Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2894
Peer-review started: May 8, 2019
First decision: June 17, 2019
Revised: July 23, 2019
Accepted: July 27, 2019
Article in press: July 27, 2019
Published online: September 26, 2019
Entrapment of the temporal horn (ETH) is a rare pathologic condition. It is a kind of focal hydrocephalus caused by obstruction of flow pathway of cerebrospinal fluid. It is caused by various conditions, but ETH secondary to postoperative gamma-knife radiosurgery (GKS) is extremely rare.
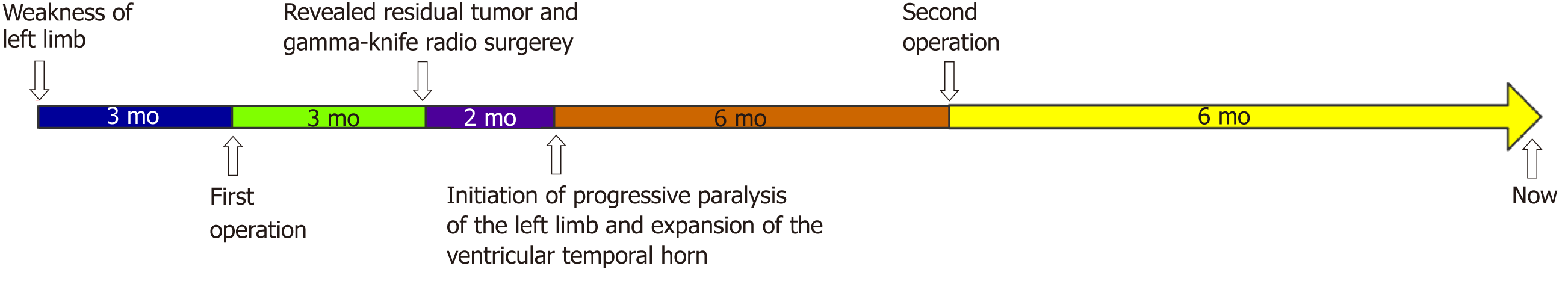
A 52-year old previously healthy woman underwent resection of a large intraventricular meningioma. A small fragment of residual tumor with no obvious enlargement of the temporal horn was observed 3 mo after surgery, and she was referred for GKS. Two months after GKS, she complained of headache and progressive paralysis of the left limb. Magnetic resonance imaging revealed enlargement of the temporal horn. There was a second procedure to resect the residual tumor 8 mo after GKS. After the second procedure, she recovered smoothly. As of the date of this writing, she has remained in good condition.
This case reminds us that ETH should be considered in the treatment of intraventricular meningiomas, especially before GKS.
Core tip: Entrapment of the temporal horn (ETH) is a rare pathologic condition. Here we present a case of ETH secondary to postoperative gamma-knife radiosurgery (GKS) in intraventricular meningioma. A 52-year old women received gamma knife therapy 3 mo after first operation of intraventricular meningioma due to residual tumor. Then, ETH occurred 2 mo after GKS. A second operation to resect the residual tumor 8 mo after GKS was performed and the patient recovered smoothly. This case reminded us that ETH should be considered in the treatment of intraventricular meningiomas, especially before GKS.
- Citation: Liu J, Long SR, Li GY. Entrapment of the temporal horn secondary to postoperative gamma-knife radiosurgery in intraventricular meningioma: A case report. World J Clin Cases 2019; 7(18): 2894-2898
- URL: https://www.wjgnet.com/2307-8960/full/v7/i18/2894.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i18.2894
Entrapment of the temporal horn (ETH) is characterized by dilation of the temporal horn of the lateral ventricle, caused by cerebrospinal fluid (CSF) obstruction at the trigone level. It is secondary to several pathological conditions, including infection[1], intraventricular hematoma[2], parasitic infection[3], arteriovenous malformation[4], and intraventricular tumors[5]. Most reported cases of ETH were secondary to these pathological conditions. However, gamma-knife radiosurgery (GKS) also can lead to ETH, although this situation has been rarely reported. Here we report the first case of ETH secondary to postoperative GKS.
A 52-year old woman was admitted to our hospital with a complaint of weakness of the left limb and lethargy.
She felt weakness of the left limb 3 mo before admission and became lethargy 3 d before admission.
No past illness was complained by the patient.
On admission, the patient was somnolent. Physical examination showed weakness of the left limbs and bilateral papilledema. After admission, her condition deteriorated rapidly.
No obvious abnormality was revealed in laboratory examinations.
