Abstract
Background
Integration of palliative care services into the surgical treatment plan is important for holistic patient care. We sought to examine the association between patient race/ethnicity and county-level vulnerability relative to patterns of hospice utilization.
Patients and Methods
Medicare Standard Analytic Files were used to identify patients undergoing lung, esophageal, pancreatic, colon, or rectal cancer surgery between 2013 and 2017. Data were merged with the Centers for Disease Control and Prevention’s social vulnerability index (SVI). Logistic regression was utilized to identify factors associated with overall hospice utilization among deceased individuals.
Results
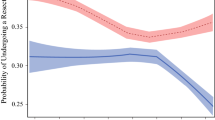
A total of 54,256 Medicare beneficiaries underwent lung (n = 16,645, 30.7%), esophageal (n = 1427, 2.6%), pancreatic (n = 6183, 11.4%), colon (n = 26,827, 49.4%), or rectal (n = 3174, 5.9%) cancer resection. Median patient age was 76 years (IQR 71–82 years), and 28,887 patients (53.2%) were male; the majority of individuals were White (91.1%, n = 49,443), while a smaller subset was Black or Latino (racial/ethnic minority: n = 4813, 8.9%). Overall, 35,416 (65.3%) patients utilized hospice services prior to death. Median SVI was 52.8 [interquartile range (IQR) 30.3–71.2]. White patients were more likely to utilize hospice care compared with minority patients (OR 1.24, 95% CI 1.17–1.31, p < 0.001). Unlike White patients, there was reduced odds of hospice utilization (OR 0.97, 95% CI 0.96–0.99) and early hospice initiation (OR 0.94, 95% CI 0.91–0.97) as SVI increased among minority patients.
Conclusions
Patients residing in counties with high social vulnerability were less likely to be enrolled in hospice care at the time of death, as well as be less likely to initiate hospice care early. The effects of increasing social vulnerability on hospice utilization were more profound among minority patients.



Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30. https://doi.org/10.3322/caac.21590.
Statement on Principles Guiding Care at the End of Life.; 1998.
Paredes AZ, Hyer JM, Tsilimigras DI, et al. Hospice utilization among Medicare beneficiaries dying from pancreatic cancer. J Surg Oncol. 2019;120(4):jso.25623. https://doi.org/10.1002/jso.25623.
Paredes AZ, Hyer JM, Palmer E, Lustberg MB, Pawlik TM. Racial/ethnic disparities in hospice utilization among Medicare beneficiaries dying from pancreatic cancer. J Gastrointest Surg. March 2020:1–7. https://doi.org/10.1007/s11605-020-04568-9.
Olmsted CL, Johnson AM, Kaboli P, Cullen J, Vaughan-Sarrazin MS. Use of palliative care and hospice among surgical and medical specialties in the veterans health administration. In: JAMA Surgery. Vol 149. American Medical Association; 2014:1169–75. https://doi.org/10.1001/jamasurg.2014.2101.
Lilley EJ, Khan KT, Johnston FM, et al. Palliative care interventions for surgical patients a systematic review. JAMA Surg. 2016;151(2):172–83. https://doi.org/10.1001/jamasurg.2015.3625.
Johnson KS. Racial and ethnic disparities in palliative care. J Palliat Med. 2013;16(11):1329–34. https://doi.org/10.1089/jpm.2013.9468.
Cohen LL. Racial/ethnic disparities in hospice care: a systematic review. J Palliat Med. 2008;11(5):763–8. https://doi.org/10.1089/jpm.2007.0216.
Kwak J, Haley WE, Chiriboga DA. Racial differences in hospice use and in-hospital death among medicare and medicaid dual-eligible nursing home residents. Gerontologist. 2008;48(1):32–41. https://doi.org/10.1093/geront/48.1.32.
Fairfield KM, Murray KM, Wierman HR, et al. Disparities in hospice care among older women dying with ovarian cancer. Gynecol Oncol. 2012;125(1):14–8. https://doi.org/10.1016/j.ygyno.2011.11.041.
