Abstract
Background
In women ≥ 70 years of age with T1N0 hormone receptor-positive (HR+)/human epidermal growth factor receptor 2-negative (HER2−) breast cancer, breast surgery type and omission of axillary surgery or radiation therapy (RT) do not impact overall survival. Although frailty and life expectancy ideally factor into therapy decisions, their impact on therapy receipt is unclear. We sought to identify trends in and factors associated with locoregional therapy type by frailty and life expectancy.
Methods
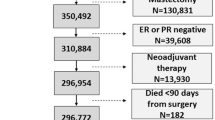
Women ≥ 70 years of age with T1N0 HR+/HER2− breast cancer diagnosed in the Surveillance, Epidemiology, and End Results (SEER)-Medicare database between 2010 and 2015 were stratified by validated claims-based frailty and life expectancy measures. Therapy trends over time by regimen intensity (‘high intensity’: lumpectomy + axillary surgery + RT, or mastectomy + axillary surgery; ‘moderate intensity’: lumpectomy + RT, lumpectomy + axillary surgery, or mastectomy only; or ‘low intensity’: lumpectomy only) were analyzed. Factors associated with therapy type were identified using generalized linear mixed models.
Results
Of 16,188 women, 21.8% were frail, 22.2% had a life expectancy < 5 years, and only 12.3% fulfilled both criteria. In frail women with a life expectancy < 5 years, high-intensity regimens decreased significantly (48.8–31.2%; p < 0.001) over the study period, although in 2015, 30% still received a high-intensity regimen. In adjusted analyses, frailty and life expectancy < 5 years were not associated with breast surgery type but were associated with a lower likelihood of axillary surgery (frailty: odds ratio [OR] 0.86, 95% confidence interval [CI] 0.76–0.96; life expectancy < 5 years: OR 0.22, 95% CI 0.20–0.25). Life expectancy < 5 years was also associated with a lower likelihood of RT receipt in breast-conserving surgery patients (OR 0.30, 95% CI 0.27–0.34).
Conclusions
Rates of high-intensity therapy are decreasing but overtreatment persists in this population. Continued efforts aimed at appropriate de-escalation of locoregional therapy are needed.


Similar content being viewed by others
Data Availability
These data will not be shared as this dataset is widely used/publicly available.
References
Schonberg MA, Marcantonio ER, Li D, Silliman RA, Ngo L, McCarthy EP. Breast cancer among the oldest old: tumor characteristics, treatment choices, and survival. J Clin Oncol. 2010;28(12):2038–45.
Smith BD, Jiang J, McLaughlin SS, et al. Improvement in breast cancer outcomes over time: are older women missing out? J Clin Oncol. 2011;29(35):4647–53.
Van Leeuwen BL, Rosenkranz KM, Feng LL, et al. The effect of under-treatment of breast cancer in women 80 years of age and older. Crit Rev Oncol Hematol. 2011;79(3):315–20.
Owusu C, Buist DS, Field TS, et al. Predictors of tamoxifen discontinuation among older women with estrogen receptor-positive breast cancer. J Clin Oncol. 2008;26(4):549–55.
Partridge AH, LaFountain A, Mayer E, Taylor BS, Winer E, Asnis-Alibozek A. Adherence to initial adjuvant anastrozole therapy among women with early-stage breast cancer. J Clin Oncol. 2008;26(4):556–62.
Ojala K, Meretoja TJ, Mattson J, Leidenius MHK. Surgical treatment and prognosis of breast cancer in elderly—a population-based study. Eur J Surg Oncol. 2019;45(6):956–62.
Derks MG, Bastiaannet E, van de Water W, et al. Impact of age on breast cancer mortality and competing causes of death at 10 years follow-up in the adjuvant TEAM trial. Eur J Cancer. 2018;99:1–8.
Shumway DA, Griffith KA, Sabel MS, et al. Surgeon and radiation oncologist views on omission of adjuvant radiotherapy for older women with early-stage breast cancer. Ann Surg Oncol. 2017;24(12):3518–26.
