Residential mobility during upbringing has been associated with multiple adverse mental health outcomes in both children and adults.Reference Mok, Webb, Appleby and Pedersen1 These associations are thought to be mediated, at least in part, by stress resulting from the relocation experience and challenges associated with loss of social capital, severing social ties and integrating oneself into a new social environment. For example, Singh et al reported that positive associations between school mobility before age 9 years and psychosis-like symptoms at age 12 years were partially mediated by bullying involvement.Reference Singh, Winsper, Wolke and Bryson2 Adolescence may be a period of increased vulnerability to the stressors associated with moving, as a number of studies have reported stronger associations with mobility during adolescence compared with other developmental periods.Reference Mok, Webb, Appleby and Pedersen1,Reference Price, Dalman, Zammit and Kirkbride3,Reference Pedersen and Mortensen4 Furthermore, a prior Danish registry-based study of mobility across childhood indicated that early childhood mobility is not independently associated with subsequent mental disorder, but is explained by mobility during middle childhood and adolescence.Reference Paksarian, Eaton, Mortensen and Pedersen5 Such findings are in keeping with the increasing importance of peer relationships during adolescence,Reference Crosnoe6 as well as with the notion of adolescence as a sensitive period the development of executive function.Reference Blakemore and Choudhury7
Some studies have questioned whether associations between residential mobility and mental disorder are causal or are owing to unmeasured individual or familial factors that predispose toward both mobility and disorder.Reference Bramson, Rickert, Class, Sariaslan, Almqvist and Larsson8–Reference Morris, Manley, Northstone and Sabel10 In a Swedish register-based study of mobility before age 12 years, associations were reduced and eliminated when estimated within differentially exposed cousins and siblings, respectively, implying that the associations were explained by unmeasured genetic or shared environmental factors.Reference Bramson, Rickert, Class, Sariaslan, Almqvist and Larsson8 However, siblings who are differentially exposed to childhood residential mobility may not represent the general population, or may differ based on age of exposure rather than occurrence. Nonetheless, genetic confounding could occur if families who have greater genetic load for mental disorder are also more mobile, perhaps because of genetic effects on residential preferences or behaviours and symptoms that in turn influence residential stability.Reference Whitfield, Zhu, Heath and Martin11 Although some studies of mobility have included information on parental mental health,Reference Mok, Webb, Appleby and Pedersen1,Reference Bramson, Rickert, Class, Sariaslan, Almqvist and Larsson8 there is a scarcity of studies of mobility during adolescence that include other indicators of genetic liability that could be used to assess the potential for genetic confounding. The polygenic risk score (PRS) provides a dimensional measure of genetic risk that may usefully supplement information on family history of mental disorder. Current PRSs are based on information from genome-wide association studies that identified 108 genome-wide significant loci for schizophrenia,Reference Ripke, Neale, Corvin, Walters and Farh12 30 loci for bipolar disorderReference Stahl, Breen, Forstner, McQuillin, Ripke and Trubetskoy13 and 44 loci for major depression.Reference Wray, Ripke, Mattheisen, Trzaskowski, Byrne and Abdellaoui14
Current study
The goal of this study was to assess whether the associations between residential mobility during early adolescence and subsequent schizophrenia, bipolar disorder and major depressive disorder (MDD) are confounded by genetic liability. We selected adolescence as the exposure period of interest because we regard it as the period for which associations with subsequent mental disorder are most likely to be causal. We used data from a nationwide, population-based, case–cohort study and included information on both parental history and PRS for each disorder as measures of genetic liability. The study aims were to estimate the association between residential mobility and PRS for each disorder, and estimate the association between residential mobility and each disorder, before and after adjustment for genetic liability.
