Abstract
Background
In a previous randomized, triple-masked, placebo-controlled study, the authors demonstrated that extending a single-injection paravertebral nerve block with a multiple-day perineural local anesthetic infusion improves analgesia and decreases pain-related dysfunction during the 3-day infusion but not subsequent to catheter removal within 1 month after mastectomy. This report describes a prospective follow-up study of the previously published trial to investigate the possibility that extending a single-injection paravertebral block with a multiple-day infusion may decrease persistent postsurgical pain as well as pain-induced emotional and functional dysfunction 1 year after mastectomy.
Methods
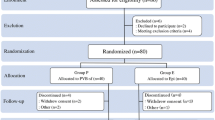
Subjects undergoing uni- or bilateral mastectomy received unilateral (n = 24) or bilateral (n = 36) single-injection thoracic paravertebral block(s) with ropivacaine and perineural catheter(s). The subjects were randomized to receive either ropivacaine 0.4 % (n = 30) or normal saline (n = 30) via their catheters until the catheters were removed on postoperative day 3. Chronic pain and pain-related physical and emotional dysfunction were measured using the Brief Pain Inventory (BPI).
Results
No statistically significant difference between treatments 3 months after surgery was observed with the BPI. In contrast, after 12 months, only 4 subjects (13 %) who had received a perineural ropivacaine infusion reported pain-induced dysfunction compared with 14 (47 %) who had received saline infusion (P = 0.011). At 12 months, the mean BPI was 1.6 ± 4.6 for the subjects who received ropivacaine versus 5.9 ± 11.3 for the subjects who received saline (P = 0.007).
Conclusions
Adding a multiple-day, continuous ropivacaine infusion to a single-injection ropivacaine paravertebral nerve block may result in a lower incidence of pain as well as pain-related physical and emotional dysfunction 1 year after mastectomy.
Similar content being viewed by others
References
Kairaluoma PM, Bachmann MS, Korpinen AK, Rosenberg PH, Pere PJ. Single-injection paravertebral block before general anesthesia enhances analgesia after breast cancer surgery with and without associated lymph node biopsy. Anesth Analg. 2004;99:1837–43.
Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006 367:1618–25.
Gartner R, Jensen MB, Nielsen J, Ewertz M, Kroman N, Kehlet H. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA. 2009;302:1985–92.
Mejdahl MK, Andersen KG, Gartner R, Kroman N, Kehlet H. Persistent pain and sensory disturbances after treatment for breast cancer: six-year nationwide follow-up study. BMJ. 2013;346:1865.
Jung BF, Ahrendt GM, Oaklander AL, Dworkin RH. Neuropathic pain following breast cancer surgery: proposed classification and research update. Pain. 2003 104:1–13.
Tasmuth T, von Smitten K, Hietanen P, Kataja M, Kalso E. Pain and other symptoms after different treatment modalities of breast cancer. Ann Oncol. 1995;6:453–9.
Tasmuth T, Estlanderb AM, Kalso E. Effect of present pain and mood on the memory of past postoperative pain in women treated surgically for breast cancer. Pain. 1996;68:343–7.
Senturk M, Ozcan PE, Talu GK, et al. The effects of three different analgesia techniques on long-term postthoracotomy pain. Anesth Analg. 2002;94:11–5.
Andreae MH, Andreae DA. Regional anaesthesia to prevent chronic pain after surgery: a Cochrane systematic review and meta-analysis. Br J Anaesth. 2013;111:711–20.
Klein SM, Bergh A, Steele SM, Georgiade GS, Greengrass RA. Thoracic paravertebral block for breast surgery. Anesth Analg. 2000;90:1402–5.
Kairaluoma PM, Bachmann MS, Rosenberg PH, Pere PJ. Preincisional paravertebral block reduces the prevalence of chronic pain after breast surgery. Anesth Analg. 2006;103:703–8.
Ibarra MM, S-Carralero GC, Vicente GU, Cuartero del Pozo A, Lopez Rincon R, Fajardo del Castillo MJ. Chronic postoperative pain after general anesthesia with or without a single-dose preincisional paravertebral nerve block in radical breast cancer surgery (in Spanish). Rev Espanola Anestesiol Reanimacion. 2011;58:290–4.
Shankarappa SA, Tsui JH, Kim KN, et al. Prolonged nerve blockade delays the onset of neuropathic pain. Proc Nat Acad Sci USA. 2012;109:17555–60.
Ilfeld BM. Continuous peripheral nerve blocks: a review of the published evidence. Anesth Analg. 2011;113:904–25.
Ilfeld BM, Enneking FK. Continuous peripheral nerve blocks at home: a review. Anesth Analg. 2005;100:1822–33.
