© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Uhthoff’s phenomenon as the initial symptom in
neuromyelitis optica spectrum disorders: a case report
H Liang, MD1; C Xu, MD2; J Xu, MD3
1 Department of Neurology, Hainan General Hospital, Hainan Affiliated Hospital of Hainan Medical University, Hainan Province Clinical Medical Center and Hainan Academician Innovation Platform, Haikou, China
2 Department of Urology, Hainan General Hospital, Hainan Affiliated Hospital of Hainan Medical University, Haikou, China
3 Department of Neurology, The National Clinical Research Center for Mental Disorders and Beijing Key Laboratory of Mental Disorders, Beijing Anding Hospital, Capital Medical University, Beijing, China
Corresponding author: Dr J Xu (xujiyi22@163.com)
Case report
A 20-year-old male presented with a history of
dysuria after taking a hot bath 13 days prior to
visiting a urology clinic. A urinary tract infection was
diagnosed. He reported difficulty urinating about
3 minutes after taking a hot bath, accompanied by
a distended and painful bladder. The symptoms
gradually resolved after about 30 minutes but
dysuria worsened over time, especially when he took
a hot bath (about 40°C, a shower or bath). Eventually
his symptoms began to persist even 12 hours after
bathing and a urinary catheter was inserted after
5 days. In the meantime, he developed numbness in
his back and limb weakness and was transferred to
the neurology department. The patient’s medical,
family and medication history were otherwise
unremarkable.
The patient’s temperature (36.6°C), blood
pressure (108/72 mmHg), and pulse (76 beats/min)
were normal as was respiratory, cardiovascular, and
abdominal examination. Neurological examination
revealed bilateral knee and ankle reflexes (notedly
hyperactive), limb muscle strength (slightly
decreased), and sensory system examination was
normal. His pupils were isochoric and the papillary
light reflex was present. No sensitive focal signs were
detected and Babinski sign was negative.
His laboratory test results (complete blood
count, blood sugar, lipid, hepatic, renal function,
antinuclear antibodies, antiphospholipid antibodies,
antineutrophil cytoplasmic antibodies, and
rheumatoid factor) were normal. Routine urinalysis
revealed a red blood cell count of 16/μL and
white blood cell count of 16/μL. Examination of a
cerebrospinal fluid sample showed a white blood
cell level of 16 × 106 L. The oligoclonal bands in
cerebrospinal fluid and serum were negative, and
anti–aquaporin-4 antibodies in the serum were
positive.
Cerebral magnetic resonance imaging (MRI)
revealed abnormal signals in the right brachium pontis, brainstem, and left parietal lobe, with no
contrast enhancement. The whole spinal MRI scan
displayed abnormal signals from C6 to T1 (Fig).
The patient was diagnosed with neuromyelitis
optica spectrum disorder (NMOSD). Treatment
included intravenous immunoglobulin (0.4 g/kg/d)
and glucocorticoids (1000 mg intravenous
methylprednisolone for 5 days, then changed to oral
methylprednisolone 60 mg for 1 week). He recovered
gradually; 5 days later, the catheter was removed and
he could urinate freely. The numbness in his back
and limb weakness resolved gradually. Five months
later, the abnormal signals on the MRI scan were
no longer present, and there was no recurrence at
1-year follow-up.