Method
Study population
We used information from four Danish registries, linked via a personal identifier assigned to all Danish residents. The Danish Civil Registration System (CRS) contains information on all residents, including dates of birth and death, place of residence and identity of parents and siblings.Reference Pedersen15 The Psychiatric Central Registry contains in-patient hospital admissions since 1969, and out-patient and emergency room visits since 1995.Reference Mors, Perto and Mortensen16 Registry diagnoses are those made by the treating clinicians and are recorded as ICD-8 and ICD-10 codes. The Neonatal Screening Biobank was established in 1981 and contains dried blood spot samples from nearly all Danish newborns.Reference Norgaard-Pedersen and Hougaard17 The Integrated Database for Longitudinal Labour Market Research was established in 1980 and contains data on education, employment and income. Data are supplied annually by tax authorities, educational institutions and employment services.Reference Petersson, Baadsgaard and Thygesen18
Data were drawn from the Lundbeck Foundation Initiative for Integrative Psychiatric Research (iPSYCH) sample, a large, psychiatric case–cohort study that contains incident psychiatric cases identified through 2012, as well as a random population sample (the subcohort), and has been described in detail previously.Reference Pedersen, Bybjerg-Grauholm, Pedersen, Grove, Agerbo and Baekvad-Hansen19 For the current study we selected cases of schizophrenia (ICD-10 code F20), bipolar disorder (ICD-10 codes F30–F31) and MDD (ICD-10 codes F32–F33)20 from the iPSYCH sample, along with the entire subcohort. We restricted the sample to those born on or before 31 December 1997, who were alive and living in Denmark on their 15th birthday and whose parents were identified in the registry. We then restricted to persons who had been genotyped and excluded cases diagnosed before age 15 years. The final analytic sample contained 4207 schizophrenia cases, 1402 bipolar disorder cases, 18 215 MDD cases and 17 582 subcohort members.
This study was approved by the Danish Data Protection Agency and the Scientific Ethics Committee in Denmark (1-10-72-287-12). According to Danish legislation, informed consent from participants is not required for registry-based studies.
Measures
Residential mobility during adolescence
Place of residence has been continually recorded in the CRS since 1971; residents are required to notify the government of address changes within 5 days.Reference Pedersen, Gotzsche, Moller and Mortensen21 This information was used to count the number of moves, defined as changes of municipality, between the 10th and 15th birthdays, with municipalities defined after the 2007 municipality reform. The number of moves in adolescence was categorised as 0, 1, 2 and ≥3.
Genetic liability
DNA from blood spots from the Neonatal Screening Biobank was whole-genome amplified in triplicate, using the Qiagen REPLI-g mini kit (Qiagen, Hilden, Germany). Reactions were pooled and genotyped with either the Illumina Human 610-Quad BeadChip array, Illumina HumanCoreExome beadchip or Illumina Infinium PsychArray-24-v.1.1 BeadChip (Illumina, San Diego, CA). PRSs for schizophrenia were calculated with a meta-analysis of Psychiatric Genomics Consortium samples, excluding two Danish samples, for a discovery sample of 34 600 cases and 45 968 controls. Single nucleotide polymorphisms (SNPs) were clumped into independent regions, excluding uncommon SNPs (minor allele frequency <0.02) and low-quality variants (information score <0.9). Only the most significant marker in the extended major histocompatibility region was retained. PRSs for MDD were calculated based on the most recently published results from the PGC,Reference Wray, Ripke, Mattheisen, Trzaskowski, Byrne and Abdellaoui14 and those for bipolar disorder were calculated based on summary statistics provided in advance of the latest genome-wide association study from the Bipolar Disorder Working Group of the PGC,Reference Ruderfer, Ripke, McQuillin, Boocock, Stahl and Pavlides22 both excluding Danish samples. SNPs were clumped based on a filtered list that included SNPs intersecting across all target data-sets and across all waves within target data-sets. SNPs were then filtered using an information score threshold of 0.6 and a minor allele frequency threshold of 0.01. For all PRSs, a P-value cut-off of 0.05 was used, in accordance with prior studies to achieve a balance between the number of false-positive and true-positive alleles.Reference Ripke, Neale, Corvin, Walters and Farh12,Reference Wray, Ripke, Mattheisen, Trzaskowski, Byrne and Abdellaoui14 PRSs were standardised using the mean and s.d. among the subcohort.
Parental history of mental disorder at the time of each individual's birth was extracted from the Psychiatric Central Registry and categorised hierarchically as broad schizophrenia (ICD-10 codes F20–F29 or equivalent ICD-8 diagnosis present for one or both parents), affective disorder (ICD-10 codes F30–F39 or ICD-8 equivalent present for one or both parents), other mental disorder (any other ICD-10 F diagnosis or ICD-8 equivalent present for one or both parents) and none.