Ilfeld BM, Madison SJ, Suresh PJ, et al. Treatment of postmastectomy pain with ambulatory continuous paravertebral nerve blocks: a randomized, triple-masked, placebo-controlled study. Reg Anesth Pain Med. 2014;39:89–96.
Dijkstra PU, Rietman JS, Geertzen JH. Phantom breast sensations and phantom breast pain: a 2-year prospective study and a methodological analysis of literature. Eur J Pain. 2007;11:99–108.
Borghi B, D’Addabbo M, White PF, et al. The use of prolonged peripheral neural blockade after lower extremity amputation: the effect on symptoms associated with phantom limb syndrome. Anesth Analg. 2010;111:1308–15.
Ilfeld BM, Moeller-Bertram T, Hanling SR, et al. Treating intractable phantom limb pain with ambulatory continuous peripheral nerve blocks: a pilot study. Pain Med. 2013;14:935–42.
World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. JAMA. 2000;284:3043–5.
Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23:129–38.
Mendoza TR, Chen C, Brugger A, et al. The utility and validity of the modified brief pain inventory in a multiple-dose postoperative analgesic trial. Clin J Pain. 2004;20:357–62.
Dworkin RH, Turk DC, Peirce-Sandner S, et al. Research design considerations for confirmatory chronic pain clinical trials: IMMPACT recommendations. Pain. 2010;149:177–93.
Dworkin RH, Turk DC, Farrar JT, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19.
Dworkin RH, Turk DC, McDermott MP, et al. Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations. Pain. 2009;146:238–44.
Turk DC, Dworkin RH, Burke LB, et al. Developing patient-reported outcome measures for pain clinical trials: IMMPACT recommendations. Pain. 2006;125:208–15.
Mann HB, Whitney DR. On a test of whether one of two random variables is stochastically larger than the other. Ann Math Stat. 1947;18:50–60.
Howlader N, Noone AM, Krapcho M, et al (2014) SEER Cancer Statistics Review, 1975–2009. National Cancer Institute: Bethesda.
Habermann EB, Abbott A, Parsons HM, Virnig BA, Al-Refaie WB, Tuttle TM. Are mastectomy rates really increasing in the United States? J Clin Oncol. 2010;28:3437–41.
Birbaumer N, Lutzenberger W, Montoya P, et al. Effects of regional anesthesia on phantom limb pain are mirrored in changes in cortical reorganization. J Neurosci. 1997;17:5503–8.
Kehlet H, Rathmell JP. Persistent postsurgical pain: the path forward through better design of clinical studies. Anesthesiology. 2010;112:514–5.
Woolf CJ, Mannion RJ. Neuropathic pain: aetiology, symptoms, mechanisms, and management. Lancet. 1999;353:1959–64.
Nikolajsen L, Ilkjaer S, Jensen TS. Relationship between mechanical sensitivity and postamputation pain: a prospective study. Eur J Pain. 2000;4:327–34.
Devor M, Govrin-Lippmann R, Angelides K. Na+ channel immunolocalization in peripheral mammalian axons and changes following nerve injury and neuroma formation. J Neurosci. 1993;13:1976–92.
McLachlan EM, Janig W, Devor M, Michaelis M. Peripheral nerve injury triggers noradrenergic sprouting within dorsal root ganglia. Nature. 1993;363:543–6.
Woolf CJ, Shortland P, Coggeshall RE. Peripheral nerve injury triggers central sprouting of myelinated afferents. Nature. 1992;355:75–8.
Woolf CJ, Salter MW. Neuronal plasticity: increasing the gain in pain. Science. 2000;288:1765–9.
Kwekkeboom K. Postmastectomy pain syndromes. Cancer Nurs. 1996;19:37–43.
Bagry H, de la Cuadra Fontaine JC, Asenjo JF, Bracco D, Carli F. Effect of a continuous peripheral nerve block on the inflammatory response in knee arthroplasty. Reg Anesth Pain Med. 2008;33:17–23.
Martin F, Martinez V, Mazoit JX, et al. Antiinflammatory effect of peripheral nerve blocks after knee surgery: clinical and biologic evaluation. Anesthesiology. 2008;109:484–90.
Karmakar MK, Samy W, Li JW, et al. Thoracic paravertebral block and its effects on chronic pain and health-related quality of life after modified radical mastectomy. Reg Anesth Pain Med. 2014;39:289–98.
Vallejo MC, Phelps AL, Sah N, et al. Preemptive analgesia with bupivacaine for segmental mastectomy. Reg Anesth Pain Med. 2006;31:227–32.