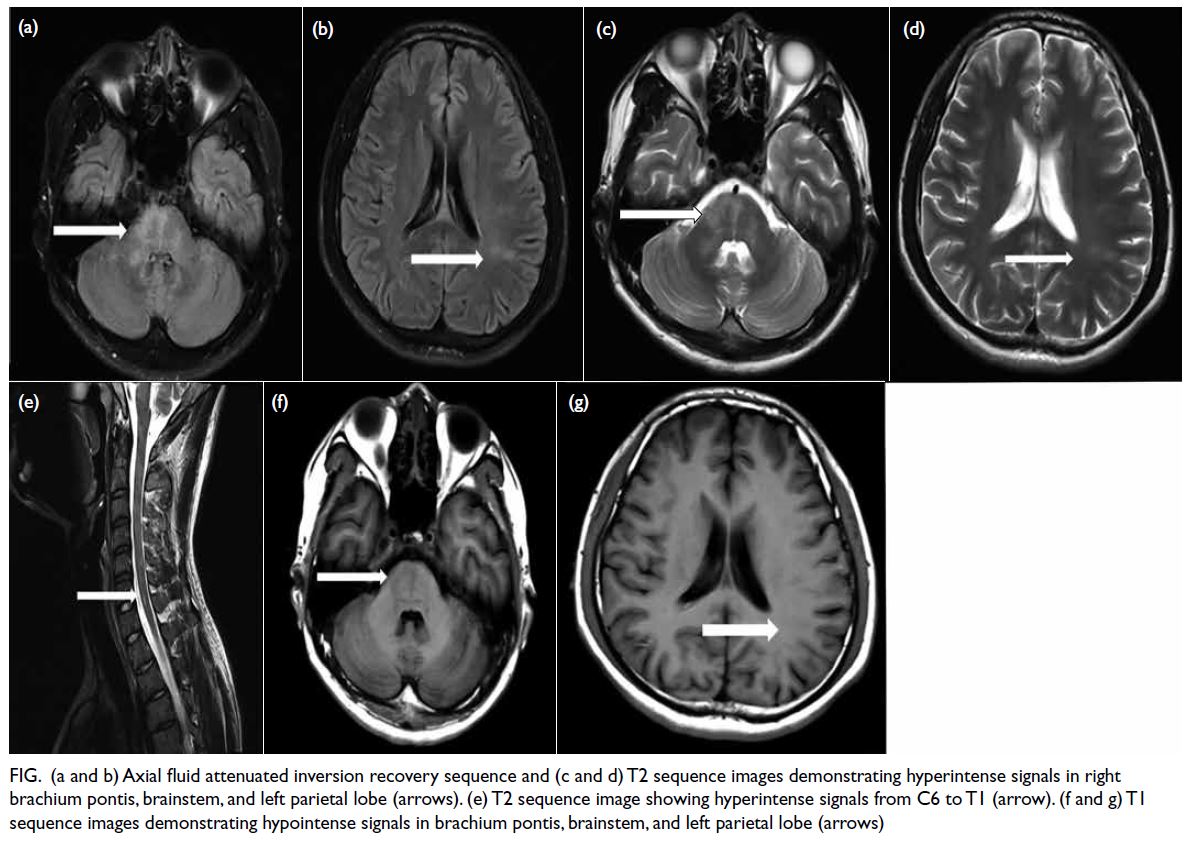
Figure. (a and b) Axial fluid attenuated inversion recovery sequence and (c and d) T2 sequence images demonstrating hyperintense signals in right brachium pontis, brainstem, and left parietal lobe (arrows). (e) T2 sequence image showing hyperintense signals from C6 to T1 (arrow). (f and g) T1 sequence images demonstrating hypointense signals in brachium pontis, brainstem, and left parietal lobe (arrows)
Discussion
German professor Wilhelm Uhthoff described
the phenomenon of transitory visual disturbance
in 1890 in patients with multiple sclerosis (MS)
occurring after physical exercise and an increase
in body temperature. In 1961, G Ricklefs named
this phenomenon Uhthoff’s phenomenon (UP),1
as Uhthoff observed the appearance of reversible
optic symptoms induced by an increase in body
temperature in four of 100 patients with MS and
described it as the ‘prominent deterioration of
visual acuity during physical exercise and exhausting
activity’.2 Subsequent observations revealed that
the physiological mechanism of visual dysfunction
during heat exposure was the same as that of
various other neurological symptoms experienced
by MS patients. When Uhthoff researched the
phenomenon, he considered exercise to be the only
aetiology and ignored the importance of elevated
body temperature. In 1950, the hot bath test was
developed based on this phenomenon and was
used to diagnose MS. Nonetheless because of the
non-specific nature and potential complications of
the hot bath test, it was replaced in 1980 by other
diagnostic tests such as cerebrospinal fluid analysis and MRI. The transient worsening of neurological
function due to heat exposure affects the cognitive
and physical functions of MS patients and affects
their daily life and functional capacity. As this
worsening differs to a real relapse or exacerbation of
MS, it is necessary to understand this phenomenon
and its pathophysiology so that suitable treatment
can be administered.