Demographic covariates
Information on each individual's date of birth, gender, urbanicity at birth, paternal age and parental place of birth was taken from the CRS. Birth year was categorised as 1981–1985, 1986–1989, 1990–1993 and 1994–1997. Parental place of birth was categorised to reflect the number of parents born in Denmark: both, one or neither. Paternal age in years at the time of each individual's birth was categorised as <20, 21–25, 26–30, 31–35, 36–40 and ≥41. Urbanicity at birth was classified into five categories as per previous studiesReference Pedersen and Mortensen4: capital, capital suburb, provincial city (municipalities having a town with >100 000 residents), provincial town (municipalities having a town with 10 000–100 000 residents) and rural (municipalities where the largest town has <10 000 residents). Information on maternal education and paternal employment just before each individual's birth was taken from the Integrated Database for Longitudinal Labour Market Research. Maternal education was dichotomised to indicate primary education as the highest completed level, and paternal employment was dichotomised to indicate workforce participation. Family structure at age 10 years was included to capture parental separation/divorce and was measured by using data from the CRS to indicate whether or not each individual lived with both parents at age 10 years.
Analysis
Individuals were followed from their 15th birthday until diagnosis, emigration from Denmark, death or 31 December 2012. First, we evaluated the association between genetic liability and mobility in the subcohort, which is a random sample of the population that gave rise to the cases. We estimated the mean PRS for each level of mobility, adjusted for ancestry using the first ten principal components from a principal components analysis conducted using smartPCA of the EIGENSOFT 6.1.4 package for Linux (available at https://www.hsph.harvard.edu/alkes-price/software/)Reference Patterson, Price and Reich23. We then estimated the associations between genetic liability (PRS and parental history) and residential mobility among the subcohort, using separate binary logistic regression models (comparing each level of mobility with no moves). Second, we estimated associations between residential mobility and mental disorder, before and after adjustment for genetic liability, using the full case–cohort design. For each disorder, any subcohort members with diagnoses before age 15 years were excluded. Inverse probability weighting was used to account for the oversampling of cases.Reference Borgan, Langholz, Samuelsen, Goldstein and Pogoda24 The weight for cases were set to 1 since all cases were sampled, and the weight for non-cases were calculated as one over the sampling fraction of non-cases. We estimated crude and adjusted hazard ratios with 95% confidence intervals, using weighted Cox regression analysis with robust s.e. Finally, because the estimated PRSs may be less valid among those of non-European ancestry, we performed a sensitivity analysis restricting the sample to those whose parents were both born in Denmark. We also performed a sensitivity analysis, using a continuous measure of residential mobility.
Results
Supplementary Table 1 (available at https://doi.org/10.1192/bjp.2020.8) shows the sample characteristics of the cases and random population subcohort. In the subcohort, 90.8% did not move between ages 10 and 14 years, 6.7% (n = 1181) moved once, 1.8% (n = 322) moved twice and 0.7% (n = 114) moved three or more times. Unadjusted hazard ratios of schizophrenia, bipolar disorder and major depression, according to sample characteristics, are displayed in Table 1. Rates of all three disorders were higher among those with more residential moves during adolescence compared with those with no moves. Rates of all three disorders were also higher among those with higher PRS, as well as among those with parental history of mental disorder (Table 1).
Table 1 Unadjusted hazard ratios of schizophrenia, bipolar disorder and major depression, by sample characteristics

Paternal age, urbanicity, maternal education and paternal employment were measured at birth. There were 4207 schizophrenia cases, 1402 bipolar disorder cases, 18 215 major depressive disorder cases and 17 582 in the random population subcohort (17 579 for analysis of schizophrenia and 17 481 for analysis of major depressive disorder).
Mean PRS, adjusted for ancestry, by each level of mobility during adolescence are shown in Fig. 1. Overall, there was little visual evidence of an association between PRS and residential mobility. Table 2 shows associations between genetic liability (PRS and parental history of mental disorder) and residential mobility, estimated using logistic regression. PRSs for schizophrenia and MDD were weakly associated with moving once during adolescence (odds ratio 1.07, 95% CI 1.00–1.16; and odds ratio 1.10, 95% CI 1.04–1.17, respectively), but not with moving two times or three or more times (Table 2). PRS for bipolar disorder was not associated with adolescent mobility. Compared with PRS, parental history of mental disorder was more strongly and consistently associated with mobility (one move: odds ratio 2.10, 95% CI 1.65–2.65; two moves: odds ratio 2.47, 95% CI 1.65–3.70; three or more moves: odds ratio 2.60, 95% CI 1.35–5.00).

Fig. 1 Mean polygenic risk score (PRS) for schizophrenia, bipolar disorder and major depressive disorder (MDD) according to the number of changes of municipality from ages 10–14 years among individuals in the random population subcohort (n = 17 582; 17 517 for MDD). Polygenic scores are adjusted for ancestry using the first ten principal components.
Table 2 Associations between genetic liability for schizophrenia, bipolar disorder and major depression, and residential mobility from ages 10–14 years, among individuals in the random population subcohort
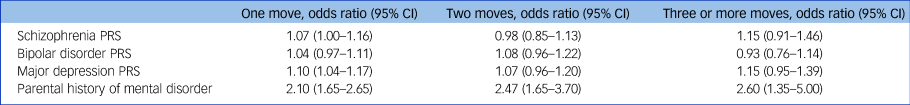
Polygenic risk score (PRS) estimates are adjusted for ancestry using the first ten principal components. PRSs are standardized as z-scores. Odds ratios are compared to moving 0 times between ages 10–14 years. Subcohort sizes were n = 17 582 for schizophrenia and bipolar disorder and n = 17 517 for major depression.
The associations of adolescent mobility with each mental disorder during follow-up, before and after adjustment for genetic liability, are displayed in Table 3. Adjusted for age, gender and birth year, mobility was positively associated with each mental disorder, with more moves associated with higher risk (model 1). The magnitude of associations was similar between the three outcomes, and hazard ratios ranged from 1.59 (95% CI 1.32–1.92) for the association between one move and bipolar disorder, to 4.43 (95% CI 3.30–5.96) for the association between three or more moves and schizophrenia.
Table 3 Associations of residential mobility from ages 10–14 years with schizophrenia, bipolar disorder and major depressive disorder, under various adjustments
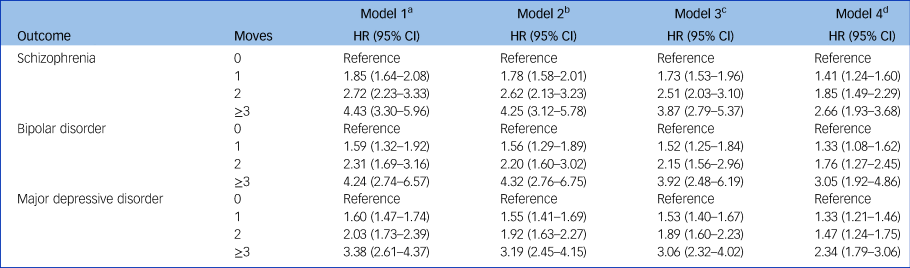
There were 4207 schizophrenia cases, 1402 bipolar disorder cases, 18 215 major depressive disorder cases and 17 582 in the random population subcohort (17 579 for analysis of schizophrenia and 17 481 for analysis of major depressive disorder).
a. Adjusted for age, gender and birth year.
b. Model 1, plus adjustment for the polygenic risk score and ancestry.
c. Model 2, plus adjustment for family history of any mental disorder.
d. Model 3, plus adjustment for urbanicity, paternal age, maternal education, paternal employment, parental place of birth and family structure at age 10 years.
The addition of adjustment for genetic liability is shown in models 2 and 3 of Table 3. Adjustment for the relevant PRS and ancestry (model 2) slightly reduced most point estimates, although some changes were negligible. Additional adjustment for parental history of mental disorder reduced estimates slightly further. Comparing model 1 with model 3 provides an assessment of the extent of genetic confounding as represented by the PRS and parental history. The percentage change in the natural logarithm of the hazard ratio between models 1 and 3 varied between 5.4 and 10.9%. Finally, additional control for urbanicity, paternal age, maternal education, paternal employment, parental place of birth and family structure at age 10 years (model 4) reduced estimates further. The magnitude of change resulting from the addition of these measures ranged from 27.7 to 37.3% for schizophrenia, 18.4–31.9% for bipolar disorder and 24.0–39.5% for major depression. Mobility was significantly associated with all three outcomes in these fully adjusted models, and the pattern of increasing risk with increasing number of moves was still apparent (Table 3).
The results of sensitivity analyses restricting to those whose parents were both born in Denmark are displayed in supplementary Tables 2 and 3 and the supplementary Fig. Associations between each PRS and residential mobility were not appreciably affected by this restriction, whereas associations between parental history of mental disorder and mobility were slightly stronger (Supplementary Table 2). The reduction in magnitude of odds ratios resulting from control for genetic liability was similar for one or two moves during adolescence. For three or more moves, model 1 point estimates were slightly higher and reductions after control for genetic liability were slightly greater in sensitivity analyses (Supplementary Table 3). The pattern of associations in fully adjusted models was similar. Supplementary Tables 4 and 5 show analyses using a continuous measure of residential mobility. These generally corroborated the results of the main analysis.
Discussion
In this study we used information on polygenic risk for schizophrenia, bipolar disorder and MDD, together with information on parental psychiatric history, to assess whether associations of residential mobility during early adolescence with subsequent diagnosis of each disorder are genetically confounded. We found little evidence that PRSs are associated with adolescent mobility. The strongest point estimates, which were modest in magnitude, were observed for the association of PRSs for schizophrenia and MDD with moving three or more times. On the other hand, parental history of mental disorder was strongly and consistently associated with mobility. Controlling for both indicators of genetic liability reduced associations slightly, indicating that partial genetic confounding may be present. However, mobility was still associated with all three outcomes after adjustment for genetic liability and demographic covariates, with point estimates indicating a dose-response relationship between the number of moves during early adolescence and risk for each disorder. Therefore, associations between adolescent residential mobility and the mental disorders assessed hereReference Mok, Webb, Appleby and Pedersen1,Reference Price, Dalman, Zammit and Kirkbride3–Reference Paksarian, Eaton, Mortensen and Pedersen5 do not appear to be attributable to genetic liability as we measured it.
Bramson et al investigated mobility up to age 12 years and found that associations with serious mental illness, substance misuse, suicide attempt, criminal convictions and low grade-point average were confounded by unmeasured familial factors, which could be genetic and/or environmental.Reference Bramson, Rickert, Class, Sariaslan, Almqvist and Larsson8 Although the age period they considered overlaps slightly with the one considered here, the two exposure periods may differ qualitatively because mobility in early childhood is more normative than mobility during early adolescence.Reference Paksarian, Eaton, Mortensen and Pedersen5,Reference Benetsky, Burd and Rapino25 Nonetheless, our results imply that the degree of genetic confounding of mobility associations captured by the PRS and family history may be relatively weak. One possibility is that our adjusted associations are affected by residual confounding owing to limitations of the PRS. However, it is also possible that the putative unmeasured familial factors that confound mobility associations are predominantly environmental in nature. Indeed, mobility is more common among children exposed to other stressors and adversities that could be shared among families, such as family conflict, parental dysfunction and abuse or neglect.Reference Bramson, Rickert, Class, Sariaslan, Almqvist and Larsson8,Reference Dong, Anda, Felitti, Williamson, Dube and Brown9 On the other hand, results from the Moving to Opportunity experiment, in which participants were randomised to receive housing vouchers providing the option to move, indicated detrimental effects of mobility on mental health among boys.Reference Osypuk, Tchetgen, Acevedo-Garcia, Earls, Lincoln and Schmidt26 Further, in a recent study Price et al found that schizophrenia risk was greater among those who moved longer distances from ages 7–15 years,Reference Price, Dalman, Zammit and Kirkbride3 a pattern less easily explained by confounding. Given such findings and the caveats inherent in interpreting results from sibling designs,Reference Keyes, Smith and Susser27 further research into the nature and degree of confounding of mobility associations may be warranted.
A small number of other studies have taken on the issue of selection-induced confounding in childhood residential mobility. Gasper et al used random effects modelling to estimate longitudinal associations between mobility and delinquency and substance use among adolescents, and found no within-person associations between mobility and those outcomes in the same year.Reference Gasper, DeLuca and Estacion28 Similarly, Morris et al found no within-person association between residential mobility and cannabis use in the same survey wave among participants in the Avon Longitudinal Study of Parents and Children.Reference Morris, Manley, Northstone and Sabel10 Using propensity score methods, Porter and Vogel found no associations between past-year mobility and past-year delinquency among adolescents with similar propensities to move.Reference Porter and Vogel29 However, in a subsequent study, Vogel et al used fixed-effects regression to estimate within-person associations and reported that although a binary indicator of mobility was not associated with delinquency, greater frequency of mobility was positively associated with delinquency.Reference Vogel, Porter and McCuddy30 Although these studies argue against a causal effect of mobility on behavioural outcomes, they have generally focused on outcomes occurring immediately following, or contemporaneous with, adolescent mobility. Additional research is needed to assess the causality of longer-term prospective associations between residential mobility and mental health.
In this study we focused on moves occurring between ages 10 and 14 years because prior studies have indicated that mobility during adolescence may be associated with greater relative risk of mental disorder compared with moves earlier in childhood.Reference Mok, Webb, Appleby and Pedersen1,Reference Price, Dalman, Zammit and Kirkbride3,Reference Paksarian, Eaton, Mortensen and Pedersen5 Adolescent mobility may differ qualitatively from earlier childhood mobility for a few reasons. Childhood mobility is more normative than adolescent mobility; in the USA, mobility is most common among young children and young adults, and decreases during later childhood and mid-to-late adulthood.Reference Benetsky, Burd and Rapino25 Mobile adolescents may therefore be newcomers in relatively entrenched social contexts, accentuating their outsider status and increasing social stress. Adolescent social contexts may also differ from those of younger children because of social developmental changes and the increasing importance of peer relationships.Reference Crosnoe6 In addition, families with young children may move for different reasons than families of adolescents.Reference Anderson, Leventhal and Dupéré31 Therefore, the degree of confounding of mobility associations, and the particular confounders involved, may differ by age. For example, if families with adolescent children are more likely to move in response to stressful life events than are families with young children, this could result in an apparent sensitive period during adolescence that is attributable to changes in the influence of confounding.
Causal explanations for associations between mobility and mental disorder generally focus on social processes and stress. Longer-distance moves, or those that require a change of school, may be accompanied by loss of social capital and severing of social ties that place adolescents at greater risk of developing mental disorder.Reference Coleman32 Adolescents who move may be more likely to join relatively less high-achieving and more deviant peer groups in their new locations, as these groups may be more receptive to newcomers.Reference Haynie, South and Bose33 This in turn may increase exposure to other risk factors such as substance use and other risky behaviours. Mobile adolescents may also be at greater risk of stressors, such as bullying, that increase risk for negative mental health outcomes.Reference Singh, Winsper, Wolke and Bryson2 These various potential social, psychological and behavioural mediators may invoke a variety of brain pathways to mental disorder. The social instability, stress and consequent exposures resulting from mobility may affect the development of executive functions such as social cognition,Reference Blakemore and Choudhury7 and affect hypothalamic–pituitary–adrenal axis and dopamine function.Reference Trainor34,Reference Lupien, McEwen, Gunnar and Heim35 Social defeat, which is used as a stress-induction paradigm and model of depression in animals, has been evoked in the schizophrenia literature to explain the increased risk among migrants and ethnic minorities.Reference Selten, van der Ven, Rutten and Cantor-Graae36 Animal models of social instability during adolescence, produced by switching cage partners, have resulted in heightened and prolonged hypothalamic–pituitary–adrenal axis response to new stressors and altered behavioural responses to drugs.Reference McCormick37 The existence of such general, stress-related or diffuse mechanisms would be consistent with the non-specific associations observed between mobility and mental disorder.Reference Mok, Webb, Appleby and Pedersen1 Future research into the role(s) of potential social and behavioural mediators in associations between mobility and mental disorder (e.g. Singh et al Reference Singh, Winsper, Wolke and Bryson2) could help to assess whether particular mediators are more or less relevant for particular outcomes. Future studies should consider outcomes across the full domain of mental disorder when possible, as assessment of the specificity versus generality of associations may shed light on potential mechanisms. Furthermore, although few experimental studies of mobility in humans exist, there may be opportunity for translational neuroscience approaches to identify stress-related brain pathways implicated in these associations (e.g. McCormickReference McCormick37).
Strengths of this study include the population-based iPSYCH sample, which includes a large number of prospectively ascertained cases of multiple mental disorders as well as a random population subcohort with available genetic information. Residential mobility was measured prospectively and independently of the outcomes, eliminating the possibility of recall bias. Although a growing number of studies have used PRSs in relation to environmental risk factors to demonstrate gene×environment correlation (e.g. Colodro-Conde et al Reference Colodro-Conde, Couvy-Duchesne, Whitfield, Streit, Gordon and Kemper38), fewer have included data on the outcome of interest to facilitate assessment of the presence and degree of confounding, as we do here. We also included information on both PRS and parental history of mental disorder to measure genetic liability, which was facilitated by the availability of psychiatric registry data covering the entire Danish population.
This study also has a number of limitations. PRSs only capture variance owing to common SNPs and may have low individual predictive abilityReference Ripke, Neale, Corvin, Walters and Farh12–Reference Wray, Ripke, Mattheisen, Trzaskowski, Byrne and Abdellaoui14; it is possible that access to a more complete or more powerful measure of genetic liability would have altered our results. We lacked individual- and family-level information on correlates of mobility that would have allowed for more thorough investigation of genetic and environmental sources of confounding. Although evidence for validity is good, registry diagnoses rely on clinician diagnosis and may not include less severe cases.Reference Kessing39,Reference Uggerby, Ostergaard, Roge, Correll and Nielsen40 Parental history of mental disorder was included as an indicator of genetic liability, although it includes both genetic and non-genetic exposures. Finally, because genetic data were available in the biobank starting in 1981, the sample was relatively young and had not completely passed through the period of risk for onset of mental disorder at the end of follow-up. A larger, older sample with more cases of disorder may afford more statistical power, which could affect the statistical significance of the modest associations we detected between genetic liability and residential mobility, especially for two and three or more moves (Table 2 and the Fig. 1).
In conclusion, we assessed the possibility of genetic confounding of the associations between residential mobility during early adolescence and subsequent schizophrenia, bipolar disorder and major depression. Using PRSs and information on parental history of mental disorder as indices of genetic liability, we found little evidence that genetic liability explained mobility associations. Although a degree of residual confounding may be present, results imply that the potential familial confounding of mobility associations may be largely environmental in nature.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2020.8.
Funding
This work was supported by the Intramural Research Program of the National Institute of Mental Health (ZIAMH002953 to K.R.M.), the Danish Strategic Research Council, the Faculty of Health Sciences at Aarhus University, the Lundbeck Foundation Initiative for Integrative Psychiatric Research (unrestricted grant R155-2014-1724) and the Stanley Medical Research Institute. The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of any of the sponsoring organisations, agencies or the US Government. Genotyping was supported by funding from a philanthropic gift to the Stanley Center for Psychiatric Research at the Broad Institute. This research has been conducted using the Danish National Biobank resource, supported by the Novo Nordisk Foundation. The funders of the study had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Acknowledgements
We gratefully acknowledge the Psychiatric Genomics Consortium Schizophrenia and Bipolar Disorders working groups and the research participants and employees of 23andMe, Inc. for making summary statistics available, as well as the Broad Institute for genotyping assistance.
Data availability
E.A., C.B.P., P.B.M., H.T.H. and B.B.T. have full ongoing access to the study data.
Author contributions
D.P., C.B.P. and E.A. formulated the research questions. E.A. and H.T.H. designed the study, and O.M., A.D.B., D.M.H., M.N., T.W., C.B.P., P.B.M. and E.A. carried it out. B.B.T. and H.T.H. analysed the data. All authors interpreted the data. D.P. drafted the manuscript. All authors revised and approved the final version of the manuscript.










eLetters
No eLetters have been published for this article.