Abstract
Background
Breast cancer-related lymphedema (BCRL) is a devastating complication of breast cancer (BC) treatment. The authors hypothesized that identifying subclinical lymphedema (SCL) presents an opportunity to prevent BCRL development. They aimed to assess rates of SCL progression (relative volume change [RVC], 5–10%) to BCRL (RVC, ≥10%) in women undergoing axillary surgery for BC via axillary lymph node dissection (ALND) or sentinel lymph node biopsy (SLNB).
Methods
Patients treated for BC were prospectively screened at preoperative baseline and throughout the follow-up period using the perometer. The cohort was stratified according to nodal surgery (ALND or SLNB) to analyze rates of progression to BCRL.
Results
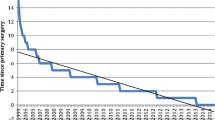
The study cohort included 1790 patients. Of the 1359 patients who underwent SLNB, 331 (24.4%) experienced SCL, with 38 (11.5%) of these patients progressing to BCRL. Of the 431 patients who underwent ALND, 171 (39.7%) experienced SCL, with 67 (39.2%) of these patients progressing to BCRL. Relative to the patients without SCL, those more likely to experience BCRL were the ALND patients with early SCL (< 3 months postoperatively; hazard ratio [HR], 2.60; 95% confidence interval [CI], 1.58–4.27; p = 0.0002) or late SCL (≥3 months postoperatively; HR, 3.14; 95% CI, 1.95–5.05; p < 0.0001) and the SLNB patients with early SCL (HR, 6.75; 95% CI, 3.8–11.98; p < 0.0001 or late SCL (HR, 3.02; 95% CI, 1.65–5.50; p = 0.0003).
Conclusion
The study suggests that patients with SCL after axillary nodal surgery for BC are more likely to progress to BCRL than those who do not experience SCL. This presents a tremendous opportunity for early intervention to prevent BCRL and improve the quality of life for women treated for BC.



Similar content being viewed by others
References
DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14:500–15.
Hespe GE, Nores GG, Huang JJ, Mehrara BJ. Pathophysiology of lymphedema: is there a chance for medication treatment? J Surg Oncol. 2017;115:96–8. https://doi.org/10.1002/jso.24414.
Gillespie TC, Sayegh HE, Brunelle CL, Daniell KM, Taghian AG. Breast cancer-related lymphedema: risk factors, precautionary measures, and treatments. Gland Surg. 2018;7:379–403. https://doi.org/10.21037/gs.2017.11.04.
Fu MR, Rosedale M. Breast cancer survivors’ experiences of lymphedema-related symptoms. J Pain Symptom Manage. 2009;38:849–59. https://doi.org/10.1016/j.jpainsymman.2009.04.030.
Tsai RJ, Dennis LK, Lynch CF, Snetselaar LG, Zamba GKD, Scott-Conner C. The risk of developing arm lymphedema among breast cancer survivors: a meta-analysis of treatment factors. Ann Surg Oncol. 2009;16:1959–72. https://doi.org/10.1245/s10434-009-0452-2.
Rebegea LF, Firescu D, Dumitru M, Anghel R. The incidence and risk factors for occurrence of arm lymphedema after treatment of breast cancer. Chirurgia. 2015;110:33–7.
Shih Y-CT, Xu Y, Cormier JN, et al. Incidence, treatment costs, and complications of lymphedema after breast cancer among women of working age: a 2-year follow-up study. J Clin Oncol. 2009;27:2007–14. https://doi.org/10.1200/JCO.2008.18.3517.
Stout NL, Binkley JM, Schmitz KH, et al. A prospective surveillance model for rehabilitation for women with breast cancer. Cancer. 2012;118(Suppl 8):2191–200. https://doi.org/10.1002/cncr.27476.
Kaufman DI, Shah C, Vicini FA, Rizzi M. Utilization of bioimpedance spectroscopy in the prevention of chronic breast cancer-related lymphedema. Breast Cancer Res Treat. 2017;166:809–15. https://doi.org/10.1007/s10549-017-4451-x.
Ridner SH, Dietrich MS, Cowher MS, et al. A randomized trial evaluating bioimpedance spectroscopy versus tape measurement for the prevention of lymphedema following treatment for breast cancer: interim analysis. Ann Surg Oncol. 2019;26:3250–59. https://doi.org/10.1245/s10434-019-07344-5.
Akita S, Nakamura R, Yamamoto N, et al. Early detection of lymphatic disorder and treatment for lymphedema following breast cancer. Plast Reconstr Surg. 2016;138:192e–202e. https://doi.org/10.1097/PRS.0000000000002337.
Ochalek K, Gradalski T, Partsch H. Preventing early postoperative arm swelling and lymphedema manifestation by compression sleeves after axillary lymph node interventions in breast cancer patients: a randomized controlled trial. J Pain Symptom Manage. 2017;54:346–54. https://doi.org/10.1016/j.jpainsymman.2017.04.014.