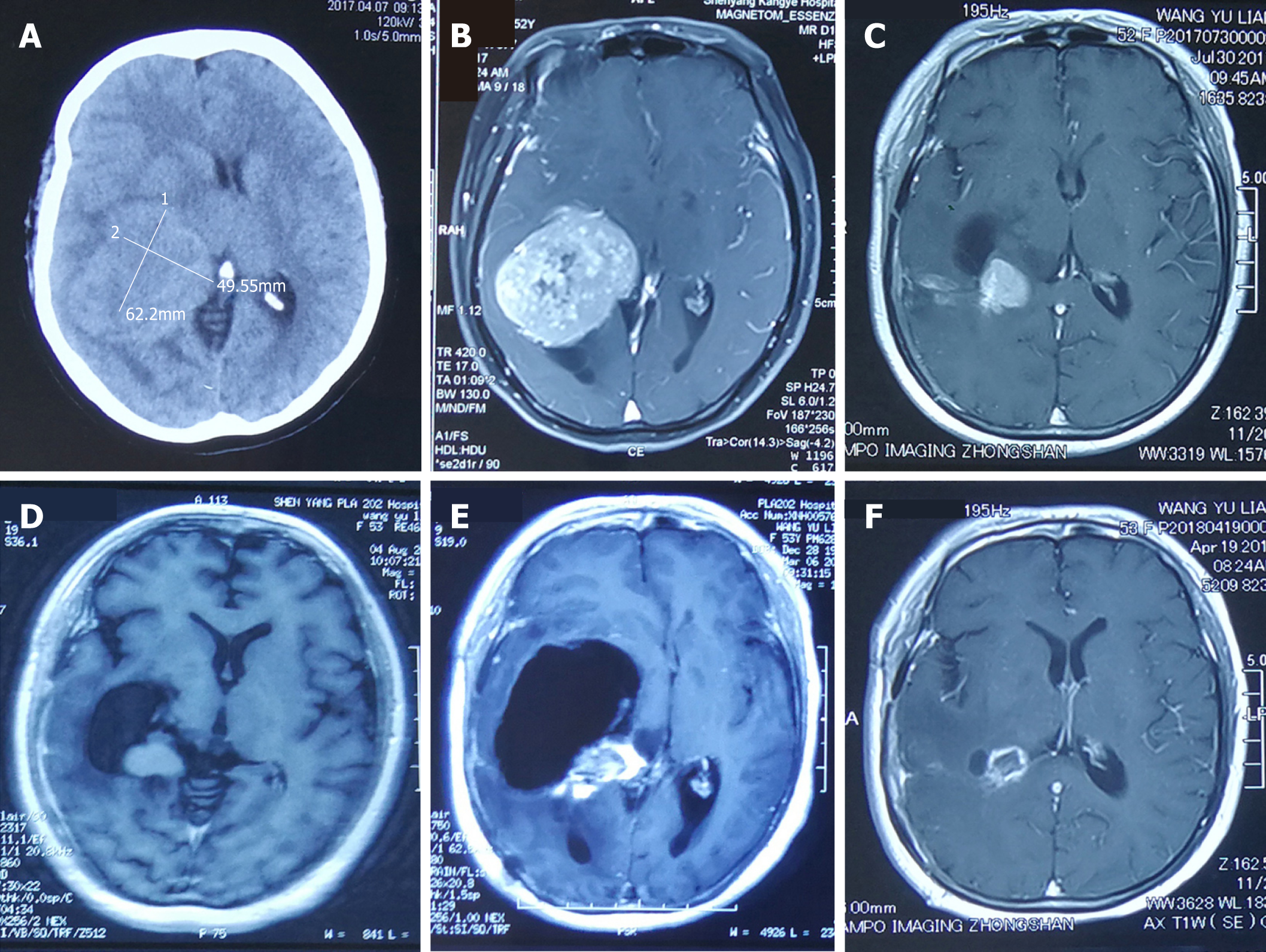
A computed tomography (CT) scan showed a homodensity lesion in the right trigon of the ventricle, and magnetic resonance imaging (MRI) showed a lesion with homogenous enhancement in the right trigone of the ventricle. No enlargement of the ventricle was observed (Figure 1).
