Abstract
Background
Patients undergoing macroscopically curative resection for distal cholangiocarcinoma (DCC) have high recurrence rates and poor prognoses. This study aimed to investigate the impact of surgical margin status on survival and recurrence after resection of DCC, specifically focusing on microscopic residual tumor (R1) and its relationship to local recurrence.
Patients and Methods
This was a retrospective analysis of patients who had undergone pancreaticoduodenectomy (PD) for DCC between 2005 and 2021. Surgical margin was classified as R0, R1cis (positive bile duct margin with carcinoma in situ), and R1inv (positive bile duct margin with an invasive subepithelial component and/or positive radial margin).
Results
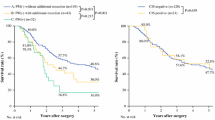
In total, 29 of 133 patients (21.8%) had R1cis and 23 (17.3%) R1inv. The 5-year overall survival (OS) for R0 (55.7%) did not differ significantly from that for R1cis/R1inv (47.4%/33.6%, respectively). The 5-year recurrence-free survival (RFS) for R0 was significantly longer than that for R1inv (50.1% vs. 17.4%, p = 0.003), whereas RFS did not differ significantly between those with R0 and R1cis. R1cis/R1inv status was not an independent predictor of OS and RFS in multivariate analysis. Cumulative incidence of isolated distant recurrence was significantly higher for R1cis/R1inv than for R0 (p = 0.0343/p = 0.0226, respectively), whereas surgical margin status was not significantly associated with rates of local or local plus distant recurrence.
Conclusions
Surgical margin status does not significantly impact OS and RFS in patients undergoing PD for DCC following precise preoperative imaging evaluation. Additionally, R1 status is significantly linked to higher isolated distant recurrence rather than local recurrence, highlighting the importance of multidisciplinary therapy.





Similar content being viewed by others
References
Banales JM, Marin JJG, Lamarca A, et al. Cholangiocarcinoma 2020: the next horizon in mechanisms and management. Nat Rev Gastroenterol Hepatol. 2020;17(9):557–88.
Amin MB, Edge SB, Greene FL, et al editors. AJCC cancer staging manual. 8th edn. Springer; 2017.
Murakami Y, Uemura K, Hayashidani Y, et al. Prognostic significance of lymph node metastasis and surgical margin status for distal cholangiocarcinoma. J Surg Oncol. 2007;95(3):207–12.
Choi SB, Park SW, Kim KS, Choi JS, Lee WJ. The survival outcome and prognostic factors for middle and distal bile duct cancer following surgical resection. J Surg Oncol. 2009;99(6):335–42.
Yasukawa K, Shimizu A, Motoyama H, et al. Impact of remnant carcinoma in situ at the ductal stump on long-term outcomes in patients with distal cholangiocarcinoma. World J Surg. 2021;45(1):291–301.
Nakagohri T, Takahashi S, Ei S, et al. Prognostic impact of margin status in distal cholangiocarcinoma. World J Surg. 2023;47(4):1034–41.
Courtin-Tanguy L, Rayar M, Bergeat D, et al. The true prognosis of resected distal cholangiocarcinoma. J Surg Oncol. 2016;113(5):575–80.
De Oliveira ML, Cunningham SC, Cameron JL, et al. Thirty-one-year experience with 564 patients at a single institution. Ann Surg. 2007;245(5):755–62.
Ishihara S, Horiguchi A, Miyakawa S, Endo I, Miyazaki M, Takada T. Biliary tract cancer registry in Japan from 2008 to 2013. J Hepatobiliary Pancreat Sci. 2016;23(3):149–57.
Park Y, Hwang DW, Kim JH, et al. Prognostic comparison of the longitudinal margin status in distal bile duct cancer: R0 on first bile duct resection versus R0 after additional resection. J Hepatobiliary Pancreat Sci. 2019;26(5):169–78.