Katz SJ, Jagsi R, Morrow M. Reducing overtreatment of cancer with precision medicine: just what the doctor ordered. JAMA. 2018;319(11):1091–2.
Katz SJ, Morrow M. Addressing overtreatment in breast cancer: the doctors’ dilemma. Cancer. 2013;119(20):3584–8.
van Dongen JA, Voogd AC, Fentiman IS, et al. Long-term results of a randomized trial comparing breast-conserving therapy with mastectomy: European Organization for Research and Treatment of Cancer 10801 trial. J Natl Cancer Inst. 2000;92(14):1143–50.
Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347(16):1233–41.
Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347(16):1227–32.
Martelli G, Boracchi P, Ardoino I, et al. Axillary dissection versus no axillary dissection in older patients with T1N0 breast cancer: 15-year results of a randomized controlled trial. Ann Surg. 2012;256(6):920–4.
Rudenstam CM, Zahrieh D, Forbes JF, et al. Randomized trial comparing axillary clearance versus no axillary clearance in older patients with breast cancer: first results of International Breast Cancer Study Group Trial 10–93. J Clin Oncol. 2006;24(3):337–44.
Hughes KS, Schnaper LA, Bellon JR, et al. Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: long-term follow-up of CALGB 9343. J Clin Oncol. 2013;31(19):2382–7.
Kunkler IH, Williams LJ, Jack WJ, Cameron DA, Dixon JM. Breast-conserving surgery with or without irradiation in women aged 65 years or older with early breast cancer (PRIME II): a randomised controlled trial. Lancet Oncol. 2015;16(3):266–73.
Kunkler IH, Williams LJ, Jack WJL, Cameron DA, Dixon JM. Breast-conserving surgery with or without irradiation in early breast cancer. N Engl J Med. 2023;388(7):585–94.
NCI: SEER-Medicare data fact sheet. Available at https://healthcaredelivery.cancer.gov/seermedicare/overview/. Accessed 3 May 2019.
Kim DH, Schneeweiss S, Glynn RJ, Lipsitz LA, Rockwood K, Avorn J. Measuring frailty in Medicare data: development and validation of a claims-based frailty index. J Gerontol A Biol Sci Med Sci. 2018;73(7):980–7.
Castillo-Angeles M, Cooper Z, Jarman MP, Sturgeon D, Salim A, Havens JM. Association of frailty with morbidity and mortality in emergency general surgery by procedural risk level. JAMA Surg. 2021;156(1):68–74.
Tan A, Kuo YF, Goodwin JS. Predicting life expectancy for community-dwelling older adults from Medicare claims data. Am J Epidemiol. 2013;178(6):974–83.
Klabunde CN, Legler JM, Warren JL, Baldwin LM, Schrag D. A refined comorbidity measurement algorithm for claims-based studies of breast, prostate, colorectal, and lung cancer patients. Ann Epidemiol. 2007;17(8):584–90.
Choosing Wisely. Available at: https://abimfoundation.org/what-we-do/choosing-wisely. Accessed 17 Oct 2019.
National Comprehensive Cancer Network (NCCN) Guidelines. Breast Cancer. Version 2.2023. Available at: https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 22 Feb 2023.
Biganzoli L, Wildiers H, Oakman C, et al. Management of elderly patients with breast cancer: updated recommendations of the International Society of Geriatric Oncology (SIOG) and European Society of Breast Cancer Specialists (EUSOMA). Lancet Oncol. 2012;13(4):e148–60.
Minami CA, Bryan AF, Freedman RA, et al. Assessment of oncologists’ perspectives on omission of sentinel lymph node biopsy in women 70 years and older with early-stage hormone receptor-positive breast cancer. JAMA Netw Open. 2022;5(8):e2228524.
Mohile SG, Dale W, Somerfield MR, et al. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology. J Clin Oncol. 2018;36(22):2326–47.
Raza S, Rudolph JL, Mujahid N, et al. Assessment of frailty and risk of chemotherapy toxicity at a geriatric-oncology multidisciplinary clinic. R I Med J. 2023;106(4):13–8.
