Abstract
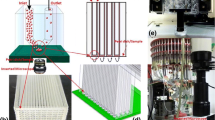
Static in vitro cell culture studies cannot capture the dynamic concentration profiles of drugs, nutrients, and other factors that cells experience in physiological systems. This limits the confidence in the translational relevance of in vitro experiments and increases the reliance on empirical testing of exposure-response relationships and dose optimization in animal models during preclinical drug development, introducing additional challenges owing to species-specific differences in drug pharmacokinetics (PK) and pharmacodynamics (PD). Here, we describe the development of a microfluidic cell culture device that enables perfusion of cells under 2D or 3D culture conditions with temporally programmable concentration profiles. Proof-of-concept studies using doxorubicin and gemcitabine demonstrated the ability of the microfluidic PK-PD device to examine dose- and time-dependent effects of doxorubicin as well as schedule-dependent effects of doxorubicin and gemcitabine combination therapy on cell viability using both step-wise drug concentration profiles and species-specific (i.e., mouse, human) drug PK profiles. The results demonstrate the importance of including physiologically relevant dynamic drug exposure profiles during in vitro drug testing to more accurately mimic in vivo drug effects, thereby improving translatability across nonclinical studies and reducing the reliance on animal models during drug development.






Similar content being viewed by others
References
Gabrielsson J, Fjellstrom O, Ulander J, Rowley M, H. Van Der Graaf P. Pharmacodynamic-pharmacokinetic integration as a guide to medicinal chemistry. Curr Top Med Chem. 2011;11(4):404–18.
Yamazaki S. Translational pharmacokinetic-pharmacodynamic modeling from nonclinical to clinical development: a case study of anticancer drug, crizotinib. AAPS J. 2012;15(2):354–66.
Tuntland T, Ethell B, Kosaka T, Blasco F, Zang RX, Jain M, et al. Implementation of pharmacokinetic and pharmacodynamic strategies in early research phases of drug discovery and development at Novartis Institute of Biomedical Research. Front Pharmacol. 2014;5:174.
Garralda E, Dienstmann R, Tabernero J. Pharmacokinetic/pharmacodynamic modeling of drug development in oncology. Am Soc Clin Oncol Educ Book. 2018;37:210–5.
Mak IW, Evaniew N, Ghert M. Lost in translation: animal models and clinical trials in cancer treatment. Am J Transl Res. 2014;6(2):114–8.
Smith MA, Houghton P. A proposal regarding reporting of in vitro testing results. Clin Cancer Res. 2013;19(11):2828–33.
Lieu CH, Tan A-C, Leong S, Diamond JR, Eckhardt SG. From bench to bedside: lessons learned in translating preclinical studies in cancer drug development. J Natl Cancer Inst. 2013;105(19):1441–56.
Liston DR, Davis M. Clinically relevant concentrations of anticancer drugs: a guide for nonclinical studies. Clin Cancer Res. 2017;23(14):3489–98.
Spilker ME, Chen X, Visswanathan R, Vage C, Yamazaki S, Li G, et al. Found in translation: maximizing the clinical relevance of nonclinical oncology studies. Clin Cancer Res. 2017;23(4):1080–90.
Bartlett R, Everett W, Lim S, Natasha G, Loizidou M, Jell G, et al. Personalized in vitro cancer modeling - fantasy or reality? Transl Oncol. 2014;7(6):657–64.
Weigelt B, Lo AT, Park CC, Gray JW, Bissell MJ. HER2 signaling pathway activation and response of breast cancer cells to HER2-targeting agents is dependent strongly on the 3D microenvironment. Breast Cancer Res Treat. 2010;122(1):35–43.
Edmondson R, Broglie JJ, Adcock AF, Yang L. Three-dimensional cell culture systems and their applications in drug discovery and cell-based biosensors. Assay Drug Dev Technol. 2014;12(4):207–18.
Ingber DE. Developmentally inspired human ‘organs on chips’. Development. 2018;145(16).
Maass C, Stokes CL, Griffith LG, Cirit M. Multi-functional scaling methodology for translational pharmacokinetic and pharmacodynamic applications using integrated microphysiological systems (MPS). Integr Biol (Camb). 2017;9(4):290–302.
