-111. [PubMed] [Cited in This Article: ] |
| 13. | Houdek MT, Wagner ER, Stans AA, Shin AY, Bishop AT, Sim FH, Moran SL. What Is the Outcome of Allograft and Intramedullary Free Fibula (Capanna Technique) in Pediatric and Adolescent Patients With Bone Tumors? Clin Orthop Relat Res. 2016;474:660-668. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 59] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 14. | Schuh R, Panotopoulos J, Puchner SE, Willegger M, Hobusch GM, Windhager R, Funovics PT. Vascularised or non-vascularised autologous fibular grafting for the reconstruction of a diaphyseal bone defect after resection of a musculoskeletal tumour. Bone Joint J. 2014;96-B:1258-1263. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 15. | Akiyama T, Clark JC, Miki Y, Choong PF. The non-vascularised fibular graft: a simple and successful method of reconstruction of the pelvic ring after internal hemipelvectomy. J Bone Joint Surg Br. 2010;92:999-1005. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Lenze U, Kasal S, Hefti F, Krieg AH. Non-vascularised fibula grafts for reconstruction of segmental and hemicortical bone defects following meta- /diaphyseal tumour resection at the extremities. BMC Musculoskelet Disord. 2017;18:289. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 17. | Masquelet AC, Begue T. The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am. 2010;41:27-37; table of contents. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 508] [Cited by in F6Publishing: 481] [Article Influence: 34.4] [Reference Citation Analysis (0)] |
| 18. | Gouron R, Deroussen F, Plancq MC, Collet LM. Bone defect reconstruction in children using the induced membrane technique: a series of 14 cases. Orthop Traumatol Surg Res. 2013;99:837-843. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | Biau DJ, Pannier S, Masquelet AC, Glorion C. Case report: reconstruction of a 16-cm diaphyseal defect after Ewing's resection in a child. Clin Orthop Relat Res. 2009;467:572-577. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 78] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 20. | Villemagne T, Bonnard C, Accadbled F, L'kaissi M, de Billy B, Sales de Gauzy J. Intercalary segmental reconstruction of long bones after malignant bone tumor resection using primary methyl methacrylate cement spacer interposition and secondary bone grafting: the induced membrane technique. J Pediatr Orthop. 2011;31:570-576. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 68] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 21. | Jiang N, Qin CH, Ma YF, Wang L, Yu B. Possibility of one-stage surgery to reconstruct bone defects using the modified Masquelet technique with degradable calcium sulfate as a cement spacer: A case report and hypothesis. Biomed Rep. 2016;4:374-378. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |