Abstract
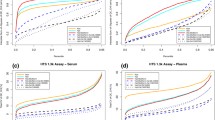
Blood-based soluble protein biomarkers provide invaluable clinical information about patients and are used as diagnostic, prognostic, and pharmacodynamic markers. The most commonly used blood sample matrices are serum and different types of plasma. In drug development research, the impact of sample matrix selection on successful protein biomarker quantification is sometimes overlooked. The sample matrix for a specific analyte is often chosen based on prior experience or literature searches, without good understanding of the possible effects on analyte quantification. Using a data set of 32 different soluble protein markers measured in matched serum and plasma samples, we examined the differences between serum and plasma and discussed how platelet or immune cell activation can change the quantified concentration of the analyte. We have also reviewed the effect of anticoagulant on analyte quantification. Finally, we provide specific recommendations for biomarker sample matrix selection and propose a systematic and data-driven approach for sample matrix selection. This review is intended to raise awareness of the impact and considerations of sample matrix selection on biomarker quantification.

Similar content being viewed by others
References
Ladenson JH, Tsai L-MB, Michael JM, Kessler G, Joist JH. Serum versus heparinized plasma for eighteen common chemistry tests: is serum the appropriate specimen? Am J Clin Pathol. 1974;62(4):545–52.
Miles RR, Roberts RF, Putnam AR, Roberts WL. Comparison of serum and heparinized plasma samples for measurement of chemistry analytes. Clin Chem. 2004;50(9):1704–6.
Dupin M, Fortin T, Larue-Triolet A, Surault I, Beaulieu C, Gouel-Chéron A, et al. Impact of serum and plasma matrices on the titration of human inflammatory biomarkers using analytically validated SRM assays. J Proteome Res. 2016;15(8):2366–78.
Jung K, Laube C, Lein M, Lichtinghagen R, Tschesche H, Schnorr D, et al. Kind of sample as preanalytical determinant of matrix metalloproteinases 2 and 9 and tissue inhibitor of metalloproteinase 2 in blood. Clin Chem. 1998;44(5):1060–2.
Scholman RC, Giovannone B, Hiddingh S, Meerding JM, Malvar Fernandez B, van Dijk MEA, et al. Effect of anticoagulants on 162 circulating immune related proteins in healthy subjects. Cytokine. 2018;106:114–24.
Biancotto A, Feng X, Langweiler M, Young NS, McCoy JP. Effect of anticoagulants on multiplexed measurement of cytokine/chemokines in healthy subjects. Cytokine. 2012;60(2):438–46.
Brondum L, Sorensen BS, Eriksen JG, Mortensen LS, Lonbro S, Overgaard J, et al. An evaluation of multiplex bead-based analysis of cytokines and soluble proteins in archived lithium heparin plasma, EDTA plasma and serum samples. Scand J Clin Lab Invest. 2016;76(8):601–11.
Tvedt TH, Rye KP, Reikvam H, Brenner AK, Bruserud O. The importance of sample collection when using single cytokine levels and systemic cytokine profiles as biomarkers--a comparative study of serum versus plasma samples. J Immunol Methods. 2015;418:19–28.
Keustermans GC, Hoeks SB, Meerding JM, Prakken BJ, de Jager W. Cytokine assays: an assessment of the preparation and treatment of blood and tissue samples. Methods. 2013;61(1):10–7.
Thavasu PW, Longhurst S, Joel SP, Slevin ML, Balkwill FR. Measuring cytokine levels in blood. Importance of anticoagulants, processing, and storage conditions. J Immunol Methods. 1992;153(1–2):115–24.
Hennø LT, Storjord E, Christiansen D, Bergseth G, Ludviksen JK, Fure H, et al. Effect of the anticoagulant, storage time and temperature of blood samples on the concentrations of 27 multiplex assayed cytokines – consequences for defining reference values in healthy humans. Cytokine. 2017;97:86–95.
O’Neal WK, Anderson W, Basta PV, Carretta EE, Doerschuk CM, Barr RG, et al. of serum, EDTA plasma and P100 plasma for luminex-based biomarker multiplex assays in patients with chronic obstructive pulmonary disease in the SPIROMICS study. J Transl Med. 2014;12(1):9.
de Jager W, Bourcier K, Rijkers GT, Prakken BJ, Seyfert-Margolis V. Prerequisites for cytokine measurements in clinical trials with multiplex immunoassays. BMC Immunol. 2009;10(1):52.
Lan J, Nunez Galindo A, Doecke J, Fowler C, Martins RN, Rainey-Smith SR, et al. Systematic evaluation of the use of human plasma and serum for mass-spectrometry-based shotgun proteomics. J Proteome Res. 2018;17(4):1426–35.
Ilies M, Iuga CA, Loghin F, Dhople VM, Thiele T, Völker U, et al. Data on the impact of the blood sample collection methods on blood protein profiling studies. Data Brief. 2017;14:313–9.
Organization WH. Use of anticoagulants in diagnostic laboratory investigations. 2nd ed. Geneva: World Health Organization; 2002.
Nossel HL. Differential consumption of coagulation factors resulting from activation of the extrinsic (tissue thromboplastin) or the intrinsic (foreign surface contact) pathways. Blood. 1967;29(3):331–40.
Carey RN, Jani C, Johnson C, Pearce J, Hui-Ng P, Lacson E. Chemistry testing on plasma versus serum samples in dialysis patients: clinical and quality improvement implications. Clin J Am Soc Nephrol. 2016;11(9):1675–9.
Smith SA, Travers RJ, Morrissey JH. How it all starts: initiation of the clotting cascade. Crit Rev Biochem Mol Biol. 2015;50(4):326–36.
Machlus KR, Johnson KE, Kulenthirarajan R, Forward JA, Tippy MD, Soussou TS, et al. CCL5 derived from platelets increases megakaryocyte proplatelet formation. Blood. 2016;127(7):921–6.
Power CA, Clemetson JM, Clemetson KJ, Wells TNC. Chemokine and chemokine receptor mRNA expression in human platelets. Cytokine. 1995;7(6):479–82.
Zhao X, Delgado L, Weiner R, Laterza OF. Influence of pre-analytical factors on thymus- and activation-regulated chemokine quantitation in plasma. J Circ Biomark. 2015;4:10.
Assoian RK, Sporn MB. Type beta transforming growth factor in human platelets: release during platelet degranulation and action on vascular smooth muscle cells. J Cell Biol. 1986;102(4):1217–23.
Otterdal K, Smith C, Øie E, Pedersen TM, Yndestad A, Stang E, et al. Platelet-derived LIGHT induces inflammatory responses in endothelial cells and monocytes. Blood. 2006;108(3):928–35.
Severin IC, Gaudry JP, Johnson Z, Kungl A, Jansma A, Gesslbauer B, et al. Characterization of the chemokine CXCL11-heparin interaction suggests two different affinities for glycosaminoglycans. J Biol Chem. 2010;285(23):17713–24.
Mei J, Liu Y, Dai N, Favara M, Greene T, Jeyaseelan S, et al. CXCL5 regulates chemokine scavenging and pulmonary host defense to bacterial infection. Immunity. 2010;33(1):106–17.
Salanga CL, Dyer DP, Kiselar JG, Gupta S, Chance MR, Handel TM. Multiple glycosaminoglycan-binding epitopes of monocyte chemoattractant protein-3/CCL7 enable it to function as a non-oligomerizing chemokine. J Biol Chem. 2014;289(21):14896–912.
Seo Y, Schenauer MR, Leary JA. Biologically relevant metal-cation binding induces conformational changes in heparin oligosaccharides as measured by ion mobility mass spectrometry. Int J Mass Spectrom. 2011;303(2–3):191–8.
Visse R, Nagase H. Matrix metalloproteinases and tissue inhibitors of metalloproteinases. Circ Res. 2003;92(8):827–39.
Tallant C, Marrero A, Gomis-Rüth FX. Matrix metalloproteinases: fold and function of their catalytic domains. Biochim Biophys Acta. 2010;1803(1):20–8.
Tezvergil-Mutluay A, Agee KA, Hoshika T, Carrilho M, Breschi L, Tjäderhane L, et al. The requirement of zinc and calcium ions for functional MMP activity in demineralized dentin matrices. Dent Mater. 2010;26(11):1059–67.
Paula K, Anne T-M, Taina T-H. The sample type used affects the levels of gelatinases (MMP-2 and -9) and their inhibitors (TIMP-1 and -2) in circulating blood of healthy controls and breast cancer patients. Biomark Insights. 2007;2:117–27.
John M, Jung K. Pre-analytical conditions for the assessment of circulating MMP-9 and TIMP-1: consideration of pitfalls. Eur Respir J. 2005;26(2):364–5.
Gerlach RF, Uzuelli JA, Souza-Tarla CD, Tanus-Santos JE. Effect of anticoagulants on the determination of plasma matrix metalloproteinase (MMP)-2 and MMP-9 activities. Anal Biochem. 2005;344(1):147–9.
Fischer JE, Janousek M, Fischer M, Seifarth FG, Blau N, Fanconi S. Effect of collection and preprocessing methods on neutrophil elastase plasma concentrations. Clin Biochem. 1998;31(3):131–6.
Beatty K, Bieth J, Travis J. Kinetics of association of serine proteinases with native and oxidized alpha-1-proteinase inhibitor and alpha-1-antichymotrypsin. J Biol Chem. 1980;255(9):3931–4.
Frommherz KJ, Faller B, Bieth JG. Heparin strongly decreases the rate of inhibition of neutrophil elastase by alpha 1-proteinase inhibitor. J Biol Chem. 1991;266(23):15356–62.
Ellyard JI, Simson L, Bezos A, Johnston K, Freeman C, Parish CR. Eotaxin selectively binds heparin: an interaction that protects eotaxin from proteolysis and potentiates chemotactic activity in vivo. J Biol Chem. 2007;282(20):15238–47.
Cedrone E, Neun BW, Rodriguez J, Vermilya A, Clogston JD, McNeil SE, et al. Anticoagulants influence the performance of in vitro assays intended for characterization of nanotechnology-based formulations. Molecules. 2017;23(1).
Ray CA. Biomarker accuracy: exploring the truth. Bioanalysis. 2014;6(3):269–71.
Smyth SS, McEver RP, Weyrich AS, Morrell CN, Hoffman MR, Arepally GM, et al. Platelet functions beyond hemostasis. J Thromb Haemost. 2009;7(11):1759–66.
Burkhart JM, Gambaryan S, Watson SP, Jurk K, Walter U, Sickmann A, et al. What can proteomics tell us about platelets? Circ Res. 2014;114(7):1204–19.
Fong KP, Barry C, Tran AN, Traxler EA, Wannemacher KM, Tang H-Y, et al. Deciphering the human platelet sheddome. Blood. 2011;117(1):e15–26.
Senzel L, Gnatenko DV, Bahou WF. The platelet proteome. Curr Opin Hematol. 2009;16(5):329–33.
Coppinger JA, Cagney G, Toomey S, Kislinger T, Belton O, McRedmond JP, et al. Characterization of the proteins released from activated platelets leads to localization of novel platelet proteins in human atherosclerotic lesions. Blood. 2004;103(6):2096–104.
Kong F-MS, Zhao L, Wang L, Chen Y, Hu J, Fu X, et al. Ensuring sample quality for blood biomarker studies in clinical trials: a multicenter international study for plasma and serum sample preparation. Transl Lung Cancer Res. 2017;6(6):625–34.
Jonnalagadda D, Izu LT, Whiteheart SW. Platelet secretion is kinetically heterogeneous in an agonist-responsive manner. Blood. 2012;120(26):5209–16.
Ding D, Liu X, Duan J, Guo S-W. Platelets are an unindicted culprit in the development of endometriosis: clinical and experimental evidence. Hum Reprod. 2015;30(4):812–32.
Gresele P, Fuster V, Lopez JA, Page CP, Vermylen J, editors. Platelets in hematologic and cardiovascular disorders. 1st ed: Cambridge University Press; 2008.
Peterson JE, Zurakowski D, Italiano JE, Michel LV, Fox L, Klement GL, et al. Normal ranges of angiogenesis regulatory proteins in human platelets. Am J Hematol. 2010;85(7):487–93.
