Abstract
Background
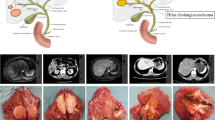
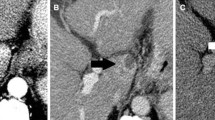
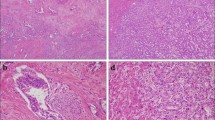
Peripheral cholangiocarcinoma (PCC) can be grossly classified into mass-forming, periductal-infiltrating, and intraductal papillary (IP) types. Information on IP-PCC patients undergoing hepatectomy is sparse because of the small number of cases.
Methods
The clinical features of 40 IP-PCC patients undergoing hepatectomy between 1977 and 2000 were reviewed. The clinical features of 94 PCC patients without IP growth undergoing hepatectomy were used for comparison.
Results
IP-PCC and non–IP-PCC groups had similar age distributions (P = .674), sex ratios (P = .079), and positive rates for serum carcinoembryonic antigen and CA 19–9 (P = .121 and .795, respectively). The two groups also exhibited similar rates of association between hepatolithiasis and PCC (P = .230). However, more IP-PCC patients exhibited signs during admission, and more had ALT values >36 IU/L; they also had smaller tumors, more mucobilia association, and tumors in earlier stages and had undergone more postoperative chemotherapy. Multivariate logistic regression analysis showed that only ALT >36 IU/L differentiated IP-PCC from non–IP-PCC patients. The two groups exhibited similar operative mortality (P = 1.0). Follow-up ranged from 1.6 to 125.2 months (mean and median, 44.6 and 5.7 months, respectively). The 1-, 3-, and 5-year overall survival rates were 72.9%, 41.2%, and 24.7%, respectively, in the IP-PCC group and 43.3, 6.03%, and 2.01% in the non–IP-PCC group. The prognosis was favorable for the IP-PCC patients (P < .00001), particularly for IP-PCC patients who received curative hepatectomy (P = .013).
Conclusions
IP-PCC patients had significantly better survival than non–IP-PCC patients, and aggressive curative hepatic resection is associated with a longer survival.
Similar content being viewed by others
REFERENCES
Chen MF. Peripheral cholangiocarcinoma (cholangiocellular carcinoma): clinical features, diagnosis and treatment. J Gastroenterol Hepatol 1999;14:1144–49.
Liver Cancer Study Group of Japan. Classification of Primary Liver Cancer. Tokyo: Kanehara, 1997.
Yamamoto J, Kosuge T, Takayama T, et al. Surgical treatment of intrahepatic cholangiocarcinoma: four patients surviving more than five years. Surgery 1992;111:617–22.
Yamamoto J, Kosuge T, Shimada K, et al. Intrahepatic cholangiocarcinoma: proposal of new macroscopic classification (in Japanese). Nippon Geka Gakkai Zasshi 1993;94:1194–200.
Suh KS, Roh HR, Koh YT, Lee KU, Park YH, Kim SW. Clinicopathologic features of the intraductal growth type of peripheral cholangiocarcinoma. Hepatology 2000;31:12–7.
Ohashi K, Nakajima Y, Kanehiro H, et al. Ki-ras mutations and p53 protein expressions in intrahepatic cholangiocarcinomas: relation to gross tumor morphology. Gastroenterology 1995;109:1612–7.
Chen TC, Nakanuma Y, Zen Y, Chen M-F. Intraductal papillary neoplasia of the liver associated with hepatolithiasis. Hepatology 2001;34:651–8.
Sobin LH, Wittekind C, eds. TNM Classification of Malignant Tumours. 5th ed. New York: Wiley-Liss, 1997.
Koga A, Ichimiya H, Yamaguchi K, et al. Hepatolithiasis associated with cholangiocarcinoma: possible etiologic significance. Cancer 1985;55:2826–9.
Ohta T, Nagakawa T, Ueda N. Mucosal dysplasia of the liver and intraductal variant of peripheral cholangiocarcinoma in hepatolithiasis. Cancer 1991;68:2217–23.
Ohta G, Nakayama Y, Terata T. Intrahepatic calculi. Nakayama F, eds. Pathology of Hepatolithiasis: Cholangitis and Cholangiocarcinoma New York: Alan R. Liss, 1984: 91–113
Sanes S, MacCallum JD. Primary carcinoma of the liver. Cholangioma in hepatolithiasis. Am J Pathol 1942;18:674–83.
Chen MF. Mucobilia: the clinical spectrum, diagnosis and treatment. J Gastroenterol Hepatol 1998;13:1084–90.
Chen MF, Jan YY, Chen TS. Clinical studies of mucin-producing cholangiocarcinoma. A study of 22 histopathology-proven cases. Ann Surg 1998;227:63–9.
Yeh CN, Chen MF, Lee WC, Jeng L. Prognostic factors of hepatic resection for hepatocellular carcinoma with cirrhosis: univariate and multivariate analysis. J Surg Oncol 2002;81:195–202.
Chen MF, Tsai HP, Jeng L, et al. Prognostic factors after resection for hepatocellular carcinoma in noncirrhotic livers: univariate and multivariate analysis. World J Surg 2003;27:443–7.
Klompje J, Petrelli NJ, Herrera L, Mittelman A. The prognostic value of preoperative alkaline-phosphatase for resection of solitary liver metastasis from colorectal carcinoma. Eur J Surg Oncol 1987;13:345–7.
Okabayashi T, Yamamoto J, Kosuge T, et al. A new staging system for mass-forming intrahepatic cholangiocarcinoma: analysis of preoperative and postoperative variables. Cancer 2001;92:2374–83.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yeh, CN., Jan, YY., Yeh, TS. et al. Hepatic Resection of the Intraductal Papillary Type of Peripheral Cholangiocarcinoma. Ann Surg Oncol 11, 606–611 (2004). https://doi.org/10.1245/ASO.2004.04.028
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1245/ASO.2004.04.028