Chen Z, Yu B, Bai J, et al. The impact of intraoperative frozen section on resection margin status and survival of patients underwent pancreatoduodenectomy for distal cholangiocarcinoma. Front Oncol. 2021;11:650585.
Igami T, Nagino M, Oda K, et al. Clinicopathologic study of cholangiocarcinoma with superficial spread. Ann Surg. 2009;249(2):296–302.
Wakai T, Shirai Y, Moroda T, Yokoyama N, Hatakeyama K. Impact of ductal resection margin status on long-term survival in patients undergoing resection for extrahepatic cholangiocarcinoma. Cancer. 2005;103(6):1210–6.
Todoroki T, Kawamoto T, Koike N, Fukao K, Shoda J, Takahashi H. Treatment strategy for patients with middle and lower third bile duct cancer. Br J Surg. 2001;88(3):364–70.
Nakanishi Y, Kondo S, Zen Y, et al. Impact of residual in situ carcinoma on postoperative survival in 125 patients with extrahepatic bile duct carcinoma. J Hepatobiliary Pancreat Sci. 2010;17(2):166–73.
Sallinen V, Sirén J, Mäkisalo H, et al. Differences in prognostic factors and recurrence patterns after curative-intent resection of perihilar and distal cholangiocarcinomas. Scand J Surg. 2020;109(3):219–27.
Komaya K, Ebata T, Shirai K, et al. Recurrence after resection with curative intent for distal cholangiocarcinoma. Br J Surg. 2017;104(4):426–33.
Vogel I, Kalthoff H, Henne-Bruns D, Kremer B. Detection and prognostic impact of disseminated tumor cells in pancreatic carcinoma. Pancreatology. 2002;2(2):79–88.
Hernandez J, Mullinax J, Clark W, et al. Survival after pancreaticoduodenectomy is not improved by extending resections to achieve negative margins. Ann Surg. 2009;250(1):76–80.
Pedrazzoli S, DiCarlo V, Dionigi R, The Lymphadenectomy Study, et al. Standard versus extended lymphadenectomy associated with pancreatoduodenectomy in the surgical treatment of adenocarcinoma of the head of the pancreas a multicenter, prospective, randomized study. Ann Surg. 1998;228(4):508–17.
Farnell MB, Pearson RK, Sarr MG, et al. A prospective randomized trial comparing standard pancreatoduodenectomy with pancreatoduodenectomy with extended lymphadenectomy in resectable pancreatic head adenocarcinoma. Surgery. 2005;138(4):618–28 (discussion 628–30).
Yeo CJ, Cameron JL, Lillemoe KD, et al. Pancreaticoduodenectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma, part 2: randomized controlled trial evaluating survival, morbidity, and mortality. Ann Surg. 2002;236(3):355–68.
Nimura Y, Nagino M, Takao S, et al. Standard versus extended lymphadenectomy in radical pancreatoduodenectomy for ductal adenocarcinoma of the head of the pancreas: long-term results of a Japanese multicenter randomized controlled trial. J Hepatobiliary Pancreat Sci. 2012;19(3):230–41.
Ojima H, Kanai Y, Iwasaki M, et al. Intraductal carcinoma component as a favorable prognostic factor in biliary tract carcinoma. Cancer Sci. 2009;100(1):62–70.
Miyazaki M, Ohtsuka M, Miyakawa S, et al. Classification of biliary tract cancers established by the Japanese Society of Hepato-Biliary-Pancreatic Surgery: 3(rd) English edition. J Hepatobiliary Pancreat Sci. 2015;22(3):181–96.
Roa JC, Adsay NV, Arola J, Tsui WM, Zen Y, et al. Carcinoma of the extrahepatic bile ducts. In: F Carneiro, et al., editors. World Health Organization classification of tumours 5th edition digestive system tumours. IARC Press; 2019.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC Cancer Staging Manual. 7th edn. Springer; 2010.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
Nakachi K, Ikeda M, Konishi M, et al. Adjuvant S-1 compared with observation in resected biliary tract cancer (JCOG1202, ASCOT): a multicentre, open-label, randomised, controlled, phase 3 trial. Lancet. 2023;401(10372):195–203.