Halldórsdóttir AM, Stoker J, Porche-Sorbet R, Eby CS. Soluble CD40 ligand measurement inaccuracies attributable to specimen type, processing time, and ELISA method. Clin Chem. 2005;51(6):1054–7.
Zhao X, Delgado L, Weiner R, Laterza OF. An ultra-sensitive clinical biomarker assay: quantitation of thymus and activation-regulated chemokine in human plasma. Bioanalysis. 2014;6(8):1069–80.
Wakefield LM, Letterio JJ, Chen T, Danielpour D, Allison RS, Pai LH, et al. Transforming growth factor-beta1 circulates in normal human plasma and is unchanged in advanced metastatic breast cancer. Clin Cancer Res. 1995;1(1):129–36.
O’Brien PJ, Ramanathan R, Yingling JM, Baselga J, Rothenberg ML, Carducci M, et al. Analysis and variability of TGFbeta measurements in cancer patients with skeletal metastases. Biologics. 2008;2(3):563–9.
Swystun LL, Liaw PC. The role of leukocytes in thrombosis. Blood. 2016;128(6):753–62.
von Brühl M-L, Stark K, Steinhart A, Chandraratne S, Konrad I, Lorenz M, et al. Monocytes, neutrophils, and platelets cooperate to initiate and propagate venous thrombosis in mice in vivo. J Exp Med. 2012;209(4):819.
Kambas K, Mitroulis I, Ritis K. The emerging role of neutrophils in thrombosis-the journey of TF through NETs. Front Immunol. 2012;3:385.
Weisel JW, Litvinov RI. Red blood cells: the forgotten player in hemostasis and thrombosis. J Thromb Haemost. 2019;17(2):271–82.
Smiley ST, King JA, Hancock WW. Fibrinogen stimulates macrophage chemokine secretion through toll-like receptor 4. J Immunol. 2001;167(5):2887.
Parkitny L, McAuley JH, Kelly PJ, Di Pietro F, Cameron B, Moseley GL. Multiplex cytokine concentration measurement: how much do the medium and handling matter? Mediat Inflamm. 2013;2013:13.
Ryu JK, Petersen MA, Murray SG, Baeten KM, Meyer-Franke A, Chan JP, et al. Blood coagulation protein fibrinogen promotes autoimmunity and demyelination via chemokine release and antigen presentation. Nat Commun. 2015;6:8164.
Koller DY. Sampling methods. Am J Respir Crit Care Med. 2000;162(supplement_1):S31–S3.
Jonsson A, Hjalmarsson C, Falk P, Ivarsson M-L. Levels of matrix metalloproteinases differ in plasma and serum - aspects regarding analysis of biological markers in cancer. Br J Cancer. 2016;115(6):703–6.
Freitas M, Porto G, Lima JLFC, Fernandes E. Isolation and activation of human neutrophils in vitro. The importance of the anticoagulant used during blood collection. Clin Biochem. 2008;41(7):570–5.
Lee JW, Devanarayan V, Barrett YC, Weiner R, Allinson J, Fountain S, et al. Fit-for-purpose method development and validation for successful biomarker measurement. Pharm Res. 2006;23(2):312–28.
Booth B, Arnold ME, DeSilva B, Amaravadi L, Dudal S, Fluhler E, et al. Workshop report: Crystal City V--quantitative bioanalytical method validation and implementation: the 2013 revised FDA guidance. AAPS J. 2014;17(2):277–88.
Arnold ME, Booth B, King L, Ray C. Workshop report: Crystal City VI—bioanalytical method validation for biomarkers. AAPS J. 2016;18(6):1366–72.
Piccoli SP, Garofolo F. Biomarker assay validation. Bioanalysis. 2018;10(12):889–91.
Bowen RAR, Remaley AT. Interferences from blood collection tube components on clinical chemistry assays. Biochemia Med. 2014;24(1):31–44.
Acknowledgments
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mathews, J.A., Ni, Y.G., Wang, C. et al. Considerations for Soluble Protein Biomarker Blood Sample Matrix Selection. AAPS J 22, 38 (2020). https://doi.org/10.1208/s12248-020-0412-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-020-0412-0