Abstract
Background
Cancer recurrence is a critically important outcome to patients and providers. However, no publicly available cancer registry data contain recurrence information. The National Cancer Data Base (NCDB) collects recurrence data; however, this information is not provided to researchers because of completeness and accuracy concerns. Our objective was to examine completeness of cancer recurrence information in the NCDB.
Methods
Stage I–III thyroid/colon/melanoma/pancreas/breast cancers diagnosed in 2002–2005 were identified. Recurrence status, recurrence type, and recurrence date were evaluated for data completeness. Patient, tumor, and hospital factors were examined using generalized linear mixed models. Pseudo-R 2 statistics estimated the relative contribution of patient and hospital factors.
Results
Of 702,144 patients with thyroid/colon/melanoma/pancreas/breast cancers treated in 1405 hospitals, recurrence information was incomplete in 21.5/24.0/20.2/34.8/18.2 % of patients, respectively. On average, hospitals had incomplete recurrence information on 56.7–66.7 % of their patients. Patients with incomplete information had more comorbidities, a higher cancer stage, non-private insurance, and lived farther from the hospital. Hospitals with the poorest collection were larger tertiary hospitals serving higher-income patients. However, these patients and hospital factors explained less than 3 %, while unexplained hospital variation accounted for the largest part of the observed variation (%ΔR 2 = 84 %).
Conclusions
The majority of hospitals report incomplete recurrence information for more than half of their patients. The presence of incomplete recurrence information was largely dependent on undefined hospital factors, rather than patient or tumor characteristics. Attempts to improve cancer recurrence information should focus on hospital operational and process factors surrounding how the hospital tumor registries collect recurrence data.

Similar content being viewed by others
References
National Cancer Data Base (NCDB). Available at: http://www.facs.org/cancer/ncdb/. Accessed 8 July 2013.
Surveillance Epidemiology and End Results (SEER). Available at: http://seer.cancer.gov/. Accessed July 8, 2013.
National Program of Cancer Registries (NPCR). Available at: http://www.cdc.gov/cancer/npcr/. Accessed 8 July 2013.
North American Association of Central Cancer Registries (NAACCR). Available at: http://www.naaccr.org/StandardsandRegistryOperations/VolumeII.aspx. Accessed 8 July 2013.
Winchester DP, Stewart AK, Bura C, Jones RS. The National Cancer Data Base: a clinical surveillance and quality improvement tool. J Surg Oncol. 2004;85:1–3.
Bilimoria KY, Stewart AK, Winchester DP, Ko CY. The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol. 2008;15:683–90.
Williams RT, Stewart AK, Winchester DP. (2012) Monitoring the delivery of cancer care: Commission on Cancer and National Cancer Data Base. Surg Oncol Clin N Am. 21:377–88.
Facility Oncology Registry Data Standards (FORDS). Revised for 2013: Commission on Cancer. Available at: http://www.facs.org/cancer/coc/fordsmanual.html.
Wolfinger R, O’Connell M. Generalized linear mixed models a pseudo-likelihood approach. J Stat Comput Simul. 1993;48:233–43.
Liao JG, Lipsitz SR. A type of restricted maximum likelihood estimator of variance components in generalized linear mixed models. Biometrika., 2002;89:401–9.
Cancer Program and Data Standards. Available at: http://www.facs.org/cancer/coc/standards.html. Accessed 8 July 2013.
Shi Q, You YN, Nelson H, Allen MS, Winchester D, Stewart A, et al. Cancer registries: a novel alternative to long-term clinical trial follow-up based on results of a comparative study. Clinical Trials. 2010;7:686–95.
Earle CC, Nattinger AB, Potosky AL, Lang K, Mallick R, Berger M, et al. Identifying cancer relapse using SEER-Medicare data. Med Care. 2002;40(IV):75–81.
Lamont EB, Herndon JE, 2nd, Weeks JC, Weeks JC, Henderson IC, Earle CC, et al. Measuring disease-free survival and cancer relapse using Medicare claims from CALGB breast cancer trial participants (companion to 9344). J Natl Cancer Inst. 2006;98:1335–8.
Yang Y, Mauldin PD, Ebeling M, Hulsey TC, Liu B, Thomas MB, et al. Effect of metabolic syndrome and its components on recurrence and survival in colon cancer patients. Cancer. 2013;119:1512–20.
Stokes ME, Thompson D, Montoya EL, Weinstein MC, Winer EP, Earle CC. Ten-year survival and cost following breast cancer recurrence: estimates from SEER-medicare data. Value Health. 2008;11:213–20.
Cheng L, Swartz MD, Zhao H, Kapadia AS, Lai D, Rowan PJ, et al. Hazard of recurrence among women after primary breast cancer treatment—a 10-year follow-up using data from SEER-Medicare. Cancer Epidemiol Biomarkers Prev. 2012;21:800–9.
Hassett MJ, Ritzwoller DP, Taback N, Carroll N, Cronin AM, Ting GV, et al. Validating billing/encounter codes as indicators of lung, colorectal, breast, and prostate cancer recurrence using 2 large contemporary cohorts. Med Care. 2012. doi:10.1097/MLR.0b013e318277eb6f.
Disclosure
None.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix A
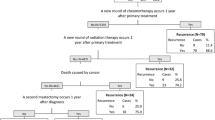
Variable Codes That Define Incomplete Information
-
Date of recurrence is coded as being entirely unknown (DATE OF FIRST RECURRENCE, NAACCR Item #1860 = 99999999) and the recurrence flag variable indicates there is a recurrence, but the date is unknown (RECURRENCE DATE-1ST FLAG, NAACCR Item #1861 = 12).
-
Date of recurrence is coded as being entirely unknown (DATE OF FIRST RECURRENCE NAACCR Item #1860 = 99999999) and the recurrence flag variable indicates it is unknown if the patient was ever disease-free or had first recurrence (RECURRENCE DATE-1ST FLAG, NAACCR Item #1861 = 10).
-
Disease has recurred, but the type of recurrence is unknown (TYPE OF FIRST RECURRENCE, NAACCR Item#1880 = 88).
-
It is unknown whether the disease has recurred or if the patient was ever disease-free (TYPE OF FIRST RECURRENCE, NAACCR Item#1880 = 99).
-
The variable to indicate whether there was or there was not a recurrence is left entirely blank (TYPE OF FIRST RECURRENCE, NAACCR Item#1880 = .)
Appendix B
See Table 5.
Rights and permissions
About this article
Cite this article
In, H., Bilimoria, K.Y., Stewart, A.K. et al. Cancer Recurrence: An Important but Missing Variable in National Cancer Registries. Ann Surg Oncol 21, 1520–1529 (2014). https://doi.org/10.1245/s10434-014-3516-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-3516-x