Greiner KA, Perera S, Ahluwalia JS. Hospice usage by minorities in the last year of life: results from the National Mortality Followback Survey. J Am Geriatr Soc. 2003;51(7):970–8. https://doi.org/10.1046/j.1365-2389.2003.51310.x.
Born W, Greiner KA, Sylvia E, Butler J, Ahluwalia JS. Knowledge, attitudes, and beliefs about end-of-life care among inner-city African Americans and Latinos. J Palliat Med. 2004;7(2):247–56. https://doi.org/10.1089/109662104773709369.
Singh G, Daus G, Allender M, et al. Social determinants of health in the United States: addressing major health inequality trends for the nation, 1935–2016. Int J MCH AIDS. 2017;6(2):139. https://doi.org/10.21106/ijma.236.
Braveman P, Gottlieb L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014;129(SUPPL. 2):19–31. https://doi.org/10.1177/00333549141291s206.
Ludwig J, Sanbonmatsu L, Gennetian L, et al. Neighborhoods, obesity, and diabetes: a randomized social experiment. N Engl J Med. 2011;365(16):1509–19. https://doi.org/10.1056/nejmsa1103216.
Arcaya MC, Tucker-Seeley RD, Kim R, Schnake-Mahl A, So M, Subramanian S V. Research on neighborhood effects on health in the United States: a systematic review of study characteristics. Soc Sci Med. 2016;168:16–29. https://doi.org/10.1016/j.socscimed.2016.08.047.
Kurani SS, McCoy RG, Lampman MA, et al. Association of neighborhood measures of social determinants of health with breast, cervical, and colorectal cancer screening rates in the US Midwest. JAMA Netw open. 2020;3(3):e200618. https://doi.org/10.1001/jamanetworkopen.2020.0618.
WHO | Commission on Social Determinants of Health: final report. WHO. 2017. http://www.who.int/social_determinants/thecommission/finalreport/en/. Accessed 12 August 2020.
Walker RJ, Garacci E, Palatnik A, Ozieh MN, Egede LE. The longitudinal influence of social determinants of health on glycemic control in elderly adults with diabetes. Diabetes Care. 2020;43(4):759–66. https://doi.org/10.2337/dc19-1586.
Walker RJ, Smalls BL, Campbell JA, Strom Williams JL, Egede LE. Impact of social determinants of health on outcomes for type 2 diabetes: a systematic review. Endocrine. 2014;47(1):29–48. https://doi.org/10.1007/s12020-014-0195-0.
Kaufman-Shriqui V, O’Campo P, Misir V, et al. Neighbourhood-level deprivation indices and postpartum women’s health: Results from the Community Child Health Network (CCHN) multi-site study. Health Qual Life Outcomes. 2020;18(1). https://doi.org/10.1186/s12955-020-1275-x.
Walker RJ, Strom Williams J, Egede LE. Influence of race, ethnicity and social determinants of health on diabetes outcomes. Am J Med Sci. 2016;351(4):366–73. https://doi.org/10.1016/j.amjms.2016.01.008.
Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible: the neighborhood atlas. N Engl J Med. 2018;378(26):2456–8. https://doi.org/10.1056/nejmp1802313.
The Social Vulnerability Index (SVI): Fact Sheet | CDC. https://svi.cdc.gov/factsheet.html. Accessed 15 August 2020.
Fairfield KM, Black AW, Ziller EC, et al. Area Deprivation Index and rurality in relation to lung cancer prevalence and mortality in a rural state. JNCI Cancer Spectr. 2020;4(4). https://doi.org/10.1093/jncics/pkaa011.
Diaz A, Chavarin D, Paredes AZ, Tsilimigras DI, Pawlik TM. Association of neighborhood characteristics with utilization of high-volume hospitals among patients undergoing high-risk cancer surgery. Ann Surg Oncol. 2020. https://doi.org/10.1245/s10434-020-08860-5.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9. https://doi.org/10.1097/01.mlr.0000182534.19832.83.
Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–82. https://doi.org/10.1093/aje/kwq433.
Enomoto LM, Schaefer EW, Goldenberg D, Mackley H, Koch WM, Hollenbeak CS. The cost of hospice services in terminally ill patients with head and neck cancer. In: JAMA Otolaryngology Head and Neck Surgery. Vol 141. American Medical Association; 2015:1066–74. https://doi.org/10.1001/jamaoto.2015.2162.
Wachterman MW, Hailpern SM, Keating NL, Tamura MK, O’Hare AM. Association between hospice length of stay, health care utilization, and medicare costs at the end of life among patients who received maintenance hemodialysis. JAMA Intern Med. 2018;178(6):792–9. https://doi.org/10.1001/jamainternmed.2018.0256.
Social Determinants of Health | Healthy People 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. Accessed 19 August 2020.
Closing the Gap in a Generation Health Equity through Action on the Social Determinants of Health Commission on Social Determinants of Health FINAL REPORT Closing the Gap in a Generation Contents.; 2008.
Carmichael H, Moore A, Steward L, Velopulos CG. Disparities in emergent versus elective surgery: comparing measures of neighborhood social vulnerability. J Surg Res. 2020;256:397–403. https://doi.org/10.1016/j.jss.2020.07.002.
Carmichael H, Moore A, Steward L, Velopulos CG. Using the Social Vulnerability Index to examine local disparities in emergent and elective cholecystectomy. J Surg Res. 2019;243:160–4. https://doi.org/10.1016/j.jss.2019.05.022.
Diaz A, Barmash E, Azap R, Paredes AZ, Hyer JM, Pawlik TM. Association of county-level social vulnerability with elective versus non-elective colorectal surgery. J Gastrointest Surg. 2020. https://doi.org/10.1007/s11605-020-04768-3.
Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–42. https://doi.org/10.1056/nejmoa1000678.
Taylor DH, Bull J, Zhong X, Samsa G, Abernethy AP. The effect of palliative care on patient functioning. J Palliat Med. 2013;16(10):1227–31. https://doi.org/10.1089/jpm.2013.0040.
Teno JM, Gozalo PL, Lee IC, et al. Does hospice improve quality of care for persons dying from dementia? J Am Geriatr Soc. 2011;59(8):1531–6. https://doi.org/10.1111/j.1532-5415.2011.03505.x.
Enomoto LM, Schaefer EW, Goldenberg D, Mackley H, Koch WM, Hollenbeak CS. The cost of hospice services in terminally ill patients with head and neck cancer. In: JAMA Otolaryngology - Head and Neck Surgery. Vol 141. American Medical Association; 2015:1066–74. https://doi.org/10.1001/jamaoto.2015.2162.
Cheraghlou S, Gahbauer EA, Leo-Summers L, Stabenau HF, Chaudhry SI, Gill TM. Restricting Symptoms before and after admission to hospice. Am J Med. 2016;129(7):754.e7–754.e15. https://doi.org/10.1016/j.amjmed.2016.02.017.
Facts and Figures | 2018 EDITION Rganization.
Connor SR, Pyenson B, Fitch K, Spence C, Iwasaki K. Comparing hospice and nonhospice patient survival among patients who die within a three-year window. J Pain Symptom Manage. 2007;33(3):238–46. https://doi.org/10.1016/j.jpainsymman.2006.10.010.
Wilkie DJ, Ezenwa MO. Pain and symptom management in palliative care and at end of life. Nurs Outlook. 2012;60(6):357–64. https://doi.org/10.1016/j.outlook.2012.08.002.
Riley GF, Lubitz JD. Long-term trends in medicare payments in the last year of life. Health Serv Res. 2010;45(2):565–76. https://doi.org/10.1111/j.1475-6773.2010.01082.x.
Olearczyk B. Health Care 2020: The critical role of palliative/hospice care in the reengineering of health care delivery. Am J Med. 2016;129(9):e197. https://doi.org/10.1016/j.amjmed.2015.11.037.