Soran A, Ozmen T, McGuire KP, et al. The importance of detection of subclinical lymphedema for the prevention of breast cancer-related clinical lymphedema after axillary lymph node dissection: a prospective observational study. Lymphat Res Biol. 2014;12:289–94. https://doi.org/10.1089/lrb.2014.0035.
National Lymphedema Network Medical Advisory Committee. Position Statement of the National Lymphedema Network: Screening and Measurement for Early Detection of Breast Cancer-Related Lymphedema. 2011.
McLaughlin SA, Staley AC, Vicini F, et al. Considerations for clinicians in the diagnosis, prevention, and treatment of breast cancer-related lymphedema: recommendations from a multidisciplinary expert ASBrS panel: part 1: definitions, assessments, education, and future directions. Ann Surg Oncol. 2017;24:2818–26. https://doi.org/10.1245/s10434-017-5982-4.
Paskett ED, Khakpour N, Moore H, O’Connor T. National Comprehensive Cancer Network Guidelines Version 2.2020: Survivorship: Lymphedema. 2020.
International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: 2016 consensus document of the International Society of Lymphology. Lymphology. 2016;49:170–84. https://doi.org/10.1063/1.4704591.
Brunelle C, Skolny M, Ferguson C, Swaroop M, O’Toole J, Taghian AG. Establishing and sustaining a prospective screening program for breast cancer-related lymphedema at the Massachusetts General Hospital: Lessons Learned. J Pers Med. 2015;5:153–64.
Stanton AW, Northfield JW, Holroyd B, Mortimer PS, Levick JR. Validation of an optoelectronic limb volumeter (Perometer). Lymphology. 1997;30:77–97.
Lee M-J, Boland RA, Czerniec S, Kilbreath SL. Reliability and concurrent validity of the perometer for measuring hand volume in women with and without lymphedema. Lymphat Res Biol. 2011;9:13–8. https://doi.org/10.1089/lrb.2010.0021.
Fu MR, Axelrod D, Cleland CM, et al. Symptom report in detecting breast cancer-related lymphedema. Breast Cancer Targets Ther. 2015;7:345–52. https://doi.org/10.2147/BCTT.S87854.
Armer JM. The problem of post-breast cancer lymphedema: impact and measurement issues. Cancer Invest. 2005;23:76–83.
Specht MC, Miller CL, Russell TA, et al. Defining a threshold for intervention in breast cancer-related lymphedema: what level of arm volume increase predicts progression? Breast Cancer Res Treat. 2013:1–10.
Stout Gergich NL, Pfalzer LA, McGarvey C, Springer B, Gerber LH, Soballe P. Preoperative assessment enables the early diagnosis and successful treatment of lymphedema. Cancer. 2008;112:2809–19. https://doi.org/10.1002/cncr.23494.
Kilgore LJ, Korentager SS, Hangge AN, et al. Reducing breast cancer-related lymphedema (BCRL) through prospective surveillance monitoring using bioimpedance spectroscopy (BIS) and patient-directed self-interventions. Ann Surg Oncol. 2018;25:2948–52. https://doi.org/10.1245/s10434-018-6601-8.
Brown JC, Cheville AL, Tchou JC, Harris SR, Schmitz KH. Prescription and adherence to lymphedema self-care modalities among women with breast cancer-related lymphedema. Support Care Cancer. 2014;22:135–43. https://doi.org/10.1007/s00520-013-1962-9.
Shah C, Arthur DW, Wazer D, Khan A, Ridner S, Vicini F. The impact of early detection and intervention of breast cancer-related lymphedema: a systematic review. Cancer Med. 2016;5:1154–62. https://doi.org/10.1002/cam4.691.
Sayegh HE, Asdourian MS, Swaroop MN, et al. Diagnostic methods, risk factors, prevention, and management of breast cancer-related lymphedema: past, present, and future directions. Curr Breast Cancer Rep. 2017;9:111–21.
Tierney S, Aslam M, Rennie K, Grace P. Infrared optoelectronic volumetry, the ideal way to measure limb volume. Eur J Vasc Endovasc Surg. 1996;12:412–7. https://doi.org/10.1016/S1078-5884(96)80005-0.
Sun F, Skolny MN, Swaroop MN, et al. The need for preoperative baseline arm measurement to accurately quantify breast cancer-related lymphedema. Breast Cancer Res Treat. 2016;157:229–40. https://doi.org/10.1007/s10549-016-3821-0.
Ancukiewicz M, Russell TA, Otoole J, et al. Standardized method for quantification of developing lymphedema in patients treated for breast cancer. Int J Radiat Oncol Biol Phys. 2011;79:1436–43. https://doi.org/10.1016/j.ijrobp.2010.01.001.
