Abstract
Background
Outcomes of women with gynecologic cancer are superior when treated by gynecologic oncologists. The National Surgical Quality Improvement Program (NSQIP) began identifying gynecologic surgeon subspecialty in 2014. We sought to identify characteristics and outcomes of women treated by general gynecologists in comparison with women treated by gynecologic oncologists.
Patients and Methods
Patients undergoing hysterectomy for gynecologic malignancy in 2014 and 2015 were abstracted from the NSQIP database. Patient characteristics, morbidities, surgeon specialty, and operative outcomes were captured.
Results
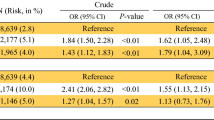
7271 hysterectomies were performed for malignant disease, and 669 were performed by generalists. In comparison with generalists, gynecologic oncologists operated on patients who were older (P < 0.001), more likely to be White [odds ratio (OR) 2.1, P < 0.001], had disseminated cancer (OR 3.1, P < 0.001), had ascites (OR 2.6, P < 0.001), and were classified as American Society of Anesthesiologists (ASA) class ≥ 3 (OR 1.7, P < 0.001). Gynecologic oncologists were also more likely to have hospital readmissions (OR 1.7, P = 0.004) and perform lymph node dissections for endometrial cancer (OR 2.2, P < 0.001). On multivariable analysis, older age [adjusted OR (aOR) 1.0, P = 0.021], White race (aOR 2.0, P < 0.001), presence of disseminated cancer (aOR 2.5, P < 0.001), presence of ascites (aOR 1.8, P = 0.036), and ASA class ≥ 3 (aOR 1.6, P < 0.001) remained independent predictive factors for having a gynecologic oncology surgeon.
Conclusions
The majority of gynecologic cancer cases are performed by gynecologic oncologists. Generalists are more likely to operate on minority patients and patients with fewer comorbidities. Further efforts to ensure access to specialized cancer care for all patients are needed.

Similar content being viewed by others
References
Practice bulletin no. 149: endometrial cancer. Obstet Gynecol. 2015;125(4):1006–26.
Practice bulletin no. 174: evaluation and management of adnexal masses. Obstet Gynecol. 2016;128(5)e210–26.
Bristow RE, et al. Adherence to treatment guidelines for ovarian cancer as a measure of quality care. Obstet Gynecol. 2013;121(6):1226–34.
Bristow RE, et al. Impact of surgeon and hospital ovarian cancer surgical case volume on in-hospital mortality and related short-term outcomes. Gynecol Oncol. 2009;115(3):334–8.
National Comprehensive Cancer Network. Cervical Cancer (Version 1.2018). January 7, 2018; https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf.
Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. 2009;105(2):103–4.
Stewart SL, et al. The effect of gynecologic oncologist availability on ovarian cancer mortality. World J Obstet Gynecol 2014;3(2):71–7.
Wallace AH, et al. Projecting the need for gynecologic oncologists for the next 40 years. Obstet Gynecol. 2010;116(6):1366–72.
Chan JK, et al. Influence of gynecologic oncologists on the survival of patients with endometrial cancer. J Clin Oncol. 2011;29(7):832–8.
Chan JK, et al. Influence of the gynecologic oncologist on the survival of ovarian cancer patients. Obstet Gynecol. 2007;109(6):1342–50.
Wright JD, et al. Patterns of specialty-based referral and perioperative outcomes for women with endometrial cancer undergoing hysterectomy. Obstet Gynecol. 2017;130(1):81–90.
National Cancer Institute. Cancer Stats Facts: Ovarian Cancer. Cited 2017 May 1; https://seer.cancer.gov/statfacts/html/ovary.html.
National Cancer Institute. Cancer Stat Facts: Cervix Uteri Cancer. Cited 2017 May 1; https://seer.cancer.gov/statfacts/html/cervix.html.
National Cancer Institute. Cancer Stat Facts: Endometrial Cancer. Cited 2017 May 1; https://seer.cancer.gov/statfacts/html/corp.html.
American Society of Anesthesiologists. ASA Physical Status Classification System. Cited 2017 May 2; https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system.
American Hospital Association. Fast Facts on US Hospitals. Cited 2017 May 3; http://www.aha.org/research/rc/stat-studies/fast-facts.shtml.
Murphy M, Alavi K, Maykel J. Working with existing databases. Clin Colon Rectal Surg. 2013;26(1):5–11.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1): 5–29.
Chatterjee S. et al. Disparities in gynecological malignancies. Front Oncol. 6:36.
Kohler BA, et al. Annual report to the nation on the status of cancer, 1975–2011, featuring incidence of breast cancer subtypes by race/ethnicity, poverty, and state. J Natl Cancer Inst. 2015;107(6):djv048.
GoffBA, et al. Predictors of comprehensive surgical treatment in patients with ovarian cancer. Cancer. 2007;109(10):2031–42.
Wright J, et al. Variability in chemotherapy delivery for elderly women with advanced stage ovarian cancer and its impact on survival. Br J Cancer. 2008;98(7):1197–203.
Bristow RE, et al. Disparities in ovarian cancer care quality and survival according to race and socioeconomic status. J Natl Cancer Inst. 2013;105(11):823–32.
Mukherjee D, et al. Disparities in access to neuro-oncologic care in the United States. Arch Surg. 2010;145(3):247–53.
Morris AM et al. Racial disparities in late survival after rectal cancer surgery. J Am Coll Surg. 2006;203(6): 787–94.
Pollack CE, et al. Racial disparities in changing to a high-volume urologist among men with localized prostate cancer. Med Care. 2011;49(11):999–1006.
Graboyes EM, et al. Adherence to National Comprehensive Cancer Network guidelines for time to initiation of postoperative radiation therapy for patients with head and neck cancer. Cancer. 2017;123(14):2651–2660.
Hamel LM, et al. Barriers to clinical trial enrollment in racial and ethnic minority patients with cancer. Cancer Control. 2016. 23(4): 327–337.
Roland PY, et al. The benefits of a gynecologic oncologist: a pattern of care study for endometrial cancer treatment. Gynecol Oncol. 2004;93(1):125–30.
Yokoyama Y, et al. Indispensability of pelvic and paraaortic lymphadenectomy in endometrial cancers. Gynecol Oncol. 1997;64(3):411–7.
Steinberg SM, et al. Comparison of risk adjustment methodologies in surgical quality improvement. Surgery. 2008;144(4):662–7 (discussion 662–7).
Shalowitz DI, et al. Teleoncology for gynecologic cancers. Gynecol Oncol. 2015;139(1): 172–7.
Dafny, L. Hospital industry consolidation–still more to come? N Engl J Med. 2014;370(3):198–9.
Disclosure
The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors. All authors declare that they have no conflicts of interest related to this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ramzan, A.A., Behbakht, K., Corr, B.R. et al. Minority Race Predicts Treatment by Non-gynecologic Oncologists in Women with Gynecologic Cancer. Ann Surg Oncol 25, 3685–3691 (2018). https://doi.org/10.1245/s10434-018-6694-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6694-0