Abstract
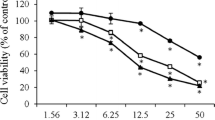
Nuclear factor erythroid-2-related factor-2 (Nrf2 or NFE2L2) is a master regulator of the anti-oxidative stress response, which is involved in the defense against many oxidative stress/inflammation-mediated diseases, including anticancer effects elicited by an increasing number of natural products. Our previous studies showed that the epigenetic modification of the Nrf2 gene plays a key role in restoring the expression of Nrf2. In this study, we aimed to investigate the epigenetic regulation of Nrf2 by astaxanthin (AST) and fucoxanthin (FX), carotenoids which are abundant in microalgae and seaweeds, in mouse skin epidermal JB6 P+ cells. FX induced the anti-oxidant response element (ARE)-luciferase and upregulated the mRNA and protein levels of Nrf2 and Nrf2 downstream genes in HepG2-C8 cells overexpressing the ARE-luciferase reporter. Both FX and AST decreased colony formation in 12-Otetradecanoylphorbol-13-acetate (TPA)-induced transformation of JB6 P+ cells. FX decreased the methylation of the Nrf2 promoter region in the JB6 P+ cells by the bisulfite conversion and pyrosequencing. Both FX and AST significantly reduced DNA methyltransferase (DNMT) activity but did not affect histone deacetylase (HDAC) activity in JB6 P+ cells. In summary, our results show that FX activates the Nrf2 signaling pathway, induces the epigenetic demethylation of CpG sites in Nrf2 and blocks the TPA-induced transformation of JB6 P+ cells, indicating the potential health-promoting effects of FX in skin cancer prevention.









Similar content being viewed by others
Abbreviations
- ARE:
-
Anti-oxidant response element
- AST:
-
Astaxanthin
- 5-aza:
-
5-aza-deoxycytidine
- DNMT:
-
DNA methyltransferase
- DNMT1:
-
DNA methyltransferase 1
- DNMT3a:
-
DNA methyltransferase 3a
- DNMT3b:
-
DNA methyltransferase 3b
- DMSO:
-
Dimethyl sulfoxide
- FBS:
-
Fetal bovine serum
- FX:
-
Fucoxanthin
- GCLC:
-
Glutamate-Cysteine Ligase, Catalytic Subunit
- GSH:
-
Glutathione
- GSS:
-
Glutathione synthetase
- GST:
-
Glutathione-S-transferases
- GAPDH:
-
Glyceraldehyde 3-phosphate dehydrogenase
- HO-1:
-
Heme oxygenase-1
- HDAC:
-
Histone deacetylases
- NQO1:
-
NAD(P)H: quinone oxidoreductase 1
- Nrf2:
-
Nuclear factor (erythroid-derived 2)-like 2, or NFE2L2
- qRT–PCR:
-
Quantitative reverse-transcriptase polymerase chain reaction
- ROS:
-
Reactive oxygen species; SEM, standard error of the mean
References
Alam M, Ratner D. Cutaneous squamous-cell carcinoma. N Engl J Med. 2001;344(13):975–83. https://doi.org/10.1056/NEJM200103293441306.
McGuire S. World cancer report 2014. Geneva, Switzerland: World Health Organization, International Agency for Research on Cancer, WHO press, 2015. Adv Nutr. 2016;7(2):418–9. https://doi.org/10.3945/an.116.012211.
Griffin LL, Ali FR, Lear JT. Non-melanoma skin cancer. Clin Med. 2016;16(1):62–5. https://doi.org/10.7861/clinmedicine.16-1-62.
Singh RP, Agarwal R. Mechanisms and preclinical efficacy of silibinin in preventing skin cancer. Eur J Cancer. 2005;41(13):1969–79. https://doi.org/10.1016/j.ejca.2005.03.033.
Xu C, Huang MT, Shen G, Yuan X, Lin W, Khor TO, et al. Inhibition of 7,12-dimethylbenz(a)anthracene-induced skin tumorigenesis in C57BL/6 mice by sulforaphane is mediated by nuclear factor E2-related factor 2. Cancer Res. 2006;66(16):8293–6. https://doi.org/10.1158/0008-5472.CAN-06-0300.
Huang MT, Xie JG, Wang ZY, Ho CT, Lou YR, Wang CX, et al. Effects of tea, decaffeinated tea, and caffeine on UVB light-induced complete carcinogenesis in SKH-1 mice: demonstration of caffeine as a biologically important constituent of tea. Cancer Res. 1997;57(13):2623–9.
Huang MT, Smart RC, Wong CQ, Conney AH. Inhibitory effect of curcumin, chlorogenic acid, caffeic acid, and ferulic acid on tumor promotion in mouse skin by 12-O-tetradecanoylphorbol-13-acetate. Cancer Res. 1988;48(21):5941–6.
Conney AH, Wang ZY, Huang MT, Ho CT, Yang CS. Inhibitory effect of green tea on tumorigenesis by chemicals and ultraviolet light. Prev Med. 1992;21(3):361–9. https://doi.org/10.1016/0091-7435(92)90043-H.
Huang MT, Ho CT, Wang ZY, Ferraro T, Lou YR, Stauber K, et al. Inhibition of skin tumorigenesis by rosemary and its constituents carnosol and ursolic acid. Cancer Res. 1994;54(3):701–8.
Talalay P. Chemoprotection against cancer by induction of phase 2 enzymes. Biofactors. 2000;12(1–4):5–11. https://doi.org/10.1002/biof.5520120102.
Dinkova-Kostova AT, Jenkins SN, Fahey JW, Ye L, Wehage SL, Liby KT, et al. Protection against UV-light-induced skin carcinogenesis in SKH-1 high-risk mice by sulforaphane-containing broccoli sprout extracts. Cancer Lett. 2006;240(2):243–52. https://doi.org/10.1016/j.canlet.2005.09.012.
Sigalotti L, Fratta E, Coral S, Cortini E, Covre A, Nicolay HJ, et al. Epigenetic drugs as pleiotropic agents in cancer treatment: biomolecular aspects and clinical applications. J Cell Physiol. 2007;212(2):330–44. https://doi.org/10.1002/jcp.21066.
Golabek K, Strzelczyk JK, Wiczkowski A, Michalski M. Potential use of histone deacetylase inhibitors in cancer therapy. Contemp Oncol (Pozn). 2015;19(6):436–40. https://doi.org/10.5114/wo.2015.51824.
van Doorn R, Gruis NA, Willemze R, van der Velden PA, Tensen CP. Aberrant DNA methylation in cutaneous malignancies. Semin Oncol. 2005;32(5):479–87. https://doi.org/10.1053/j.seminoncol.2005.07.001.
Bachman AN, Curtin GM, Doolittle DJ, Goodman JI. Altered methylation in gene-specific and GC-rich regions of DNA is progressive and nonrandom during promotion of skin tumorigenesis. Toxicol Sci. 2006;91(2):406–18. https://doi.org/10.1093/toxsci/kfj179.
Schinke C, Mo Y, Yu Y, Amiri K, Sosman J, Greally J, et al. Aberrant DNA methylation in malignant melanoma. Melanoma Res. 2010;20(4):253–65. https://doi.org/10.1097/CMR.0b013e328338a35a.
Yang AY, Lee JH, Shu L, Zhang C, Su ZY, Lu Y, et al. Genome-wide analysis of DNA methylation in UVB- and DMBA/TPA-induced mouse skin cancer models. Life Sci. 2014;113(1–2):45–54. https://doi.org/10.1016/j.lfs.2014.07.031.
Yang CS, Fang M, Lambert JD, Yan P, Huang TH. Reversal of hypermethylation and reactivation of genes by dietary polyphenolic compounds. Nutr Rev. 2008;66(Suppl 1):S18–20. https://doi.org/10.1111/j.1753-4887.2008.00059.x.
Yang AY, Kim H, Li W, Kong AN. Natural compound-derived epigenetic regulators targeting epigenetic readers, writers and erasers. Curr Top Med Chem. 2016;16(7):697–713.
Wang LG, Beklemisheva A, Liu XM, Ferrari AC, Feng J, Chiao JW. Dual action on promoter demethylation and chromatin by an isothiocyanate restored GSTP1 silenced in prostate cancer. Mol Carcinog. 2007;46(1):24–31. https://doi.org/10.1002/mc.20258.
Wang LG, Liu XM, Fang Y, Dai W, Chiao FB, Puccio GM, et al. De-repression of the p21 promoter in prostate cancer cells by an isothiocyanate via inhibition of HDACs and c-Myc. Int J Oncol. 2008;33(2):375–80.
Nian H, Delage B, Ho E, Dashwood RH. Modulation of histone deacetylase activity by dietary isothiocyanates and allyl sulfides: studies with sulforaphane and garlic organosulfur compounds. Environ Mol Mutagen. 2009;50(3):213–21. https://doi.org/10.1002/em.20454.
Myzak MC, Tong P, Dashwood WM, Dashwood RH, Ho E. Sulforaphane retards the growth of human PC-3 xenografts and inhibits HDAC activity in human subjects. Exp Biol Med. 2007;232(2):227–34.
Meeran SM, Patel SN, Tollefsbol TO. Sulforaphane causes epigenetic repression of hTERT expression in human breast cancer cell lines. PLoS One. 2010;5(7):e11457. https://doi.org/10.1371/journal.pone.0011457.
Su ZY, Zhang C, Lee JH, Shu L, Wu TY, Khor TO, et al. Requirement and epigenetics reprogramming of Nrf2 in suppression of tumor promoter TPA-induced mouse skin cell transformation by sulforaphane. Cancer Prev Res (Phila). 2014;7(3):319–29. https://doi.org/10.1158/1940-6207.CAPR-13-0313-T.
Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357(9255):539–45. https://doi.org/10.1016/S0140-6736(00)04046-0.
Lund AW, Medler TR, Leachman SA, Coussens LM. Lymphatic vessels, inflammation, and immunity in skin cancer. Cancer Discov. 2016;6(1):22–35. https://doi.org/10.1158/2159-8290.CD-15-0023.
Singh R, Akhtar N, Haqqi TM. Green tea polyphenol epigallocatechin-3-gallate: inflammation and arthritis. [corrected]. Life Sci. 2010;86(25–26):907–18. https://doi.org/10.1016/j.lfs.2010.04.013.
Singh S, Vrishni S, Singh BK, Rahman I, Kakkar P. Nrf2-ARE stress response mechanism: a control point in oxidative stress-mediated dysfunctions and chronic inflammatory diseases. Free Radic Res. 2010;44(11):1267–88. https://doi.org/10.3109/10715762.2010.507670.
Hu R, Saw CL, Yu R, Kong AN. Regulation of NF-E2-related factor 2 signaling for cancer chemoprevention: antioxidant coupled with antiinflammatory. Antioxid Redox Signal. 2010;13(11):1679–98. https://doi.org/10.1089/ars.2010.3276.
Kong AN, Yu R, Lei W, Mandlekar S, Tan TH, Ucker DS. Differential activation of MAPK and ICE/Ced-3 protease in chemical-induced apoptosis. The role of oxidative stress in the regulation of mitogen-activated protein kinases (MAPKs) leading to gene expression and survival or activation of caspases leading to apoptosis. Restor Neurol Neurosci. 1998;12(2–3):63–70.
Itoh K, Wakabayashi N, Katoh Y, Ishii T, Igarashi K, Engel JD, et al. Keap1 represses nuclear activation of antioxidant responsive elements by Nrf2 through binding to the amino-terminal Neh2 domain. Genes Dev. 1999;13(1):76–86. https://doi.org/10.1101/gad.13.1.76.
Lee JH, Khor TO, Shu L, Su ZY, Fuentes F, Kong AN. Dietary phytochemicals and cancer prevention: Nrf2 signaling, epigenetics, and cell death mechanisms in blocking cancer initiation and progression. Pharmacol Ther. 2013;137(2):153–71. https://doi.org/10.1016/j.pharmthera.2012.09.008.
Suzuki T, Motohashi H, Yamamoto M. Toward clinical application of the Keap1-Nrf2 pathway. Trends Pharmacol Sci. 2013;34(6):340–6. https://doi.org/10.1016/j.tips.2013.04.005.
Khor TO, Huang MT, Prawan A, Liu Y, Hao X, Yu S, et al. Increased susceptibility of Nrf2 knockout mice to colitis-associated colorectal cancer. Cancer Prev Res (Phila). 2008;1(3):187–91. https://doi.org/10.1158/1940-6207.CAPR-08-0028.
Saw CL, Yang AY, Huang MT, Liu Y, Lee JH, Khor TO, et al. Nrf2 null enhances UVB-induced skin inflammation and extracellular matrix damages. Cell Biosci. 2014;4(1):39. https://doi.org/10.1186/2045-3701-4-39.
Saw CL, Huang MT, Liu Y, Khor TO, Conney AH, Kong AN. Impact of Nrf2 on UVB-induced skin inflammation/photoprotection and photoprotective effect of sulforaphane. Mol Carcinog. 2011;50(6):479–86. https://doi.org/10.1002/mc.20725.
Gills JJ, Jeffery EH, Matusheski NV, Moon RC, Lantvit DD, Pezzuto JM. Sulforaphane prevents mouse skin tumorigenesis during the stage of promotion. Cancer Lett. 2006;236(1):72–9. https://doi.org/10.1016/j.canlet.2005.05.007.
Hu C, Eggler AL, Mesecar AD, van Breemen RB. Modification of keap1 cysteine residues by sulforaphane. Chem Res Toxicol. 2011;24(4):515–21. https://doi.org/10.1021/tx100389r.
Quitain AT, Kai T, Sasaki M, Goto M. Supercritical carbon dioxide extraction of fucoxanthin from Undaria pinnatifida. J Agric Food Chem. 2013;61(24):5792–7. https://doi.org/10.1021/jf400740p.
Gammone MA, D’Orazio N. Anti-obesity activity of the marine carotenoid fucoxanthin. Mar Drugs. 2015;13(4):2196–214. https://doi.org/10.3390/md13042196.
Muradian K, Vaiserman A, Min KJ, Fraifeld VE. Fucoxanthin and lipid metabolism: a minireview. Nutr Metab Cardiovasc Dis. 2015;25(10):891–7. https://doi.org/10.1016/j.numecd.2015.05.010.
Zheng J, Piao MJ, Keum YS, Kim HS, Hyun JW. Fucoxanthin protects cultured human keratinocytes against oxidative stress by blocking free radicals and inhibiting apoptosis. Biomol Ther (Seoul). 2013;21(4):270–6. https://doi.org/10.4062/biomolther.2013.030.
Zheng J, Piao MJ, Kim KC, Yao CW, Cha JW, Hyun JW. Fucoxanthin enhances the level of reduced glutathione via the Nrf2-mediated pathway in human keratinocytes. Mar Drugs. 2014;12(7):4214–30. https://doi.org/10.3390/md12074214.
Matsui M, Tanaka K, Higashiguchi N, Okawa H, Yamada Y, Tanaka K, et al. Protective and therapeutic effects of fucoxanthin against sunburn caused by UV irradiation. J Pharmacol Sci. 2016;132(1):55–64. https://doi.org/10.1016/j.jphs.2016.08.004.
Urikura I, Sugawara T, Hirata T. Protective effect of fucoxanthin against UVB-induced skin photoaging in hairless mice. Biosci Biotechnol Biochem. 2011;75(4):757–60. https://doi.org/10.1271/bbb.110040.
Aoi W, Naito Y, Sakuma K, Kuchide M, Tokuda H, Maoka T, et al. Astaxanthin limits exercise-induced skeletal and cardiac muscle damage in mice. Antioxid Redox Signal. 2003;5(1):139–44. https://doi.org/10.1089/152308603321223630.
Iwamoto T, Hosoda K, Hirano R, Kurata H, Matsumoto A, Miki W, et al. Inhibition of low-density lipoprotein oxidation by astaxanthin. J Atheroscler Thromb. 2000;7(4):216–22. https://doi.org/10.5551/jat1994.7.216.
Kobayashi M. In vivo antioxidant role of astaxanthin under oxidative stress in the green alga Haematococcus pluvialis. Appl Microbiol Biotechnol. 2000;54(4):550–5. https://doi.org/10.1007/s002530000416.
Peng J, Yuan JP, Wang JH. Effect of diets supplemented with different sources of astaxanthin on the gonad of the sea urchin Anthocidaris crassispina. Nutrients. 2012;4(8):922–34. https://doi.org/10.3390/nu4080922.
Yasui Y, Hosokawa M, Mikami N, Miyashita K, Tanaka T. Dietary astaxanthin inhibits colitis and colitis-associated colon carcinogenesis in mice via modulation of the inflammatory cytokines. Chem Biol Interact. 2011;193(1):79–87. https://doi.org/10.1016/j.cbi.2011.05.006.
Nagendraprabhu P, Sudhandiran G. Astaxanthin inhibits tumor invasion by decreasing extracellular matrix production and induces apoptosis in experimental rat colon carcinogenesis by modulating the expressions of ERK-2, NFkB and COX-2. Investig New Drugs. 2011;29(2):207–24. https://doi.org/10.1007/s10637-009-9342-5.
Jyonouchi H, Sun S, Iijima K, Gross MD. Antitumor activity of astaxanthin and its mode of action. Nutr Cancer. 2000;36(1):59–65. https://doi.org/10.1207/S15327914NC3601_9.
Kang JO, Kim SJ, Kim H. Effect of astaxanthin on the hepatotoxicity, lipid peroxidation and antioxidative enzymes in the liver of CCl4-treated rats. Methods Find Exp Clin Pharmacol. 2001;23(2):79–84. https://doi.org/10.1358/mf.2001.23.2.627931.
Uchiyama K, Naito Y, Hasegawa G, Nakamura N, Takahashi J, Yoshikawa T. Astaxanthin protects beta-cells against glucose toxicity in diabetic db/db mice. Redox Rep. 2002;7(5):290–3. https://doi.org/10.1179/135100002125000811.
Ohgami K, Shiratori K, Kotake S, Nishida T, Mizuki N, Yazawa K, et al. Effects of astaxanthin on lipopolysaccharide-induced inflammation in vitro and in vivo. Invest Ophthalmol Vis Sci. 2003;44(6):2694–701. https://doi.org/10.1167/iovs.02-0822.
Yuan JP, Peng J, Yin K, Wang JH. Potential health-promoting effects of astaxanthin: a high-value carotenoid mostly from microalgae. Mol Nutr Food Res. 2011;55(1):150–65. https://doi.org/10.1002/mnfr.201000414.
Lee JJ, Kong M, Ayers GD, Lotan R. Interaction index and different methods for determining drug interaction in combination therapy. J Biopharm Stat. 2007;17(3):461–80. https://doi.org/10.1080/10543400701199593.
Rao AR, Sindhuja HN, Dharmesh SM, Sankar KU, Sarada R, Ravishankar GA. Effective inhibition of skin cancer, tyrosinase, and antioxidative properties by astaxanthin and astaxanthin esters from the green alga Haematococcus pluvialis. J Agric Food Chem. 2013;61(16):3842–51. https://doi.org/10.1021/jf304609j.
Saw CL, Yang AY, Guo Y, Kong AN. Astaxanthin and omega-3 fatty acids individually and in combination protect against oxidative stress via the Nrf2-ARE pathway. Food Chem Toxicol. 2013;62:869–75. https://doi.org/10.1016/j.fct.2013.10.023.
Yang Y, Fuentes F, Shu L, Wang C, Pung D, Li W, et al. Epigenetic CpG methylation of the promoter and reactivation of the expression of GSTP1 by astaxanthin in human prostate LNCaP cells. AAPS J. 2016;
Li R, Wu H, Zhuo WW, Mao QF, Lan H, Zhang Y, et al. Astaxanthin normalizes epigenetic modifications of bovine somatic cell cloned embryos and decreases the generation of lipid peroxidation. Reprod Domest Anim. 2015;50(5):793–9. https://doi.org/10.1111/rda.12589.
Yang Y, Bae M, Park YK, Lee Y, Pham TX, Rudraiah S, et al. Histone deacetylase 9 plays a role in the antifibrogenic effect of astaxanthin in hepatic stellate cells. J Nutr Biochem. 2016;40:172–7.
Takahashi K, Heine UI, Junker JL, Colburn NH, Rice JM. Role of cytoskeleton changes and expression of the H-ras oncogene during promotion of neoplastic transformation in mouse epidermal JB6 cells. Cancer Res. 1986;46(11):5923–32.
Suzukawa K, Weber TJ, Colburn NH. AP-1, NF-kappa-B, and ERK activation thresholds for promotion of neoplastic transformation in the mouse epidermal JB6 model. Environ Health Perspect. 2002;110(9):865–70. https://doi.org/10.1289/ehp.02110865.
Yu R, Mandlekar S, Lei W, Fahl WE, Tan TH, Kong AN. p38 mitogen-activated protein kinase negatively regulates the induction of phase II drug-metabolizing enzymes that detoxify carcinogens. J Biol Chem. 2000;275(4):2322–7. https://doi.org/10.1074/jbc.275.4.2322.
Su ZY, Khor TO, Shu L, Lee JH, Saw CL, Wu TY, et al. Epigenetic reactivation of Nrf2 in murine prostate cancer TRAMP C1 cells by natural phytochemicals Z-ligustilide and Radix angelica sinensis via promoter CpG demethylation. Chem Res Toxicol. 2013;26(3):477–85. https://doi.org/10.1021/tx300524p.
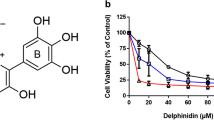
Kang NJ, Lee KW, Kwon JY, Hwang MK, Rogozin EA, Heo YS, et al. Delphinidin attenuates neoplastic transformation in JB6 Cl41 mouse epidermal cells by blocking Raf/mitogen-activated protein kinase kinase/extracellular signal-regulated kinase signaling. Cancer Prev Res (Phila). 2008;1(7):522–31. https://doi.org/10.1158/1940-6207.CAPR-08-0071.
Yu S, Khor TO, Cheung KL, Li W, Wu TY, Huang Y, et al. Nrf2 expression is regulated by epigenetic mechanisms in prostate cancer of TRAMP mice. PLoS One. 2010;5(1):e8579. https://doi.org/10.1371/journal.pone.0008579.
Khor TO, Fuentes F, Shu L, Paredes-Gonzalez X, Yang AY, Liu Y, et al. Epigenetic DNA methylation of antioxidative stress regulator NRF2 in human prostate cancer. Cancer Prev Res (Phila). 2014;7(12):1186–97. https://doi.org/10.1158/1940-6207.CAPR-14-0127.
Yla-Herttuala S. Oxidized LDL and atherogenesis. Ann N Y Acad Sci. 1999;874(1 HEART IN STRE):134–7. https://doi.org/10.1111/j.1749-6632.1999.tb09231.x.
Muthuirulappan S, Francis SP. Anti-cancer mechanism and possibility of nano-suspension formulations for a marine algae product fucoxanthin. Asian Pac J Cancer Prev: APJCP. 2013;14(4):2213–6. https://doi.org/10.7314/APJCP.2013.14.4.2213.
ACKNOWLEDGEMENTS
We thank all members of Dr. Ah-Ng Kong’s lab for helpful discussions and preparation of this manuscript. This study was supported in part by R01 CA200129, R01-CA118947, and R01-CA152826 from the National Cancer Institute (NCI), R01 AT009152 from the National Center for Complementary and Integrative Health (NCCIH), and institutional funds awarded to Dr. Ah-Ng Kong.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there are no conflicts of interest.
Additional information
Guest Editors: Ah-Ng Tony Kong and Chi Chen
Rights and permissions
About this article
Cite this article
Yang, Y., Yang, I., Cao, M. et al. Fucoxanthin Elicits Epigenetic Modifications, Nrf2 Activation and Blocking Transformation in Mouse Skin JB6 P+ Cells. AAPS J 20, 32 (2018). https://doi.org/10.1208/s12248-018-0197-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-018-0197-6