O’Toole J, Jammallo LS, Miller CL, Skolny MN, Specht MC, Taghian AG. Screening for breast cancer-related lymphedema: the need for standardization. Oncologist. 2013;18:350–2. https://doi.org/10.1634/theoncologist.2012-0387.
Sun F, Hall A, Tighe MP, et al. Perometry versus simulated circumferential tape measurement for the detection of breast cancer-related lymphedema. Breast Cancer Res Treat. 2018;172:83–91. https://doi.org/10.1007/s10549-018-4902-z.
Ancukiewicz M, Miller CL, Skolny MN, et al. Comparison of relative versus absolute arm size change as criteria for quantifying breast cancer-related lymphedema: the flaws in current studies and need for universal methodology. Breast Cancer Res Treat. 2012;135:145–52. https://doi.org/10.1007/s10549-012-2111-8.
Armer JM, Stewart BR. A comparison of four diagnostic criteria for lymphedema in a post-breast cancer population. Lymphat Res Biol. 2005;3:208–17. https://doi.org/10.1089/lrb.2005.3.208.
Borman P, Yaman A, Yasrebi S, Özdemir O. The importance of awareness and education in patients with breast cancer-related lymphedema. J Cancer Educ. 2017;32:629–33. https://doi.org/10.1007/s13187-016-1026-1.
Sherman KAKL. The role of information sources and objective risk status on lymphedema risk-minimization behaviors in women recently diagnosed with breast cancer. Oncol Nurs Forum. 2011;38:E27-36. https://doi.org/10.1188/11.ONF.E27-E36.
Fu MR, Chen CM, Haber J, Guth AA, Axelrod D. The effect of providing information about lymphedema on the cognitive and symptom outcomes of breast cancer survivors. Ann Surg Oncol. 2010;17:1847–53. https://doi.org/10.1245/s10434-010-0941-3.
Warren LEG, Miller CL, Horick N, et al. The impact of radiation therapy on the risk of lymphedema after treatment for breast cancer: a prospective cohort study. Int J Radiat Oncol Biol Phys. 2014;88:565–71. https://doi.org/10.1016/j.ijrobp.2013.11.232.
Johansson K, Branje E. Arm lymphoedema in a cohort of breast cancer survivors 10 years after diagnosis. Acta Oncol Madr. 2010;49:166–73. https://doi.org/10.3109/02841860903483676.
Johansson K, Ochalek K, Hayes S. Prevention of arm lymphedema through the use of compression sleeves following breast cancer: results from a targeted literature review. Phys Ther Rev. 2020. https://doi.org/10.1080/10833196.2020.1822140.
Foldi E. The treatment of lymphedema. Cancer. 1988; (12 Suppl A):2833–4.
NCCN. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Survivorship.
ISL. The diagnosis and treatment of peripheral lymphedema, . consensus document of the International Society of Lymphology. Lymphology. 2016;2016(49):170–84. https://doi.org/10.1063/1.4704591.
McDuff SGR, Mina AI, Brunelle CL, et al. Timing of lymphedema after treatment for breast cancer: when are patients most at risk? Int J Radiat Oncol Biol Phys. 2019;103:62–70. https://doi.org/10.1016/j.ijrobp.2018.08.036.
Brunelle CL, Roberts SA, Horick NK, et al. Integrating symptoms into the diagnostic criteria for breast cancer-related lymphedema: applying results from a prospective surveillance program. Phys Ther. 2020;100:2186–97.
Yahathugoda C, Weiler MJ, Rao R, et al. Use of a novel portable three-dimensional imaging system to measure limb volume and circumference in patients with filarial lymphedema. Am J Trop Med Hyg. 2017;97:1836–42. https://doi.org/10.4269/ajtmh.17-0504.
Acknowledgment
The project was supported by award no. R01CA139118 (A. G. Taghian) and award no. P50CA08393 (A. G. Taghian) from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health. This program was supported by the Adele McKinnon Research Fund for Breast Cancer-Related Lymphedema, the Heinz Family Foundation, and the Olayan-Xefos Family Fund for Breast Cancer Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Alphonse G. Taghian has been loaned equipment from ImpediMed for use in an investigator-initiated clinical trial. Alphonse G. Taghian is on the Scientific Advisory Board of Puretech Health and is a previous consultant for VisionRT. Both involvements are unrelated to this study. Cheryl L. Brunelle is on the Scientific Advisory Board of Puretech Health. The remaining authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bucci, L.K., Brunelle, C.L., Bernstein, M.C. et al. Subclinical Lymphedema After Treatment for Breast Cancer: Risk of Progression and Considerations for Early Intervention. Ann Surg Oncol 28, 8624–8633 (2021). https://doi.org/10.1245/s10434-021-10173-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10173-0