Watson DE, Hunziker R, Wikswo JP. Fitting tissue chips and microphysiological systems into the grand scheme of medicine, biology, pharmacology, and toxicology. Exp Biol Med (Maywood). 2017;242(16):1559–72.
Prantil-Baun R, Novak R, Das D, Somayaji MR, Przekwas A, Ingber DE. Physiologically based pharmacokinetic and pharmacodynamic analysis enabled by microfluidically linked organs-on-chips. Annu Rev Pharmacol Toxicol. 2018;58:37–64.
Reichel A, Lienau P. Pharmacokinetics in drug discovery: an exposure-centred approach to optimising and predicting drug efficacy and safety. In: Nielsch U, Fuhrmann U, Jaroch S, editors. New approaches to drug discovery. Cham: Springer International Publishing; 2016. p. 235–60.
Yamazaki S, Spilker ME, Vicini P. Translational modeling and simulation approaches for molecularly targeted small molecule anticancer agents from bench to bedside. Expert Opin Drug Metab Toxicol. 2016;12(3):253–65.
Ande A, Vaidya TR, Tran BN, Vicchiarelli M, Brown AN, Ait-Oudhia S. Utility of a novel three-dimensional and dynamic (3DD) cell culture system for PK/PD studies: evaluation of a triple combination therapy at overcoming anti-HER2 treatment resistance in breast cancer. Front Pharmacol. 2018;9:403.
Wu J, Racine F, Wismer MK, Young K, Carr DM, Xiao JC, et al. Exploring the pharmacokinetic/pharmacodynamic relationship of relebactam (MK-7655) in combination with imipenem in a hollow-fiber infection model. Antimicrob Agents Chemother. 2018;62(5).
Sung JH, Kam C, Shuler ML. A microfluidic device for a pharmacokinetic-pharmacodynamic (PK-PD) model on a chip. Lab Chip. 2010;10(4):446–55.
Dhumpa R, Roper MG. Temporal gradients in microfluidic systems to probe cellular dynamics: a review. Anal Chim Acta. 2012;743:9–18.
McAleer CW, Long CJ, Elbrecht D, Sasserath T, Bridges LR, Rumsey JW, et al. Multi-organ system for the evaluation of efficacy and off-target toxicity of anticancer therapeutics. Sci Transl Med. 2019;11(497):eaav1386.
McAleer CW, Pointon A, Long CJ, Brighton RL, Wilkin BD, Bridges LR, et al. On the potential of in vitro organ-chip models to define temporal pharmacokinetic-pharmacodynamic relationships. Sci Rep. 2019;9(1):9619.
Huang Q, Hu X, He W, Zhao Y, Hao S, Wu Q, et al. Fluid shear stress and tumor metastasis. Am J Cancer Res. 2018;8(5):763–77.
Rizvi I, Gurkan UA, Tasoglu S, Alagic N, Celli JP, Mensah LB, et al. Flow induces epithelial-mesenchymal transition, cellular heterogeneity and biomarker modulation in 3D ovarian cancer nodules. Proc Natl Acad Sci. 2013;110(22):E1974.
Choi HY, Yang G-M, Dayem AA, Saha SK, Kim K, Yoo Y, et al. Hydrodynamic shear stress promotes epithelial-mesenchymal transition by downregulating ERK and GSK3β activities. Breast Cancer Res. 2019;21(1):6.
Muller M, Bockenheimer J, Zellenberg U, Klein N, Steger GG, Eichler HG, et al. Relationship between in vivo drug exposure of the tumor interstitium and inhibition of tumor cell growth in vitro: a study in breast cancer patients. Breast Cancer Res Treat. 2000;60(3):211–7.
Bartlett DW, Wu A, Li X, Kraus M, Wang H, Kindt E. Development of an in vivo retrodialysis calibration method using stable isotope labeling to monitor metabolic pathways in the tumor microenvironment via microdialysis. J Pharm Sci. 2019;108(9):3124–9.
Qin D, Xia Y, Whitesides GM. Soft lithography for micro- and nanoscale patterning. Nat Protoc. 2010;5:491.
Paguirigan AL, Beebe DJ. Microfluidics meet cell biology: bridging the gap by validation and application of microscale techniques for cell biological assays. Bioessays. 2008;30(9):811–21.
Zhang Q, Austin RH. Applications of microfluidics in stem cell biology. Bionanoscience. 2012;2(4):277–86.
