Abstract
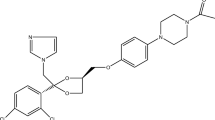
We focused to explore a suitable solvent for rifampicin (RIF) recommended for subcutaneous (sub-Q) delivery [ethylene glycol (EG), propylene glycol (PG), tween 20, polyethylene glycol-400 (PEG400), oleic acid (OA), N-methyl-2-pyrrolidone (NMP), cremophor-EL (CEL), ethyl oleate (EO), methanol, and glycerol] followed by computational validations and in-silico prediction using GastroPlus. The experimental solubility was conducted over temperature ranges T = 298.2–318.2 K) and fixed pressure (p = 0.1 MPa) followed by validation employing computational models (Apelblat, and vanʼt Hoff). Moreover, the HSPiP solubility software provided the Hansen solubility parameters. At T = 318.2K, the estimated maximum solubility (in term of mole fraction) values of the drug were in order of NMP (11.9 × 10-2) ˃ methanol (6.8 × 10-2) ˃ PEG400 (4.8 × 10-2) ˃ tween 20 (3.4 × 10-2). The drug dissolution was endothermic process and entropy driven as evident from “apparent thermodynamic analysis”. The activity coefficients confirmed facilitated RIF–NMP interactions for increased solubility among them. Eventually, GastroPlus predicted the impact of critical input parameters on major pharmacokinetics responses after sub-Q delivery as compared to oral delivery. Thus, NMP may be the best solvent for sub-Q delivery of RIF to treat skin tuberculosis (local and systemic) and cutaneous related disease at explored concentration.






Similar content being viewed by others
Abbreviations
- RIF:
-
rifampicin
- OA:
-
oleic acid
- EO:
-
ethyl oleate
- PG:
-
propylene glycol
- EG:
-
ethylene glycol
- RMSD:
-
root mean square deviation
- CEL:
-
cremophor-EL
- PEG400:
-
polyethylene glycol 400
- UPLC:
-
ultra performance liquid chromatography
- DSC:
-
differential scanning calorimeter
References
Wehrli W. Rifampin: Mechanisms of action and resistance, reviews of infectious diseases. Rev Infect Dis. 1983;5(3):S407–11.
Hussain A, Altamimi MA, Alshehri S, Imam SS, Shakeel F, Singh SK. Novel approach for transdermal delivery of rifampicin to induce synergistic antimycobacterial effects against cutaneous and systemic tuberculosis using a cationic nanoemulsion gel. Int J Nanomedicine. 2020;15:1073–94.
Thakur BK, Verma S, Hazarika DA. Clinicopathological study of cutaneous tuberculosis at Dibrugarh district, Assam. Indian J Dermatol. 2012;57:63–5.
Begum K, Shahid MS, Jalil R. Topical nanoemulsion of rifampicin with benzoic acid and salicylic acid: activity against staphylococcus aureus, stap. epidermis and candida albicans, Bangladesh. Pharm J. 2019;22:1–6.
Caon T, Campos CEM, Simões CMO, Silva MAS. Novel perspectives in the tuberculosis treatment: administration of isoniazid through the skin. Int J Pharm. 2015;494:463–70.
Chen S, Han Y, Yu D, Huo F, Wang F, Li Y, et al. Transdermal delivery of isoniazid and rifampin in guinea pigs by electro-phonophoresis. Drug Deliv. 2017;24(1):467–70.
Hussain A, Altamimi MA, Alshehri S, Imam SS, Singh SK. Vesicular elastic liposomes for transdermal delivery of rifampicin: in-vitro, in-vivo and in silico GastroPlus™ prediction studies. Eur J Pharm Sci. 2020;151:105411.
Ahmed M, Ramadan W, Rambhu D, Shakeel F. Potential of nanoemulsions for intravenous delivery of rifampicin. Pharmazie. 2008;63(11):806–11.
Mathur IS, Gupta HP, Srivastav SK, Singh S, Madhu K, Khanna NM. Evaluation of subdermal biodegradable implants incorporating rifampicin as a method of drug delivery in experimental tuberculosis of guinea pigs. J Med Microbiol. 1985;20:387–92.
Vyas SP, Kannan ME, Jain S, Mishra V, Singh P. Design of liposomal aerosols for improved delivery of rifampicin to alveolar macrophages. Int J Pharm. 2004;269:37–49.
Chen L, Xie Z, Hu J, Chen X, Jing X. Enantiomeric PLA– PEG block copolymers and their stereocomplex micelles used as rifampin delivery. J Nanopart Res. 2007;9:777–85.
Singh H, Jindal S, Singh M, Sharma G, Kaur IP. Nanoformulation of rifampicin with enhanced bioavailability: development, characterization and in-vivo safety. Int J Pharm. 2015;485:138–51.
Kitak T, Dumicic A, Planinsek O, Sibanc R, Srcic S. Determination of solubility 10 parameters of ibuprofen and ibuprofen lysinate. Molecules. 2015;20:21549–68.
Hussain A, Altamimi MA, Alshehri S, Imam SS. Assessment of solubility and Hansen solubility parameters of rifampicin in various permeation enhancers: experimental and computational approach. J Mol Liq. 2021:115432. In press, pre-proof.
Hussain A, Singh SK, Singh N, Verma PRP. In vitro-in vivo in-silico simulation studies of anti-tubercular drugs doped with self-nanoemulsifying drug delivery system. RSC Adv. 2016;6:93147–61.
Kalam MA, Khan AA, Alshamsan A, Haque A, Shakeel F. Solubility of a poorly soluble immunosuppressant in different pure solvents: measurement, correlation, thermodynamics and molecular interactions. J Mol Liq. 2018;249:53–60.
Hildebrand JH, Scott RL. The solubility of nonelectrolytes. New York: Reinhold Pub. Corp; 1950. p. 514.
Hildebrand JH, Scott RL. Regular solutions. Saddle River: Prentice-Hall; 1962. p. 202.
Van Krevelen DW, te Nijenhuis K. Properties of polymers: their correlation with chemical structure; their numerical estimation and prediction from additive group contributions. Amsterdam, The Netherland; Tokyo, Japan: Elsevier; 2009. p. 189.
Greenhalgh DJ, Williams AC, Timmins P, York P. Solubility parameters as predictors of miscibility in solid dispersions. J Pharm Sci. 1999;88(11):1182–90.
Hojjati H, Rohani S. Measurement and prediction of solubility of paracetamol in water–isopropanol solution. Part 2. Prediction. Org Process Res Dev. 2006;10:1110–8.
Hansen CM. Hansen solubility parameters: a user’s handbook. 2nd ed. Boca Raton: CRC Press, Taylor Francis Group; 2007. p. 544.
Ruidiaz MA, Delgado DR, Martínez F, Marcus Y. Solubility and preferential solvation of indomethacin in 1,4-dioxane + water solvent mixtures. Fluid Phase Equilib. 2010;299:259–65.
Halkowsky SH. Solubility and solubilization in aqueous media. New York: Oxford University Press; 1999, ISBN 0-8412-3576-7. p. 61–3.
Apelblat A, Manzurola E. Solubilities of o-acetylsalicylic, 4-aminosalicylic, 3,5-dinitrosalicylic and p-toluic acid and magnesium-DL-aspartate in water from T = 20 (278–348) K. J Chem Thermodyn. 1999;31:85–91.
Wei DW, Li H, Liu C, Wang BH. The effect of temperature on the solubility of 11-cyanoundecanoic acid in cyclohexane, n-hexane, and water. Ind Eng Chem Res. 2011;50:2473–7.
Manzurola E, Apelblat A. Solubilities of L-glutamic acid, 3-nitrobenzoic acid, acetylsalicylic, p-toluic acid, calcium-L-lactate, calcium gluconate, magnesium-DL- aspartate, and magnesium-L-lactate in water. J Chem Thermodyn. 2002;34:1127–36.
