Abstract
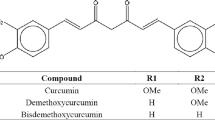
The oral bioavailability of curcumin is limited, attributed to its low solubility or dissolution and poor absorption. Herein, the study describes formulation of curcumin-loaded mixed micelles of Gelucire® 48/16 and TPGS for its dissolution rate enhancement. Curcumin was dispersed in these molten lipidic surfactants which was then adsorbed on carrier and formulated as pellets by extrusion spheronization. Critical micelle concentration (CMC) of binary mixture of Gelucire® 48/16 and TPGS was lower than their individual CMC demonstrating the synergistic behavior of mixture. Thermodynamic parameters like partition coefficient and Gibbs free energy of solubilization indicated that mixed micelles were more efficient than micelles of its individual components in curcumin solubilization. Dynamic light scattering (DLS) suggested slight increase in micellar size of mixed micelles than its components suggesting curcumin loading in mixed micelles. Fourier transform infrared spectroscopy (FTIR) revealed that phenolic hydroxyl group interacts with lipids which contribute to its enhanced solubility. Furthermore, the differential scanning calorimetry (DSC) and X-ray diffraction (XRD) study indicated the conversion of crystalline curcumin into amorphous form. In the pellet formulation, Gelucire® 48/16 acted as a binder and eliminated the requirement of additional binder. Microcrystalline cellulose (MCC) forms wet mass and retards the release of curcumin from pellets. Increase in concentration of water-soluble diluent increased drug release. The optimized formulation released more than 90% drug and maintains supersaturation level of curcumin for 2 h. Thus, mixed micellar system was effective delivery system for curcumin while pellet formulation is an interesting formulation strategy consisting semi-solid lipids.
Graphical Abstract








Similar content being viewed by others
References
Zhao L, Du J, Duan Y, Zang Y, Zhang H, Yang C, et al. Curcumin loaded mixed micelles composed of Pluronic P123 and F68: preparation, optimization and in vitro characterization. Colloids Surf B: Biointerfaces. 2012;97:101–8. https://doi.org/10.1016/j.colsurfb.2012.04.017.
Shen L, Ji H. The pharmacology of curcumin : is it the degradation products ? Trends Mol Med. 2012;18(3):138–44. https://doi.org/10.1016/j.molmed.2012.01.004.
Banez MJ, Geluz MI, Chandra A, Hamdan T, Biswas OS, Bryan NS, et al. A systemic review on the antioxidant and anti- inflammatory effects of resveratrol, curcumin, and dietary nitric oxide supplementation on human cardiovascular health. Nutr Res. 2020;78:11–26. https://doi.org/10.1016/j.nutres.2020.03.002.
Mathew D, Hsu W. Antiviral potential of curcumin. J Funct Foods. 2018;40:692–9. https://doi.org/10.1016/j.jff.2017.12.017.
Aditya NP, Chimote G, Gunalan K, Banerjee R, Patankar S, Madhusudhan B. Curcuminoids-loaded liposomes in combination with arteether protects against Plasmodium berghei infection in mice. Exp Parasitol. 2012;131(3):292–9. https://doi.org/10.1016/j.exppara.2012.04.010.
Changtam C, De Koning HP, Ibrahim H, Sajid MS, Gould MK, Suksamrarn A. Curcuminoid analogs with potent activity against Trypanosoma and Leishmania species. Eur J Med Chem. 2010;45(3):941–56. https://doi.org/10.1016/j.ejmech.2009.11.035.
Sun J, Chen F, Braun C, Zhou Y-Q, Rittner H, Tian Y-K, et al. Role of curcumin in the management of pathological pain. Phytomedicine. 2018;48:129–40. https://doi.org/10.1016/j.phymed.2018.04.045.
Priebe W, Jasi UT, Lewandowski W. Curcumin as tyrosine kinase inhibitor in cancer treatment. Eur J Med Chem. 2019;181:111512. https://doi.org/10.1016/j.ejmech.2019.07.015.
Li H, Sureda A, Devkota HP, Pittalà V, Barreca D, Silva AS, et al. Curcumin, the golden spice in treating cardiovascular diseases. Biotechnol Adv. 2019;38:107343. https://doi.org/10.1016/j.biotechadv.2019.01.010.
Amalraj A, Jude S, Varma K, Jacob J, Gopi S, Oluwafemi OS, et al. Preparation of a novel bioavailable curcuminoid formulation (CureitTM) using Polar-Nonpolar-Sandwich (PNS) technology and its characterization and applications. Mater Sci Eng C. 2017;75:359–67. https://doi.org/10.1016/j.msec.2017.02.068.
Kakkar V, Kaur IP. Evaluating potential of curcumin loaded solid lipid nanoparticles in aluminium induced behavioural , biochemical and histopathological alterations in mice brain. Food Chem Toxicol. 2011;49(11):2906–13. https://doi.org/10.1016/j.fct.2011.08.006.
Kim T, Davis J, Zhang AJ, He X, Mathews ST. Curcumin activates AMPK and suppresses gluconeogenic gene expression in hepatoma cells. Biochem Biophys Res Commun. 2009;388(2):377–82. https://doi.org/10.1016/j.bbrc.2009.08.018.
Parsamanesh N, Moossavi M, Bahrami A, Butler AE, Sahebkar A. Therapeutic potential of curcumin in diabetic complications. Pharmacol Res. 2018;136:181–93. https://doi.org/10.1016/j.phrs.2018.09.012.
Ma Z, Na W, He H, Tang X. Pharmaceutical strategies of improving oral systemic bioavailability of curcumin for clinical application. J Control Release. 2019;316:359–80. https://doi.org/10.1016/j.jconrel.2019.10.053.
Sadeghi F, Ashofteh M, Homayouni A, Abbaspour M, Nokhodchi A, Garekani HA. Antisolvent precipitation technique: A very promising approach to crystallize curcumin in presence of polyvinyl pyrrolidon for solubility and dissolution enhancement. Colloids Surf B: Biointerfaces. 2016;147:258–64. https://doi.org/10.1016/j.colsurfb.2016.08.004.
Ipar VS, Dsouza A, Devarajan PV. Enhancing curcumin oral bioavailability through nanoformulations. Eur J Drug Metab Pharmacokinet. 2019;44(4):459–80. https://doi.org/10.1007/s13318-019-00545-z.
Williams HD, Trevaskis NL, Yeap YY, Anby MU, Pouton CW, Porter CJH Lipid-based formulations and drug supersaturation : harnessing the unique benefits of the lipid digestion/absorption pathway. 2013;30(12):2976-2992. https://doi.org/10.1007/s11095-013-1126-0.
Gelucire® family. https://www.pharmaexcipients.com/news/the-gelucire-family-semi-solid-excipients-by-gattefosse/. Accessed 30 Dec 2020.
Liu RUI, Liu Z, Zhang C, Zhang B. Gelucire44 / 14 as a novel absorption enhancer for drugs with different hydrophilicities : in vitro and in vivo improvement on transcorneal permeation. J Pharm Sci. 2011;100(8):3186–95. https://doi.org/10.1002/jps.22540.
Mitsutake H, Neves MDG, Rutledge DN, Poppi RJ, Breitkreitz MC. Extraction of information about structural changes in a semisolid pharmaceutical formulation from near-infrared and Raman images by multivariate curve resolution–alternating least squares and ComDim. J Chemom. 2020;34(12):1–16. https://doi.org/10.1002/cem.3288.
Gattefossé. Oral Drug Delivery with lipid Excipients. https://www.gattefosse.com/pharmaceuticals-content/lipid-based-drug-delivery-systems. Accessed 30 Dec 2020.
Gelucire® 48/16 Pellets. Solubility and oral bioavailability enhancement. https://www.pharmaexcipients.com/wp-content/uploads/2020/03/Gelucire-48-16_solubility-and-bioavailability-enhancer-from-Gattefosse.pdf. Accessed 30 Dec 2020.
Xua S, Dai WG. Drug precipitation inhibitors in supersaturable formulations. Int J Pharm. 2013;453(1):36–43. https://doi.org/10.1016/j.ijpharm.2013.05.013.
Feng D, Peng T, Huang Z, Singh V, Shi Y, Wen T, et al. Polymer–surfactant system based amorphous solid dispersion: Precipitation inhibition and bioavailability enhancement of itraconazole. Pharmaceutics. 2018;10(2):1–15. https://doi.org/10.3390/pharmaceutics10020053.
Brouwers J, Brewster ME, Augustijns P. Supersaturating drug delivery systems: the answer to solubility-limited oral bioavailability? J Pharm Sci. 2009;98:2549–72. https://doi.org/10.1002/jps.21650.
Chaudhari SP, Dugar RP. Application of surfactants in solid dispersion technology for improving solubility of poorly water soluble drugs Smruti. J Drug Deliv Sci Technol. 2017;41:68–77. https://doi.org/10.1016/j.jddst.2017.06.010.
Gao Y, Li LB, Zhai G. Preparation and characterization of Pluronic/TPGS mixed micelles for solubilization of camptothecin. Colloids Surf B: Biointerfaces. 2008;64(2):194–9. https://doi.org/10.1016/j.colsurfb.2008.01.021.
Zhang Z, Tan S, Feng SS. Vitamin E TPGS as a molecular biomaterial for drug delivery. Biomaterials. 2012;33(19):4889–906. https://doi.org/10.1016/j.biomaterials.2012.03.046.
Sobczyński J, Chudzik-Rząd B. Mixed micelles as drug delivery nanocarriers. Design and Development of New Nanocarriers. 2018. 331–364 p.
Duan Y, Zhang B, Chu L, Tong HHY, Liu W, Zhai G. Evaluation in vitro and in vivo of curcumin-loaded mPEG-PLA/TPGS mixed micelles for oral administration. Colloids Surf B: Biointerfaces. 2016;141:345–54. https://doi.org/10.1016/j.colsurfb.2016.01.017.
Parikh A, Kathawala K, Song Y, Zhou XF, Garg S. Curcumin-loaded self-nanomicellizing solid dispersion system: part I: development, optimization, characterization, and oral bioavailability. Drug Deliv Transl Res. 2018;8(5):1389–405. https://doi.org/10.1007/s13346-018-0543-3.
Wei T, Manickam S. Response Surface Methodology, an an effective strategy in the optimization of the generation of curcumin-loaded micelles. Asia Pac J Chem Eng. 2012;7:S125–33.
Zhao L, Du J, Duan Y, Zang Y, Zhang H, Yang C, et al. Curcumin loaded mixed micelles composed of Pluronic P123 and F68: preparation, optimization and in vitro characterization. Colloids Surf B: Biointerfaces. 2012;97:101–8. https://doi.org/10.1016/j.colsurfb.2012.04.017.
Patil S, Choudhary B, Rathore A, Roy K, Mahadik K. Enhanced oral bioavailability and anticancer activity of novel curcumin loaded mixed micelles in human lung cancer cells. Phytomedicine. 2015;22(12):1103–11. https://doi.org/10.1016/j.phymed.2015.08.006.
Jaiswal M, Kumar M, Pathak K. Zero order delivery of itraconazole via polymeric micelles incorporated in situ ocular gel for the management of fungal keratitis. Colloids Surf B: Biointerfaces. 2015;130:23–30. https://doi.org/10.1016/j.colsurfb.2015.03.059.
Pokharkar V, Suryawanshi S, Dhapte-Pawar V. Exploring micellar-based polymeric systems for effective nose-to-brain drug delivery as potential neurotherapeutics. Drug Deliv Transl Res. 2020;10(4):1019–31. https://doi.org/10.1007/s13346-019-00702-6.
Singla P, Singh O, Chabba S, Aswal VK, Mahajan RK. Sodium deoxycholate mediated enhanced solubilization and stability of hydrophobic drug Clozapine in pluronic micelles. Spectrochim Acta - Part A Mol Biomol Spectrosc. 2018;191:143–54. https://doi.org/10.1016/j.saa.2017.10.015.
Singla P, Chabba S, Mahajan RK. A systematic physicochemical investigation on solubilization and in vitro release of poorly water soluble oxcarbazepine drug in pluronic micelles. Colloids Surfaces A Physicochem Eng Asp. 2016;504:479–88. https://doi.org/10.1016/j.colsurfa.2016.05.043.
Parekh P, Singh K, Marangoni DG, Bahadur P. Micellization and solubilization of a model hydrophobic drug nimesulide in aqueous salt solutions of Tetronic® T904. Colloids Surf B: Biointerfaces. 2011;83(1):69–77. https://doi.org/10.1016/j.colsurfb.2010.10.046.
Anitha A, Deepagan VG, Divya Rani VV, Menon D, Nair SV, Jayakumar R. Preparation, characterization, in vitro drug release and biological studies of curcumin loaded dextran sulphate-chitosan nanoparticles. Carbohydr Polym. 2011;84(3):1158–64. https://doi.org/10.1016/j.carbpol.2011.01.005.
Mailafiya MM, Abubakar K, Danmaigoro A, Chiroma SM, Rahim EBA, Moklas MAM, et al. Evaluation of in vitro release kinetics and mechanisms of curcumin-loaded cockle shell-derived calcium carbonate nanoparticles. Biomed Res Ther. 2019;6(12):3518–40. https://doi.org/10.15419/bmrat.v6i12.580.
Nasser B, Aldosari A. Development and evaluation of self-nanoemulsifying drug delivery systems for oral delivery of indomethacin. 2018. https://www.researchgate.net/publication/331465365_Development_and_evaluation_of_self-nanoemulsifying_drug_delivery_systems_for_oral_delivery_of_indomethacin. Accessed 5 Nov 2020.
Kaur V, Goyal AK, Ghosh G, Chandra S, Rath G. Development and characterization of pellets for targeted delivery of 5-fluorouracil and phytic acid for treatment of colon cancer in Wistar rat. Heliyon. 2020;6:e03125. https://doi.org/10.1016/j.heliyon.2019.e03125.
Goyanes A, Souto C, Martínez-pacheco R. Co-processed MCC-EudragitÒ E excipients for extrusion–spheronization. Eur J Pharm Biopharm. 2011;79:658–63. https://doi.org/10.1016/jejpb.2011.07.013.
Acknowledgements
Authors are thankful to the University Grants Commission (UGC), New Delhi, for providing fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Guest Editors: Harsh Chauhan, Abhijit Date and Sonali Dhindwal
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shinde, U.K., Suryawanshi, D.G. & Amin, P.D. Development of Gelucire® 48/16 and TPGS Mixed Micelles and Its Pellet Formulation by Extrusion Spheronization Technique for Dissolution Rate Enhancement of Curcumin. AAPS PharmSciTech 22, 182 (2021). https://doi.org/10.1208/s12249-021-02032-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-021-02032-8