Velve-Casquillas G, Le Berre M, Piel M, Tran PT. Microfluidic tools for cell biological research. Nano Today. 2010;5(1):28–47.
Immordino ML, Brusa P, Rocco F, Arpicco S, Ceruti M, Cattel L. Preparation, characterization, cytotoxicity and pharmacokinetics of liposomes containing lipophilic gemcitabine prodrugs. J Control Release. 2004;100(3):331–46.
Johansen PB. Doxorubicin pharmacokinetics after intravenous and intraperitoneal administration in the nude mouse. Cancer Chemother Pharmacol. 1981;5(4):267–70.
Ishisaka T, Kishi S, Okura K, Horikoshi M, Yamashita T, Mitsuke Y, et al. A precise pharmacodynamic study showing the advantage of a marked reduction in cardiotoxicity in continuous infusion of doxorubicin. Leuk Lymphoma. 2006;47(8):1599–607.
Lovitt CJ, Shelper TB, Avery VM. Doxorubicin resistance in breast cancer cells is mediated by extracellular matrix proteins. BMC Cancer. 2018;18(1):41.
Osman A-MM, Bayoumi HM, Al-Harthi SE, Damanhouri ZA, Elshal MF. Modulation of doxorubicin cytotoxicity by resveratrol in a human breast cancer cell line. Cancer Cell Int. 2012;12(1):47.
Vogus DR, Pusuluri A, Chen R, Mitragotri S. Schedule dependent synergy of gemcitabine and doxorubicin: improvement of in vitro efficacy and lack of in vitro-in vivo correlation. Bioeng Transl Med. 2018;3(1):49–57.
Checkley S, MacCallum L, Yates J, Jasper P, Luo H, Tolsma J, et al. Bridging the gap between in vitro and in vivo: dose and schedule predictions for the ATR inhibitor AZD6738. Sci Rep. 2015;5:13545.
Gibbs JP. Prediction of exposure-response relationships to support first-in-human study design. AAPS J. 2010;12(4):750–8.
Bovard D, Sandoz A, Luettich K, Frentzel S, Iskandar A, Marescotti D, et al. A lung/liver-on-a-chip platform for acute and chronic toxicity studies. Lab Chip. 2018;18(24):3814–29.
Mould DR, Walz AC, Lave T, Gibbs JP, Frame B. Developing exposure/response models for anticancer drug treatment: special considerations. CPT Pharmacometrics Syst Pharmacol. 2015;4(1):e00016-e.
Makiyama A, Qin B, Uchino K, Shibata Y, Arita S, Isobe T, et al. Schedule-dependent synergistic interaction between gemcitabine and oxaliplatin in human gallbladder adenocarcinoma cell lines. Anti-Cancer Drugs. 2009;20(2).
Aschele C, Baldo C, Sobrero AF, Debernardis D, Bornmann WG, Bertino JR. Schedule-dependent synergism between raltitrexed and irinotecan in human colon cancer cells in vitro. Clin Cancer Res. 1998;4(5):1323–30.
Van der Veldt AAM, Lammertsma AA, Smit EF. Scheduling of anticancer drugs: timing may be everything. Cell Cycle. 2012;11(23):4339–43.
Fujimoto-Ouchi K, Tanaka Y, Tominaga T. Schedule dependency of antitumor activity in combination therapy with capecitabine/5′-deoxy-5-fluorouridine and docetaxel in breast Cancer models. Clin Cancer Res. 2001;7(4):1079–86.
Eduati F, Utharala R, Madhavan D, Neumann UP, Longerich T, Cramer T, et al. A microfluidics platform for combinatorial drug screening on cancer biopsies. Nat Commun. 2018;9(1):2434.
Funding
Financial support: Pfizer, Inc.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of Interest
YAG, DD, CS, and DS are employees of Neofluidics. EK, MES, TM, and DWB are employees of Pfizer.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(PDF 1144 kb)
Rights and permissions
About this article
Cite this article
Guerrero, Y.A., Desai, D., Sullivan, C. et al. A Microfluidic Perfusion Platform for In Vitro Analysis of Drug Pharmacokinetic-Pharmacodynamic (PK-PD) Relationships. AAPS J 22, 53 (2020). https://doi.org/10.1208/s12248-020-0430-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-020-0430-y