Sidiropoulou T, Buonomo O, Fabbi E, et al. A prospective comparison of continuous wound infiltration with ropivacaine versus single-injection paravertebral block after modified radical mastectomy. Anesth Analg. 2008;106:997–1001.
Albi-Feldzer A, Mouret-Fourme EE, Hamouda S, et al. A double-blind randomized trial of wound and intercostal space infiltration with ropivacaine during breast cancer surgery: effects on chronic postoperative pain. Anesthesiology. 2013;118:318–26.
Exadaktylos AK, Buggy DJ, Moriarty DC, Mascha E, Sessler DI. Can anesthetic technique for primary breast cancer surgery affect recurrence or metastasis? Anesthesiology. 2006;105:660–4.
McElwain J, Freir NM, Burlacu CL, Moriarty DC, Sessler DI, Buggy DJ. The feasibility of patient-controlled paravertebral analgesia for major breast cancer surgery: a prospective, randomized, double-blind comparison of two regimens. Anesth Analg. 2008;107:665–8.
Buckenmaier CC, III, Klein SM, Nielsen KC, Steele SM. Continuous paravertebral catheter and outpatient infusion for breast surgery. Anesth Analg. 2003;97:715–7.
Buckenmaier CC III, Kwon KH, Howard RS, et al. Double-blinded, placebo-controlled, prospective randomized trial evaluating the efficacy of paravertebral block with and without continuous paravertebral block analgesia in outpatient breast cancer surgery. Pain Med. 2010;11:790–9.
Burlacu CL, Frizelle HP, Moriarty DC, Buggy DJ. Fentanyl and clonidine as adjunctive analgesics with levobupivacaine in paravertebral analgesia for breast surgery. Anaesthesia. 2006;61:932–7.
Iohom G, Abdalla H, O’Brien J, et al. The associations between severity of early postoperative pain, chronic postsurgical pain, and plasma concentration of stable nitric oxide products after breast surgery. Anesth Analg. 2006;103:995–1000.
Buggy DJ, Kerin MJ. Paravertebral analgesia with levobupivacaine increases postoperative flap tissue oxygen tension after immediate latissimus dorsi breast reconstruction compared with intravenous opioid analgesia. Anesthesiology. 2004;100:375–80.
Schnabel A, Reichl SU, Kranke P, Pogatzki-Zahn EM, Zahn PK. Efficacy and safety of paravertebral blocks in breast surgery: a meta-analysis of randomized controlled trials. Br J Anaesth. 2010;105:842–52.
Naesh O, Haljamae H, Hindberg I, Holm J, Jivegard L, Wennmalm A. Epidural anaesthesia prolonged into the postoperative period prevents stress response and platelet hyperaggregability after peripheral vascular surgery. Eur J Vasc Surg. 1994;8:395–400.
Lewis GN, Rice DA, McNair PJ. Conditioned pain modulation in populations with chronic pain: a systematic review and meta-analysis. J Pain. 2012;13:936–44.
Yarnitsky D, Crispel Y, Eisenberg E, et al. Prediction of chronic postoperative pain: preoperative DNIC testing identifies patients at risk. Pain. 2008;138:22–8.
Wilder-Smith OH, Schreyer T, Scheffer GJ, Arendt-Nielsen L. Patients with chronic pain after abdominal surgery show less preoperative endogenous pain inhibition and more postoperative hyperalgesia: a pilot study. J Pain Palliat Care Pharmacother. 2010;24:119–28.
Acknowledgment
Funding for this project was provided by National Institutes of Health Grant GM077026 (P.I.: Dr. Ilfeld) from the National Institute of General Medical Sciences (Bethesda, MD, USA); the Clinical and Translational Research Institute, University of California, San Diego (San Diego, CA, USA), with funding provided by National Institutes of Health grants UL1RR031980 and UL1TR000100; the Department of Anesthesiology, University of California San Diego (San Diego, CA, USA) and Baxter Healthcare International (Deerfield, IL, USA). This company also provided the portable infusion pumps used in the original investigation but had no input into any aspect of study conceptualization, design and implementation, data collection, analysis and interpretation, or manuscript preparation. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the funding entities.
Disclosure
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ilfeld, B.M., Madison, S.J., Suresh, P.J. et al. Persistent Postmastectomy Pain and Pain-Related Physical and Emotional Functioning With and Without a Continuous Paravertebral Nerve Block: A Prospective 1-Year Follow-Up Assessment of a Randomized, Triple-Masked, Placebo-Controlled Study. Ann Surg Oncol 22, 2017–2025 (2015). https://doi.org/10.1245/s10434-014-4248-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-4248-7