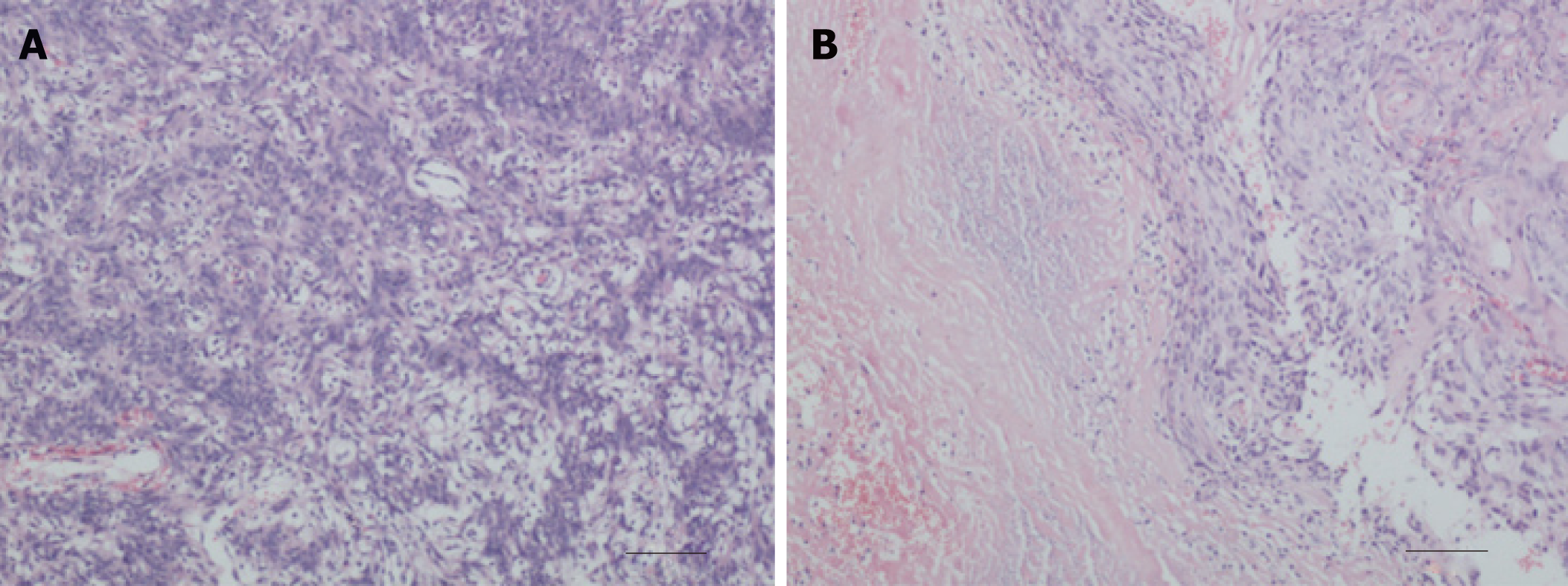
She underwent intraventricular meningioma resection under general anesthesia via a transcortical approach. A small piece of tumor remained during the operation because of unstable vital signs. Postoperative pathological diagnosis confirmed meningioma. The patient recovered smoothly after surgery and symptoms disappeared gradually. A follow-up at 3 mo after surgery revealed residual tumor. She was in good condition at the time. She was then referred for GKS. Radiosurgery was performed with 32 Gy of five central points and a marginal dose of 16 Gy to 50% isodose curve, which lasted 2325 s. Two months after GKS, she developed a headache and progressive paralysis of the left limb. Follow-up magnetic resonance imaging revealed progressive expansion of the ventricular temporal horn. She then underwent a second operation 11 mo after the first procedure. At the second operation, the residual tumor was resected completely and the choroid plexus was coagulated (Figure 2).
After the second operation, she recovered rapidly with disappearance of headache and hemiparesis. She has remained well until the most recent follow-up 9 mo after the second surgery (Figure 3).
Recently, ETH after operation of the trigone meningioma has been brought into focus, which was seldom discovered before. As the development of imaging plays an important role in neurosurgery[6,7], dilation of the ventricle can be monitored by CT and MRI. In fact, dilation of the temporal horn of the lateral ventricle is not rare after surgery for intraventricular lesions[8], especially for trigone meningioma[9]. However, most are asymptomatic or can be treated with conservative therapy. Only few cases require surgical intervention because of progressive intracranial hypertension and mass effect caused by dilated temporal horn. Several factors were reported to be related to the occurrence of postoperative ETH, including meningitis after surgery, neurologic deficits after operation, and inappropriate ventricular drainage[5]. In our case, a large trigon meningioma was resected. None of the factors mentioned above were present in our case. Despite a small residual piece of tumor, no substantial dilation of the temporal horn occurred 3 mo after surgery. Nevertheless, two months after GKS, she suffered from headache and gradual symptom worsening. In our case, no high-risk factor related with ETH was observed; therefore, we speculated that ETH in our case was secondary to radiation damage induced by GKS. Radiation led to brain damage, including to the ventricular wall; this may have led to occlusion of CSF flow. Radiation-associated ETH was reported in only a girl with a diffuse parietoccipital AVM who underwent GKS[10]. GKS also can cause tumor edema and increase tumor volume, leading to ETH. To the best of our knowledge, ETH secondary to GKS in trigone meningioma has not been reported previously.