Krug RR, Hunter WG, Grieger RS. Enthalpy-entropy compensation. 2. Separation 5 of the chemical from the statistic effect. J Phys Chem. 1976;80:2341–51.
Tao M, Wang Z, Gong J, Hao H, Wang J. Determination of the solubility, dissolution enthalpy, and entropy of pioglitazone hydrochloride (form II) in different pure solvents. Ind Eng Chem Res. 2013;52(8):3036–41.
Holguín AR, Rodríguez GA, Cristancho DM, Delgado DR, Martínez F. Solution thermodynamics of indomethacin in propylene glycol + water mixtures. Fluid Phase Equilib. 2012;314:134–9.
Akhtari H, Bazzaz BF, Golmohammadzadeh S, Movaffagh J, Soheili V, Khameneh B. Rifampin and cis-2-decenoic acid co-entrapment in solid lipid nanoparticles as an efficient nanosystem with potent anti-biofilm activities. J Pharm Innov. 2020. https://doi.org/10.1007/s12247-020-09446-0.
Henwood SQ, Liebenberg W, Tiedt LR, Lötter AP, de Villiers MM. Characterization of the solubility and dissolution properties of several new rifampicin polymorphs, solvates, and hydrates. Drug Dev Ind Pharm. 2001;27(10):1017–30.
Pelizza G, Nebuloni M, Ferrari P, Gallo GG. Polymorphism of rifampicin. Il Farmaco. 1977;32:471–81.
Mohammad MA, Alhalaweh A, Velaga SP. Hansen solubility parameter as a tool 5 to predict cocrystal formation. Int J Pharm. 2011;407:63–71.
Alanazi A, Alshehri S, Altamimi M, Shakeel F. Solubility determination and three dimensional Hansen solubility parameters of gefitinib in different organic solvents: experimental and computational approaches. J Mol Liq. 2020;299. https://doi.org/10.1016/j.molliq.2019.112211.
Guner A. The algorithmic calculations of solubility parameter for the determination of interactions in dextran/certain polar solvent systems. Eur Polym J. 2004;40:1587–94.
Etman MA, Naggar VF. Thermodynamics of paracetamol solubility in sugar-water cosolvent systems. Int J Pharm. 1999;58:177–84.
www.sciencedirect.com. Rifampin. Tuberculosis. 2008;88(2):151–154.
Trevaskis NL, Charman WN, Porter CJH. Lipid-based delivery systems and intestinal lymphatic drug transport: a mechanistic update. Adv Drug Deliv Rev. 2008;60:702–16.
Atrigel® for subcutaneous delivery. A pharmacology review. NDA number 21-343. US FDA review leaflet. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2002/21-343_Eligard_pharmr.pdf.
Ursin C, Hansen CM, Van Dyk JW, Jensen PO, Christensen IJ, Ebbehoej J. Permeability of commercial solvents through living human skin. Am Ind Hyg Assoc J. 1995;56:651–60.
World Health Organization (WHO). Concise international chemical assessment document 39. N-Methyl-2-pyrrolidone. WHO, Geneva; 2001.
Acknowledgement
“The authors would like to thank the Deanship of Scientific Research at King Saud University for supporting this study through research group project number (RG-1441-443)”.
Author information
Authors and Affiliations
Contributions
Wael A. Mahdi: conceptualization and funding acquisition, Afzal Hussain: methodology and writing—original draft and review, Mohammad A. Altamimi: software and data curation, Sultan Alshehri: data curation, Sarah I Bukhari: formal review, Mohd. Neyaz Ahsan: software and analysis.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mahdi, W.A., Hussain, A., Altamimi, M.A. et al. Experimental Solubility, Thermodynamic/Computational Validations, and GastroPlus-Based In Silico Prediction for Subcutaneous Delivery of Rifampicin. AAPS PharmSciTech 22, 116 (2021). https://doi.org/10.1208/s12249-021-01987-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-021-01987-y