Miwa S, Kobayashi A, Akahane Y, et al. Is major hepatectomy with pancreatoduodenectomy justified for advanced biliary malignancy? J Hepatobiliary Pancreat Surg. 2007;14(2):136–41.
Kaneoka Y, Yamaguchi A, Isogai M. Hepatopancreatoduodenectomy: its suitability for bile duct cancer versus gallbladder cancer. J Hepatobiliary Pancreat Surg. 2007;14(2):142–8.
Ebata T, Yokoyama Y, Igami T, et al. Hepatopancreatoduodenectomy for cholangiocarcinoma: a single-center review of 85 consecutive patients. Ann Surg. 2012;256(2):297–305.
Wakai T, Shirai Y, Tsuchiya Y, Nomura T, Akazawa K, Hatakeyama K. Combined major hepatectomy and pancreaticoduodenectomy for locally advanced biliary carcinoma: long-term results. World J Surg. 2008;32(6):1067–74.
Lim CS, Jang JY, Lee SE, Kang MJ, Kim SW. Reappraisal of hepatopancreatoduodenectomy as a treatment modality for bile duct and gallbladder cancer. J Gastrointest Surg. 2012;16(5):1012–8.
Primrose JN, Fox RP, Palmer DH, et al. Capecitabine compared with observation in resected biliary tract cancer (BILCAP): a randomised, controlled, multicentre, phase 3 study. Lancet Oncol. 2019;20(5):663–73.
Kobayashi S, Nagano H, Tomokuni A, et al. A prospective, randomized phase II study of adjuvant gemcitabine versus S-1 after major hepatectomy for biliary tract cancer (KHBO 1208): Kansai Hepato-Biliary Oncology Group. Ann Surg. 2019;270(2):230–7.
Kobayashi S, Ikeda M, Nakachi K, et al. A multicenter survey on eligibility for a randomized phase III trial of adjuvant chemotherapy for resected biliary tract cancer (JCOG1202, ASCOT). Ann Surg Oncol. 2023;30(12):7331–7.
Versteijne E, van Dam JL, Suker M, et al. Neoadjuvant chemoradiotherapy versus upfront surgery for resectable and borderline resectable pancreatic cancer: long-term results of the dutch randomized PREOPANC trial. J Clin Oncol. 2022;40(11):1220–30.
Goetze TO, Bechstein WO, Bankstahl US, et al. Neoadjuvant chemotherapy with gemcitabine plus cisplatin followed by radical liver resection versus immediate radical liver resection alone with or without adjuvant chemotherapy in incidentally detected gallbladder carcinoma after simple cholecystectomy or in front of radical resection of BTC (ICC/ECC)—A phase III study of the German registry of incidental gallbladder carcinoma platform (GR)—The AIO/CALGP/ACO-GAIN-trial. BMC Cancer. 2020;20(1):122.
Nara S, Ioka T, Ogawa G, et al. Randomized multicenter phase III trial of neoadjuvant gemcitabine + cisplatin + S-1 (GCS) versus surgery first for resectable biliary tract cancer (JCOG1920: NABICAT). J Clin Oncol. 2023;41(4_suppl):TPS621–TPS621.
Acknowledgments
We thank Dr. Trish Reynolds, MBBS, FRACP, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Umino, R., Nara, S., Mizui, T. et al. Impact of Surgical Margin Status on Survival and Recurrence After Pancreaticoduodenectomy for Distal Cholangiocarcinoma: Is Microscopic Residual Tumor (R1) Associated with Higher Rates of Local Recurrence?. Ann Surg Oncol (2024). https://doi.org/10.1245/s10434-024-15313-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1245/s10434-024-15313-w