Barthelemy P, Heitz D, Mathelin C, et al. Adjuvant chemotherapy in elderly patients with early breast cancer. Impact of age and comprehensive geriatric assessment on tumor board proposals. Crit Rev Oncol Hematol. 2011;79(2):196–204.
Clough-Gorr KM, Stuck AE, Thwin SS, Silliman RA. Older breast cancer survivors: geriatric assessment domains are associated with poor tolerance of treatment adverse effects and predict mortality over 7 years of follow-up. J Clin Oncol. 2010;28(3):380–6.
Orum M, Gregersen M, Jensen K, Meldgaard P, Damsgaard EMS. Frailty status but not age predicts complications in elderly cancer patients: a follow-up study. Acta Oncol. 2018;57(11):1458–66.
Nishijima TF, Shimokawa M, Komoda M, et al. Survival in older Japanese adults with advanced cancer before and after implementation of a geriatric oncology service. JCO Oncol Pract. 2023. https://doi.org/10.1200/OP.22.00842.
Ma M, Peters XD, Zhang LM, et al. Multi-site implementation of an American College of surgeons geriatric surgery quality improvement initiative. J Am Coll Surg. 2023;237(2):171–81.
Sharon CE, Strohl C, Saur NM. Frailty assessment and prehabilitation as part of a perioperative evaluation and planning (PREP) program for patients undergoing colorectal surgery. Clin Colon Rectal Surg. 2023;36(3):184–91.
Deeb AL, Garrity M, Cooper L, Frain LN, Jaklitsch MT, DuMontier C. Implementing 4-meter gait speed as a routine vital sign in a thoracic surgery clinic. J Geriatr Oncol. 2023;14(4):101481.
Minami CA, Cooper Z. The frailty syndrome: a critical issue in geriatric oncology. Crit Care Clin. 2021;37(1):151–74.
Ballinger RS, Mayer KF, Lawrence G, Fallowfield L. Patients’ decision-making in a UK specialist centre with high mastectomy rates. Breast. 2008;17(6):574–9.
Dicks E, Roome R, Chafe J, et al. Factors influencing surgical treatment decisions for breast cancer: a qualitative exploration of surgeon and patient perspectives. Curr Oncol. 2019;26(2):e216–25.
Gollop SJ, Kyle SM, Fancourt MW, Gilkison WT, Mosquera DA. Why Taranaki women choose to have a mastectomy when suitable for breast conservation treatment. ANZ J Surg. 2009;79(9):604–9.
Hamelinck VC, Bastiaannet E, Pieterse AH, et al. A prospective comparison of younger and older patients’ preferences for breast-conserving surgery versus mastectomy in early breast cancer. J Geriatr Oncol. 2018;9(2):170–3.
Collins ED, Moore CP, Clay KF, et al. Can women with early-stage breast cancer make an informed decision for mastectomy? J Clin Oncol. 2009;27(4):519–25.
Greenup RA, Rushing C, Fish L, et al. Financial costs and burden related to decisions for breast cancer surgery. J Oncol Pract. 2019;15(8):e666–76.
Kirby RM, Basit A, Manimaran N. Patient choice significantly affects mastectomy rates in the treatment of breast cancer. Int Semin Surg Oncol. 2008;5:20.
Shinall MC Jr, Arya S, Youk A, et al. Association of preoperative patient frailty and operative stress with postoperative mortality. JAMA Surg. 2020;155(1):e194620.
DuMontier C, Loh KP, Bain PA, et al. Defining undertreatment and overtreatment in older adults with cancer: a scoping literature review. J Clin Oncol. 2020;38(22):2558–69.
Smith BD, Jiang J, Shih YC, et al. Cost and complications of local therapies for early-stage breast cancer. J Natl Cancer Inst. 2016;109(1):djw178.
Goyal S, Chandwani S, Haffty BG, Demissie K. Effect of travel distance and time to radiotherapy on likelihood of receiving mastectomy. Ann Surg Oncol. 2015;22(4):1095–101.
Onega T, Cook A, Kirlin B, et al. The influence of travel time on breast cancer characteristics, receipt of primary therapy, and surveillance mammography. Breast Cancer Res Treat. 2011;129(1):269–75.