Palliative Care in Oncology | ASCO. https://www.asco.org/practice-policy/cancer-care-initiatives/palliative-care-oncology. Accessed 15 August 2020.
Haines KL, Jung HS, Zens T, Turner S, Warner-Hillard C, Agarwal S. Barriers to hospice care in trauma patients: the disparities in end-of-life care. Am J Hosp Palliat Med. 2018;35(8):1081–4. https://doi.org/10.1177/1049909117753377.
Barnato AE, Anthony DL, Skinner J, Gallagher PM, Fisher ES. Racial and ethnic differences in preferences for end-of-life treatment. J Gen Intern Med. 2009;24(6):695–701. https://doi.org/10.1007/s11606-009-0952-6.
Flanagan BE, Hallisey EJ, Adams E, Lavery A. Measuring community vulnerability to natural and anthropogenic hazards: The Centers for Disease Control and Prevention’s social vulnerability index. J Environ Health. 2018;80(10):34–6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7179070/. Accessed 19 August 2020.
Health Equity Measures - Social Vulnerability: Department of Health. https://health.ri.gov/data/healthequity/socialvulnerability/. Accessed 19 August 2020.
Kind AJH, Jencks S, Brock J, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: A retrospective cohort study. Ann Intern Med. 2014;161(11):765–74. https://doi.org/10.7326/m13-2946.
Mehta B, Goodman S, Ho K, Parks M, Ibrahim SA. Community Deprivation Index and discharge destination after elective hip replacement. Arthritis Care Res (Hoboken). January 2020. https://doi.org/10.1002/acr.24145.
Hu J, Kind AJH, Nerenz D. Area Deprivation Index predicts readmission risk at an urban teaching hospital. Am J Med Qual. 2018;33(5):493–501. https://doi.org/10.1177/1062860617753063.
Cagle JG, LaMantia MA, Williams SW, Pek J, Edwards LJ. Predictors of preference for hospice care among diverse older adults. Am J Hosp Palliat Med. 2016;33(6):574–84. https://doi.org/10.1177/1049909115593936.
Orlovic M, Smith K, Mossialos E. Racial and ethnic differences in end-of-life care in the United States: evidence from the Health and Retirement Study (HRS). SSM - Popul Heal. 2019;7:100331. https://doi.org/10.1016/j.ssmph.2018.100331.
Bakitas MA, Tosteson TD, Li Z, et al. Early versus delayed initiation of concurrent palliative oncology care: Patient outcomes in the ENABLE III randomized controlled trial. J Clin Oncol. 2015;33(13):1438–45. https://doi.org/10.1200/jco.2014.58.6362.
Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet. 2014;383(9930):1721–30. https://doi.org/10.1016/s0140-6736(13)62416-2.
Qureshi D, Tanuseputro P, Perez R, Pond GR, Seow HY. Early initiation of palliative care is associated with reduced late-life acute-hospital use: a population-based retrospective cohort study. Palliat Med. 2019;33(2):150–9. https://doi.org/10.1177/0269216318815794.
Tavakkoli A, Singal AG, Waljee AK, et al. Racial disparities and trends in pancreatic cancer incidence and mortality in the United States. Clin Gastroenterol Hepatol. 2020;18(1):171–8.e10. https://doi.org/10.1016/j.cgh.2019.05.059.
Newman LA, Roff NK, Weinberg AD. Cancer clinical trials accrual: Missed opportunities to address disparities and missed opportunities to improve outcomes for all. Ann Surg Oncol. 2008;15(7):1818–9. https://doi.org/10.1245/s10434-008-9869-2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abbas, A., Madison Hyer, J. & Pawlik, T.M. Race/Ethnicity and County-Level Social Vulnerability Impact Hospice Utilization Among Patients Undergoing Cancer Surgery. Ann Surg Oncol 28, 1918–1926 (2021). https://doi.org/10.1245/s10434-020-09227-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09227-6