Uhthoff’s phenomenon is most commonly
observed in individuals with MS but can also
occur in those with NMOSDs.3 To date, the exact
mechanisms of UP have remained unclear; however
they likely involve a combination of structural and
physiological changes within the demyelinated
axons in the central nervous system that occur in the
presence of a raised core body temperature.4 Factors
including exercise, taking a hot bath or shower, fever,
exposure to sun, menstrual cycle, psychological
stress, and hot meals may worsen the symptoms in
MS or NMOSD.5
A study reported UP as the first manifestation
of MS in an adult male who presented with blurred
vision after performing intense exercise in the fitness room.6 Another study reported three episodes of
oscillopsia that occurred while a 17-year-old man
participated in intense sports in summer (which was
interpreted as recurrent UP); the man was finally
diagnosed with radiologically isolated syndrome.7
To date, no studies have reported UP as the initial
symptom in individuals with NMOSDs.
The longitudinally extensive spinal cord
lesions and anti–aquaporin-4 antibodies in the
serum of our patient supported the diagnosis of
NMOSD. Our patient first presented with dysuria
after taking a hot bath and was considered a case of
UP. Loss of the myelin sheath is the primary cause
of UP: an elevation in the core body temperature
in the context of axonal demyelination results in
pore closure of voltage-gated sodium channels,
thus compromising action potential depolarisation.
There are a variety of heat stressors (fever, hot
bath, premenstrual period, physical exercise) and
clinical manifestations of UP depending on where
demyelinating plaques are located.8 In our patient,
the rise in core body temperature during the hot
bath could have aggravated the spinal lesion that impaired the micturition centre and led to dysuria.
The patient initially visited the urology clinic
and was misdiagnosed with urinary infection; due
to the development of additional symptoms, he was
suspected of having spinal cord lesions. Overall,
urologists as well as neurologists should be aware
of the phenomenon to avoid misdiagnosing diseases
related to UP.
Author contributions
Concept or design: H Liang, C Xu.
Acquisition of data: H Liang, C Xu.
Analysis or interpretation of data: J Xu.
Drafting of the manuscript: H Liang, C Xu.
Critical revision of the manuscript for important intellectual content: J Xu.
Acquisition of data: H Liang, C Xu.
Analysis or interpretation of data: J Xu.
Drafting of the manuscript: H Liang, C Xu.
Critical revision of the manuscript for important intellectual content: J Xu.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
The authors declare no conflict of interest.
Funding/support
This study was supported by Natural Science Foundation Fund of Hainan Province (Ref No.: 823QN343) and Hainan
General Hospital Qingnian Fund (Ref No.: QN202002). The
funders had no role in study design, data collection/analysis/interpretation or manuscript preparation.
Ethics approval
Written informed consent was obtained from the patient for the publication of this case report and any accompanying
images.
References
1. Fraser CL, Davagnanam I, Radon M, Plant GT. The time course and phenotype of Uhthoff phenomenon following
optic neuritis. Mult Scler 2012;18:1042-4. Crossref
2. Pearce JM. Early observations on optic neuritis and Uhthoff’s sign. Eur Neurol 2010;63:243-7. Crossref
3. Park K, Tanaka K, Tanaka M. Uhthoff’s phenomenon in multiple sclerosis and neuromyelitis optica. Eur Neurol
2014;72:153-6. Crossref
4. Jacquerye P, Poma JF, Dupuis M. Uhthoff’s phenomenon as the presenting symptom of multiple sclerosis (MS). Acta Neurol Belg 2017;117:953-4. Crossref
5. Panginikkod S, Rayi A, Rocha Cabrero F, Rukmangadachar LA. Uhthoff Phenomenon. Treasure Island (FL): StatPearls Publishing; 2019.
6. Santos-Bueso E, Viera-Peláez D, Asorey-García A, Porta-Etessam J, Vinuesa-Silva JM, García-Sánchez J. Uhthoff’s phenomenon as the first manifestation of multiple sclerosis in an adult male. J Fr Ophtalmol 2016;39:e123-4. Crossref
7. Baroncini D, Zaffaroni M, Minonzio G, et al. Uhthoff’s phenomena and brain MRI suggesting demyelinating lesions: RIS or CIS? A case report. J Neurol Sci 2014;345:262-4. Crossref
8. Frohman TC, Davis SL, Beh S, Greenberg BM, Remington G, Frohman EM. Uhthoff’s phenomena in MS—clinical features and pathophysiology. Nat Rev Neurol 2013;9:535-40. Crossref