Bredbeck BC, Baskin AS, Wang T, et al. Incremental spending associated with low-value treatments in older women with breast cancer. Ann Surg Oncol. 2022;29(2):1051–9.
Morgan JL, George J, Holmes G, et al. Breast cancer surgery in older women: outcomes of the Bridging Age Gap in Breast Cancer study. Br J Surg. 2020;107(11):1468–79.
Sedrak MS, Freedman RA, Cohen HJ, et al. Older adult participation in cancer clinical trials: a systematic review of barriers and interventions. CA Cancer J Clin. 2021;71(1):78–92.
Hind D, Wyld L, Beverley CB, Reed MW. Surgery versus primary endocrine therapy for operable primary breast cancer in elderly women (70 years plus). Cochrane Database Syst Rev. 2006;25(1):CD004272.
Acknowledgment
This research was funded by the American Society of Clinical Oncology Conquer Cancer Foundation (Young Investigator Award in Geriatric Oncology). Mara A. Schonberg’s effort was supported by NIH/NIA K24 (5K24AG071906). Christina A. Minami reports research support (to the institution) from the American Society of Clinical Oncology Conquer Cancer Foundation (Young Investigator Award, 2020–2021), American College of Surgeons (Faculty Research Fellowship, 2020–2022), and a Grant for Early Medical/Surgical Specialists’ Transition to Aging Research (GEMSSTAR). Elizabeth A. Mittendorf acknowledges support as the Rob and Karen Hale Distinguished Chair in Surgical Oncology. This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the National Cancer Institute; Information Management Services (IMS), Inc.; and the SEER Program tumor registries in the creation of the SEER-Medicare database. This project included data from the California Cancer Registry. The collection of cancer incidence data used in this study was supported by the California Department of Public Health pursuant to California Health and Safety Code Section 103885; Centers for Disease Control and Prevention’s (CDC’s) National Program of Cancer Registries, under cooperative agreement 1NU58DP007156; the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program under contract HHSN261201800032I awarded to the University of California, San Francisco, contract HHSN261201800015I awarded to the University of Southern California, and contract HHSN261201800009I awarded to the Public Health Institute. The ideas and opinions expressed herein are those of the authors and do not necessarily reflect the opinions of the State of California, Department of Public Health, the National Cancer Institute, and the CDC, or their contractors and subcontractors.
Funding
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization: CAM; Data curation: CAM, GJ; Formal analysis: CAM, GJ; Funding acquisition: CAM, EAM; Investigation: CAM, GJ, MAS, RAF, TAK, EAM; Methodology: CAM, GJ, MAS, RAF; Project administration: CAM; Resources: CAM; Software: GJ; Visualization: CAM; Writing—original draft: CAM; Writing—review and editing: CAM, GJ, MAS, RAF, TAK, EAM; Supervision: CAM, EAM, TAK; Validation: CAM, GJ; CAM had full access to all the data in the study and takes responsibility for the integrity of the data and accuracy of the data analysis.
Corresponding author
Ethics declarations
Disclosure
Tari A. King reports speaker honoraria and compensated service on the Scientific Advisory Board of Exact Sciences. Elizabeth A. Mittendorf reports compensated service on Scientific Advisory Boards for Astra Zeneca, BioNTech and Merck; uncompensated service on Steering Committees for Bristol Myers Squibb and Roche/Genentech; speakers honoraria and travel support from Merck Sharp & Dohme; and institutional research support from Roche/Genentech (via an SU2C grant) and Gilead. She also reports research funding from Susan Komen for the Cure for which she serves as a Scientific Advisor, and uncompensated participation as a member of the American Society of Clinical Oncology Board of Directors. Christina A. Minami, Ginger Jin, Rachel A. Freedman, and Mara A. Schonberg report no disclosures or conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Minami, C.A., Jin, G., Freedman, R.A. et al. Trends in Locoregional Therapy in Older Women with Early-Stage Hormone Receptor-Positive Breast Cancer by Frailty and Life Expectancy. Ann Surg Oncol 31, 920–930 (2024). https://doi.org/10.1245/s10434-023-14446-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14446-8