There are many methods to manage ETH, including V-P shunt[2], endoscopic temporal ventriculocisternostomy[11,12], frontal-to-temporal horn shunt[13], and temporal horn to prepontine cistern shunt[14]. In this case, resection of residual tumor was performed, and the patient recovered smoothly thereafter.
In conclusion, to the best of our knowledge, this is the first case of ETH after GKS in an intraventricular meningioma. This case reminds us that ETH should be considered when treating intraventricular meningiomas, especially before GKS.
Manuscript source: Unsolicited Manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El-Razek AA, Jiang B, Sotelo J S-Editor: Cui LJ L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Tsugane R, Shimoda M, Yamaguchi T, Yamamoto I, Sato O. Entrapment of the temporal horn: a form of focal non-communicating hydrocephalus caused by intraventricular block of cerebrospinal fluid flow--report of two cases. Neurol Med Chir (Tokyo). 1992;32:210-214. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Maurice-Williams RS, Choksey M. Entrapment of the temporal horn: a form of focal obstructive hydrocephalus. J Neurol Neurosurg Psychiatry. 1986;49:238-242. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 41] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Kamali NI, Huda MF, Srivastava VK. Intraventricular hydatid cyst causing entrapped temporal horn syndrome: Case report and review of literature. Trop Parasitol. 2011;1:113-115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Paredes I, Orduna J, Fustero D, Salgado JA, de Diego JM, de Mesa FG. Endoscopic temporal ventriculocisternostomy for the management of temporal horn entrapment: report of 4 cases. J Neurosurg. 2017;126:298-303. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Wang Y, Lin Z, Li Z, Zhao M, Hu M, Zhang H, Chen X, Jiang Z. The Incidence and Risk Factors of Postoperative Entrapped Temporal Horn in Trigone Meningiomas. World Neurosurg. 2016;90:511-517. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Abdel Razek AAK, El-Serougy L, Abdelsalam M, Gaballa G, Talaat M. Differentiation of Primary Central Nervous System Lymphoma From Glioblastoma: Quantitative Analysis Using Arterial Spin Labeling and Diffusion Tensor Imaging. World Neurosurg. 2019;123:e303-e309. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 7. | Razek AAKA, El-Serougy L, Abdelsalam M, Gaballa G, Talaat M. Differentiation of residual/recurrent gliomas from postradiation necrosis with arterial spin labeling and diffusion tensor magnetic resonance imaging-derived metrics. Neuroradiology. 2018;60:169-177. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 84] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 8. | Zhang B, Wang X, Li C, Li Z. Neuroendoscopic Fenestration for Entrapped Temporal Horn After Surgery: Report of 3 Cases. World Neurosurg. 2018;112:77-80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Ma J, Cheng L, Wang G, Lin S. Surgical management of meningioma of the trigone area of the lateral ventricle. World Neurosurg. 2014;82:757-769. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 10. | Yeon JY, Shin HJ, Kim JS, Hong SC, Lee JI. Clinico-radiological outcomes following gamma knife radiosurgery for pediatric arteriovenous malformations. Childs Nerv Syst. 2011;27:1109-1119. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Krähenbühl AK, Baldauf J, Gaab MR, Schroeder HW. Endoscopic temporal ventriculocisternostomy: an option for the treatment of trapped temporal horns. J Neurosurg Pediatr. 2013;11:568-574. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Arenas-Ruiz JA, Martinez-Maldonado H, Gonzalez-Carranza V, Torres-García S, Chico-Ponce de Leon F. Endoscopic ventriculo-cisterno-ventricular approach in the treatment of bilateral trapped temporal horn related to fungal infection in a child: case report and review of the literature. Childs Nerv Syst. 2018;34:1593-1597. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Hervey-Jumper SL, Ziewacz JE, Heth JA, Sullivan SE. Frontal-to-temporal horn shunt as treatment for temporal horn entrapment. J Neurosurg. 2010;112:410-413. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 3] [Reference Citation Analysis (0)] |
| 14. | Chen CC, Kasper EM, Zinn PO, Warnke PC. Management of entrapped temporal horn by temporal horn to prepontine cistern shunting. World Neurosurg. 2013;79:404.e7-404.10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |