- Research
- Open access
- Published:
Ensuring universal access to quality care for persons with presumed tuberculosis reaching the private sector: lessons from Kerala
International Journal for Equity in Health volume 23, Article number: 101 (2024)
Abstract
Background
More than half of the people with Tuberculosis (TB) symptoms in India seek care from the private sector. People with TB getting treatment from private sector in India are considered to be at a higher risk for receiving suboptimal quality of care in terms of incorrect diagnosis and treatment, lack of treatment adherence support with a high loss to follow-up rate that could eventually increase their risk of drug resistance. The current study aims at documenting the approach and efforts taken by the Kerala state to partner with the private health care delivery providers for ensuring quality TB care to the people with presumed TB reaching them.
Methods
A case study approach was adopted with review of all available literature followed by five Key Informant Interviews to understand the case through a primary descriptive exploration. Grounded theory approach was used to generating the single theory of the case itself that explains it.
Results
Kerala state has taken a variety of interventions to ensure universal access to TB care for citizens reaching the private sector with documented improvement in the quality of TB care. Key learnings from these initiatives were (i) patients need to be at the centre of partnerships, (ii) good governance is essential for ensuring Universal Health Coverage in a mixed health system, (iii) data intelligence is required to guide partnerships, (iv) identification of the correct ‘problems’ is crucial for effective design of partnerships and (v) a platform for meaningful dialogue of key stakeholders is needed.
Conclusion
Kerala experience demonstrated that if governments take a proactive role in engaging the private sector, in an informed and evidence-based way, they can leverage the advantages of the private sector while protecting the public health interest.
Background
The Standards for TB Care in India (STCI), which is a locally customized version of the International Standards of Tuberculosis Care, mentions 26 standards of care that every citizen of India should receive irrespective of the sector of treatment [1]. STCI deliberate on standard tools and strategies for early and complete detection of TB, standards of treatment in terms of drugs and regimens for best patient outcome, standards of public health actions and patient support such as adherence monitoring, clinical follow up, contact investigations and TB Preventive Therapy to the family. STCI lays down what is expected for quality TB care from the Indian healthcare system.
More than half of the people with TB symptoms in India seek care from the private sector [2, 3]. Gaps in the TB care cascade such as people with TB not having access to correct and complete diagnosis, people diagnosed with TB not being started on correct treatment; and people started on treatment not completing treatment, were observed more among people with TB who were diagnosed in the private sector compared to the public sector [4,5,6,7]. There are also concerns about the suboptimal quality of care including incorrect diagnosis and non-standardized treatment regimens, lack of systems for treatment adherence support resulting in high loss to follow-up rate increasing the risk of drug resistance among the people who seek care from the private sector in India [4,5,6,7]. Many services assured in the public sector, such as free diagnostics including rapid molecular tests and drug susceptibility testing, free quality assured drugs, treatment adherence support and monitoring, contact investigation and TB preventive therapy, linkages to social welfare schemes rarely reach the patients who are treated in the private sector. Not having access to full range of quality TB care when and where the people need them, could be a hindrance to achieve Universal health coverage (UHC).
Realising the urgent need to engage private sector, the National Strategic Plan (NSP) for TB Elimination in India (2017–2025) enlisted various strategies to ensure that patients reaching the private sector receive care as per the STCI [8]. National TB Elimination Program (NTEP) has taken a variety of approaches including trainings, regulations, provisions of free services such as drugs and diagnostics, incentives and partnership schemes to engage with private sector [9]. Government of India has issued directives making TB notification mandatory as a first step to ensure STCI to all people affected with TB [10]. Provisions have been developed in Ni-kshay, the real time case-based web-based management information system of NTEP, where private providers can directly log in to the system using their user credentials and notify TB and report outcomes [11]. NTEP provides 500 INR (IUSD = 85 INR) as an incentive to the private provider to notify each TB patient and another 500 INR to report the treatment outcome [12]. Anti TB medicines have been included in schedule H1 which can only be sold on prescription of a Registered Medical Practitioner and details of the prescriber, the patient and the drug sold needs to be maintained by the chemists [13]. NTEP has also provisions for supplying free quality assured anti- TB drugs and free molecular tests and drug susceptibility tests to the patients reaching the private sector. Directly and through various agencies, NTEP intends to provide support for contact investigations and treatment adherence to all patients reaching private sector. NTEP guidance document on partnership (2019) details out about the purchase of various services from private sector [14]. Patient Provider Support Agencies (PPSA), predominantly Non-Governmental Agencies, are contracted in with the task of engaging with private sector for notifying cases to NTEP and coordinating with NTEP for free drugs and follow-up.
Despite all these initiatives in India, TB notifications and ensuring public health actions for people with TB have not been really converted into routine practice in private sector. NSP intended to achieve a target of two million TB notification from private sector in 2021; there is a gap of 1.3 million TB cases who are ‘missing’ in the surveillance system [2, 9]. Studies, annual reports and evaluations revealed that Kerala state has successful ensured quality TB care to the people reaching the private sector [9, 15, 16]. The current study aims at documenting the approach and efforts taken by the Kerala TB Elimination program to partner with the ‘for profit’ formal private health care delivery providers for ensuring quality TB care with special emphasis on potential lessons to be learnt from the state. This is expected to help policy makers and programme managers in other parts of India and in other countries who face challenges in partnering with private sector for ensuring universal access to quality TB care.
Methods
Local setting
Kerala has experienced a 7.5% annual decline in the TB incidence since 2015 and has been certified for the same by Government of India under its sub-national TB free certification process [17, 18]. The state TB program has been appreciated by the Joint Monitoring Mission (JMM) 2019, led by the World Health Organization and global developmental partners, for providing patient-centric TB care through systematic interventions [15]. Various efforts by the state for providing support to the people and family with TB were documented [19]. The private health care sector in Kerala accounts for more than 70% of all facilities and 60% of all inpatient beds. A significant proportion of people from low socio economic status also avail health care from private hospitals in the state for various reason such as long waiting time in public facilities, perceived low quality of care in public sector and proximity of health facilities [20]. National TB Prevalence survey (NTPS) revealed that among those with TB symptoms and sought health care in Kerala, 38% consulted the private sector first [2].
Design
A case study approach was used to understand the case through a primary descriptive exploration. Review of all available literature followed by five Key Informant Interviews (KIIs) were conducted.
Desk review
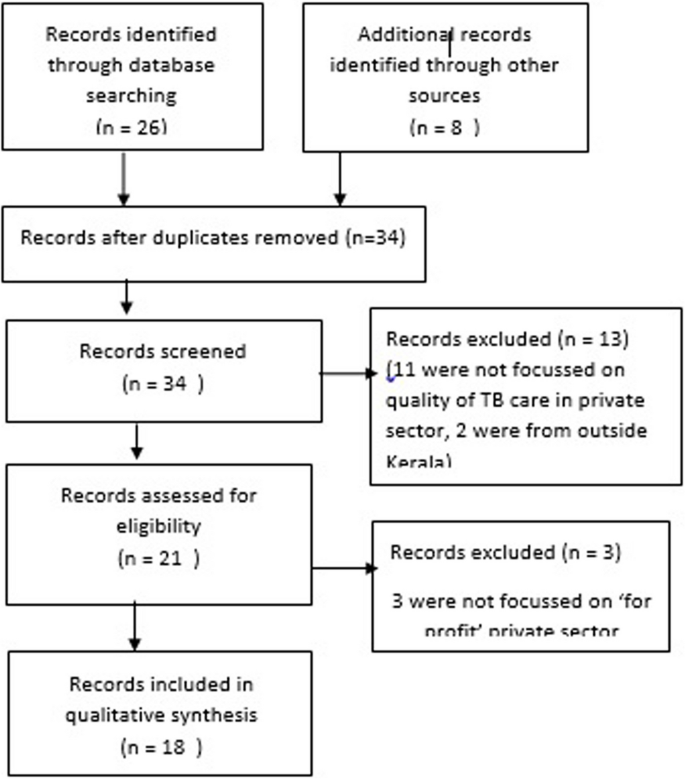
Desk review of all available documents and studies were attempted first. All documents such as policy documents, operational plans, guidelines, annual reports and evaluation studies available in public domain in official websites of health department were referred to look for (1) policy and plan for engagement of private sector for TB care and (2) outcomes and data related to TB patients reaching the private sector. A high level of objectivity and sensitivity was maintained during the process; the authenticity of the documents were assessed, and the goals and biases were explored before examining the content. Literature search was done in MEDLINE, Embase and Web of Science using the key words (TB OR Tuberculosis) AND (Private hospital OR Private facility OR Private Partnership OR Private Practise OR Private Sector OR Public Private Partnership) AND Kerala. The search was carried out on 21st December 2022, and all studies including descriptive and analytical studies were included irrespective of the publication type. Studies published since 2000–2022 were included as our interest was in the recent situation, and earlier publications were difficult to access. Reference lists of papers identified in the searches, were scanned. Information was obtained about studies from state TB cell from where permissions for using TB-related data are sanctioned.
We used the operational definition provided by World Health Organisation which defined private health sector as ‘the individuals and organizations that are neither owned nor directly controlled by governments and are involved in provision of health services’ [21]. Reading abstracts, studies related to private sector and TB done in Kerala were included. We focussed on ‘for-profit’ healthcare providers, because they are more numerous and difficult to engage. We included only health service providers rather than manufacturers or distributors of medical equipment, technologies, consumables or drugs. All identified articles were screened for full-text review. Articles not focussing on ‘for-profit’ health sector and ‘quality of TB care’ were excluded.
Key informant interviews
Based on the literature review, additional five KIIs were conducted to fill in gaps in the information, to explore additional documents to be reviewed and to validate the observations from the literature. Key informants were persons with long experience in the field of TB control, who had broad knowledge of the TB scenario in the state, were aware of the TB programme activities over the years and who were involved in policy formulation and implementation related to TB and private sector. They were selected as they were the persons with the longest experience, each having more than 15 years of experience, in the field and had a broad overview of the TB and private sector engagement in the state. They were (i) a senior bureaucrat, involved in policy making (ii) a state-level programme manager responsible for TB programme activity implementation, (iii) a technical consultant for TB elimination from a global partner agency, responsible for guiding the state in TB policy formulation, implementation and supervision (iv) a senior leader of Indian Medical Association who was associated with TB projects implemented through IMA and (v) director of a 600 bedded private hospital. Participants were approached by phone, the purpose of the interviews were communicated and the prerequisites during the interview (stable internet connection, calm environment and with video switched on) were communicated. Two interviews were conducted in English and the rest in Malayalam, by PS (male, medical doctor with post-graduation in public health with 10 years of research experience), who was experienced in conducting qualitative studies and was fluent in the local language. All KIIs were conducted online using Zoom (Zoom Video Communications, San Jose, CA, USA) with video. One researcher recorded the proceedings, identifying key themes and monitored the verbal and non-verbal interactions. All participants who were contacted could participate. Major themes discussed were initiatives taken by the Government to engage private sector, major outcomes of such strategies and reasons for changing strategies. Each interview lasted for approximately 45 min (range: 25–75). No repeat interviews were attempted. KIIs were later transcribed verbatim and translated into English. Transcripts were returned to participants for comments.
Grounded theory approach was used to develop theory. We did not attempt to generate strong theories rather focussed on generating the single theory of the case itself that explains it. This was a deliberate attempt in order not to draw away our attention from features for understanding the case.
The transcripts were then manually coded by PS, emerging themes were identified. Citations with similar coding were grouped according to the predetermined themes. Themes were derived from the data. Recurrent themes were marked as important. All the flagged statements were put together and synthesised. The team went through the transcripts and notes and reached a consensus. Data triangulation was done comparing information from literature and qualitative interviews. Inductive thematic saturation was reached and no new codes emerged after the fourth interview. The study was approved by the Institutional Ethics Committee of Amity University, Noida, India.
Results
PRISMA flow chart for the literature review were presented as Fig. 1.
The results of desk review and the KIIs are presented below.
Efforts for private sector engagement for TB care in Kerala
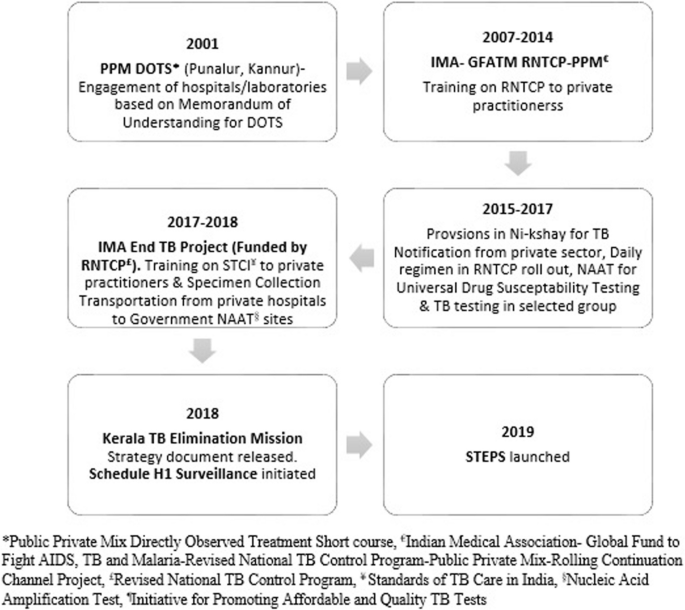
Many public-private mix strategies for TB care started in Kerala during the initial years of implementation of the National TB Elimination Program (NTEP), then called Revised National TB Control Program (RNTCP). Milestones of various initiatives by the state TB program to engage private sector for TB care ares described in Fig. 2. Details of major initiatives by NTEP directly or in partnership with various stakeholders are compiled in Table 1.
In 2016, even after the NTEP implemented a daily anti-TB regimen—the absence of which was cited as the major reason by the private sector for not participating—there was not much improvement in the private sector participation in terms of contributions towards TB notification or partnering with NTEP on signed partnership schemes. Operations researches conducted through the NTEP mechanisms, revealed many challenges for sub-optimal private sector participation [32, 33]. Efforts were also put in place to understand the real problems of patients reaching the private sector [34]. A study that followed up a cohort of TB patients treated in private facilities in Kerala reported a loss to follow-up of 20–30% [34]. Limited ability to monitor and promote treatment adherence remained a major challenge in the private sector. Although NTEP documents the treatment outcome of every patient diagnosed/enrolled for treatment, such documentation is rare in the private sector. Lack of a network of field staff in the private sector limits the ability to monitor and support adherence to standards of care. STEPS (System for TB Elimination in Private Sector) evolved as a solution for ensuring standards of TB care in a patient-centric way for all patients accessing the private sector, addressing the concerns of the public and private sector [29, 30]. A pilot STEPS centre in a private tertiary care centre in Kerala demonstrated that establishing STEPS centre within the hospital ensured 100% TB notification with a 4-fold increase in the number of patients notified over 6 months [35].Two interventions which emerged as prominent and replicable ones in our review are described below.
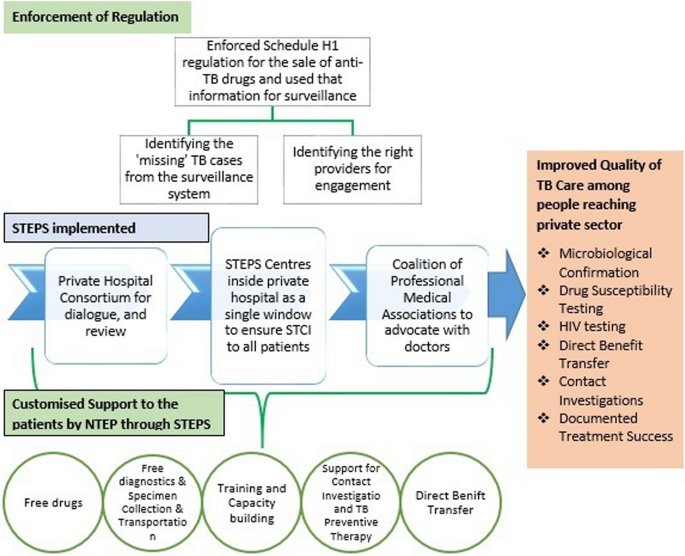
STEPS model
STEPS was envisioned as an equal partnership between the public and private sector for benefit of the society with improving standards of TB care as the outcome. Concept and evolution of STEPS are documented in detail elsewhere [30]. STEPS has three components: (i) a private hospitals TB consortium at district and state level consisting of hospital managements for policy support and review (ii) a coalition of medical professional associations at state and district levels for advocating with doctors and (iii) a STEPS centre in each private hospital. STEPS centre within a private hospital is a single window for diagnostic and treatment services, notification, patient linkage with social welfare, contact investigation, TB Preventive Therapy and treatment adherence support. A central person (STEPS lead) nominated by the hospital management, work together with contact persons (STEPS links) for each in-house department in a hub-and-spoke model. The STEPS lead and links are typically staff nurses. STEPS Links from various in-house clinical departments transfer the patients and related information to the STEPS Lead. Patients visit STEPS centre where education, counselling, support and linkages for molecular diagnostics, anti TB treatment initiation, contact investigations, TB Preventive Therapy, social welfare schemes and air borne infection control counselling are provided. STEPS Lead follows up the patient periodically over telephone and provides treatment adherence support, monitors adverse drug reactions, reminds clinical follow up and schedules reviews. Patient visits the concerned in house departments for clinical follow up. Through STEPS, private hospitals proactively supported patients to make decisions and participate in their own care. It also fosters customer loyalty. STEPS Lead enters information in NI-KSHAY. NTEP through its field staff and also through the five city officers of project JEET, a PPSA worked in the state for 2 years (2018–2019), provided customised and need based support to the patients reaching private hospitals, through the STEPS centres, including free diagnostics such as molecular tests and drug susceptibility testing, transportation of specimen from the hospitals for testing, free drugs, support for contact investigation, TB Preventive Therapy, Direct Benefit Transfer, linkages to social welfare services and retrieval if there is a lost to follow up. STEPS was implemented in all 14 districts of Kerala state, India since January 2019. Of the 446 hospitals mapped which manages more than 80% of the TB patients in the state, 318 established STEPS centres during 2019 and the remaining in 2020 [17, 30].
Outcomes of STEPS
JMM (2019 November, India) visited Kerala and recommended supporting the establishment of STEPS Centres in all private health care facilities [15]. A formal evaluation of STEPS was conducted by a multi-disciplinary team in 2021 by (i) visiting 30 randomly selected STEPS centres for assessing infrastructure and process using a checklist, (ii) validating the patient data with Ni-kshay by telephonic interview of 57 TB patients (iii) analysing the quality of patient care indicators (iv) conducting in-depth interviews with 33 beneficiaries and stakeholders to understand their satisfaction and perceived benefits and (v) a cost analysis from the perspective of NTEP, private hospital and patients [31] .
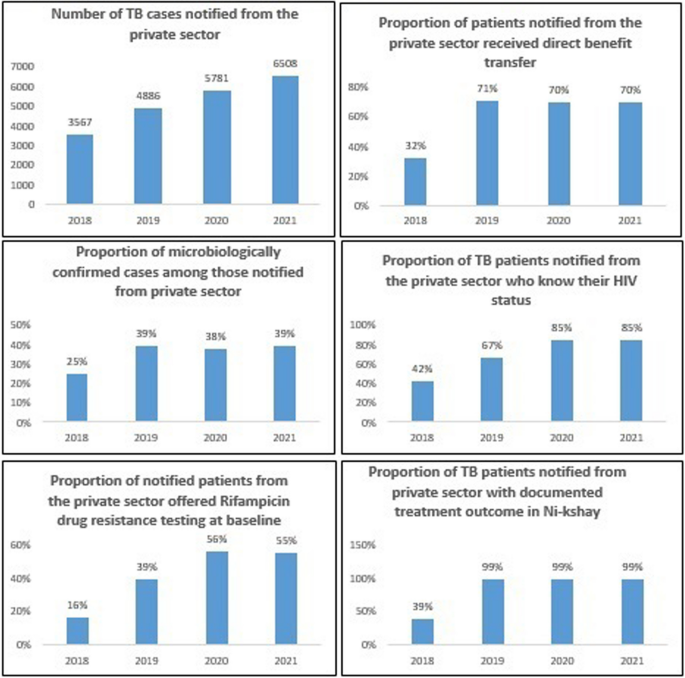
Evaluation concluded that STEPS is a low cost, ‘patient centric’ model where the patient can approach any provider according to his/her choice and get uniform high quality TB care. Evaluation also revealed that STEPS was acceptable to all stakeholders and patient satisfaction was good. There was significant improvement in the quality of TB care indicators for patients diagnosed in private hospitals over the years in terms of notification, proportion with a microbiological confirmation of diagnosis, known HIV status, beneficiary receiving baseline rifampicin testing, Direct Benefit Transfer and the documented treatment success rate (Fig. 3).
Number of specimens from private sector tested using molecular testing machines at public laboratories increased from 7606 in 2018 to 14,940 in 2021 [9]. STEPS led to a shift from using private anti-TB drugs to NTEP-supplied drugs and there was a drastic drop in the sale of anti-TB drugs in the state from 1.6 million rifampicin units in 2018 to 0.5 million rifampicin units in 2019 [16, 17, 31]. STEPS had also demonstrated good resilience in ensuring TB services during COVID-19 pandemic period [36].
Schedule H1 surveillance
Since 2016, the Government of Kerala has enforced Schedule H1 implementation for anti-TB drugs as a joint venture by the drugs control department and state TB Elimination program, with monitoring from the top administrative level. From 2018 onwards, the state program managers of NTEP have modified it into a Schedule H1 surveillance system [28]. The process of schedule H1 surveillance and its benefits were documented through in-depth interviews of the drugs control department enforcement officers, chemist shop owners, private sector doctors, leaders of professional medical associations, and program managers and key staff of the TB Elimination Program in Kerala [28]. The TB Elimination Program of Kerala used the information from the Schedule H1 drug register to identify the missing TB cases from the surveillance system, identify providers who prescribed the anti TB drugs and extended support to them for ensuring STCI to their patients, and provide feedback to providers regarding prescription practices. The estimated number of un-notified TB cases per 100,000 people based on the total sales of rifampicin-containing products in Kerala showed an annual decline of 22% over the last few years, closing the gap in the surveillance system [17]. The major initiatives taken by the state for ensuring quality care to the patients reaching the private sector is represented schematically in Fig. 4.
Learnings from Kerala for engaging private sector for TB care
-
1.
Vision of partnership: Most of the partnership models implemented in the country were mostly business-centred like incentive-based or service-purchase models that were similar to a client-vendor relationship rather than an equal partnership between the public and private sectors. Several models implemented in India that have successfully increased private case notifications were difficult to expand due to lesser emphasis on creating lasting partnerships and huge short-term financial implications [37, 38]. As the intermediary agency who interacts with the private sector withdraws, the model collapses. Kerala state has literally redefined the ‘private sector engagement’ as a partnership for shared health outcomes. The vision of partnership that the state implemented through STEPS is in line with the recent vision shared by World Health Organization which described partnership as a means to “bring together a set of actors for the common goal of improving the health of populations based on mutually agreed roles and principles based on the principles of relative equality between the partners, mutual benefits to the stakeholders, autonomy, accountability and mutual commitment to agreed objectives” [39]. The state has proved that partnership with private sector is possible in the form of a relationship and not mere as contracts or purchase.
-
2.
Strategic policy direction: Having a clear policy and strategy will help to avoid confusions among the stakeholders and will enable them to execute better. It should clearly define the goals and objectives of private sector engagement, clarify roles of all stakeholders, describe the institutional arrangements for engagement, outline the feasible strategies and arrangements to monitor performance. Health system decision makers need to know “where they are going” to be able to make efficient use of finite resources. The state has set a clear strategic policy direction with regard to engagement of private sector and trained all program managers regarding the same [29]
-
3.
Strong governance mechanism: In Kerala, the state government focused on the governance of the whole health system – both private and public – to ensure access to quality TB care. The government efforts were successful in aligning the private sector with a common goal and making them commit to work to support the agenda. Both the sectors collectively delivered on the realization to ensure access and quality of TB care. Institutional mechanisms for periodic interaction between the public health system and the private sector were established. There was a clear understanding and delineation of the roles based on each stakeholder’s skills and expertise and there was mechanism to ensure accountability of both sectors. There was also a strong regulatory environment with regard to implementation of schedule H1 for anti-TB drugs, at the same time the information through the process has been used for generating data intelligence and ‘nudging’ positive behaviors among the private sector. The governance mechanisms ensured that the actors have the powers to do their jobs and to ensure that others do theirs. The government proactively promoted initiatives like IPAQT where TB tests are made available at affordable prices in the private sector [40]. Through ‘Coalition of Professional Medical Associations’ the government tried to bring in a social regulation too promoting STCI to every citizen.
-
4.
Understanding the ‘problem’: Clear understanding of the ‘problem’ that is to be solved through partnership is critical in any successful partnership. The partnership needs to be tailor made to address the identified problems. Similarly understanding the behaviour of stakeholders and involving them from the planning phase are also important before developing any strategy. In Kerala, efforts were put in formally through operations research to identify the problem clearly and document the perceptions and concerns of different stakeholders [32, 33]. STEPS evolved as a solution to address those concerns. Major challenges for ‘partnerships’ identified through various operations research done in the state and how that have been addressed through the STEPS is summarised in Table 2. Kerala experience also reiterates that it is better to avoid over-reliance on pre-designed solutions when it comes to designing partnerships.
-
5.
Generate data intelligence: There need to be systematic efforts for collection, compilation and analysis of data to guide the priorities for action. In Kerala, overall data regarding the sales of anti-TB drugs helped in (1) estimating the load of patients being treated in private sector and (2) monitor the trends. Granular information from schedule H1 data helped to (1) identify the potential providers for engagement and (2) identify the cases missed from the official surveillance system [28]. Experiences from the state iterate that pharmacy based surveillance of anti-TB drug sales has immense potential to improve the overall quality of TB care.
-
6.
Enable stakeholders, foster relations and align structures: In Kerala, organizational structures were aligned towards the policy objectives that empowered the actors. ‘Private hospital consortium’ and ‘coalition of professional medical associations’ at state and district level enabled actors to work openly, sustainably, and effectively together, with trust. The consortium became the face of the private sector which facilitated dialogues between partners, catalyzed the implementation of policies and ensured that both the sectors are held accountable for their actions for the population. There were also district and sub-district wise WhatsApp groups with STEPS leads of all hospitals and the NTEP staff which facilitated smooth and easy communication. All such efforts to foster relations allowed stakeholders to move beyond simply understanding one another, to being able to work together.
-
7.
Openness to change: Important strategic change that contributed to rapid scale-up and acceptance of STEPS were the attempts to gain the trust of hospital management, involvement of nurses for documentation and counselling, efforts for quality control through a coalition of professional medical associations, lack of formal memoranda of understanding, and lack of major financial transactions between partners [30]. Such flexibility and openness to change is crucial while governing mixed health systems.
-
8.
Patient needs to be at the centre of every partnership: All public private partnership need to be ‘patient centric’ and their specific health needs and desired health outcomes should be the driving force. STEPS is a patient centric partnership where patient is the central figure in the continuum of care [30, 31]. STEPS tells us that partnerships need to be designed after understanding the needs, preferences and circumstances of patients.
-
9.
Equipping the public sector with the necessary skills and understanding to effectively engage with private sector: The state has undertaken a behavior change strategy for the NTEP staff to have a uniform outlook with regard to private sector engagement. Capacity of program managers and peripheral staff were built to deal with private sector in a more efficient way [31].
-
10.
Incorporating UHC principles into a business model is possible: STEPS is a model based upon a self-initiated business promotion focusing on the concepts of ‘quality of care’ and ‘customer loyalty’ blended with the social responsibility of the private sector. STEPS centers used ‘after-sales support’ by following up every client, which could also be viewed as a business strategy which typically leads to higher customer satisfaction, brand loyalty, and even word-of-mouth marketing. Cost estimates revealed that implementing STEPS will be of benefit to private hospitals in terms of business returns [31].
Discussion
The current study documents various approaches and efforts taken by the Kerala TB Elimination program to partner with the‘for profit’ formal private health care delivery providers for ensuring quality TB care. The current study attempts to synthesise the evidences generated from various studies conducted over different time periods and narrates a story which explains the changes in strategies, outcomes and the reasons for the same. Though the results are not meant to be generalized to other settings, it provides lot of insights to strengthen the private sector engagement in the country.
Though, Kerala state was proactive in engaging hospital and laboratories for DOTS (Directly Observed Treatment Short course) through formal memorandum of understanding through various partnership schemes and various efforts for capacity building, a significant chunk of private hospitals could not be engaged until 2018 resulting in sub-optimal quality of care to a significant proportion of people reaching the private sector in terms of not being offered treatment adherence support, baseline susceptibility testing for Rifampicin, contact investigations and linkages to social welfare schemes. After thorough understanding of the problem and the characteristics of the private sector and in consultation with the stakeholders, the state initiated STEPS which is an equal partnership model where both sectors have been made accountable to ensure uniform standards of TB care to the citizens reaching the private sector. Through enforcing schedule H1 regulations for the sales of anti-TB drugs, the state generated data and established an intelligence system for prioritising actions for partnerships and monitoring the outcomes. The implementation resulted in improvement in the quality of TB care among the people with TB reaching the private sector too.
Through the initiatives, Kerala has literality reframed ‘private sector engagement’ as ‘a partnership where both the sectors come together for the benefit of the society’. STEPS ensured that public resources are not diverted too much; and whatever is diverted through the STEPS is for the patient. In a country like India where most of the patients seek care from the private sector and the program managers are thriving to ensure quality of care in public sector with the limited resources, ‘purchasing’ of services and ‘incentivising’ of the private sector may not be the best way to create sustainable partnerships. Instead, the commitments to offer quality TB services need to be considered as the prime partnership option. Private sector will be more than willing to improve the quality of care to their clients as it improves patient satisfaction and provides good marketing advantage in the competitive healthcare. High out of pocket health expenditure will be the only concern then, which could be addressed to the needy through public provision of services through the private partner, promoting schemes such as IPAQT where TB tests are made available at affordable prices in the private sector or hospitals getting reimbursed for drugs and diagnostics through national health insurance schemes.
Kerala demonstrated that if Governments take a proactive role in engaging the private sector, in an informed and evidence-based way, they can leverage the advantages of the private sector while protecting the public health interest. The case study reiterate that a good governance is essential for ensuring care in a mixed health system. The pursuit of UHC requires Governments to take ownership of healthcare, irrespective of where a person seeks care. WHO Advisory Group on the Governance of the Private Sector for Universal Health Coverage also emphasise a fundamental shift in the Governance behaviours to do business in a new way [39].
Data intelligence is crucial to successful governance. Good governance require data to identify whom to engage, monitor the progress and measure the impact. The state has used data coming out from the drug sales for the surveillance purpose. The state demonstrated that pharmacy based surveillance of anti-TB drug sales has immense potential to help the TB programs in improving the quality of care in private sector.
Success of STEPS also emphasises that successful private sector engagement initiatives need to have a platform for meaningful dialogue. Strengthening platforms, or structures for dialogue, and communication between sectors is important in building trust, and co-development of policies. Medical College Task Force is an example of a structured mechanism where NTEP interacts with all medical colleges [41]. It has state, zonal and national level structures. Similarly, a ‘Private Health Sector Task Force/consortium’ created at district, state, zonal and national level need to be established at the country level.
Kerala state has taken proactive role to partner with private sector after ensuring the quality of care in the public system. The model need to be customised and contextually adapted following the principles and approach and shall not be replicated as such, especially in settings where health systems are weak. It has also to be emphasised that the current experiences with the STEPS model in Kerala are with private hospitals and not with individual practitioners. It is also recommended that Kerala needs to systematically capture the patient’s cost and document the same for more meaningful insights.
Conclusion
Kerala state has taken a variety of interventions through STEPS to ensure universal access to TB care for citizens reaching the private sector with documented improvement in the quality of TB care. Kerala demonstrated that if Governments take a proactive role in engaging the private sector, in an informed and evidence-based way, they can leverage the advantages of the private sector while protecting the public health interest. The case study reiterates that a good governance is essential for ensuring care in a mixed health system and such successful governance requires good data intelligence. Kerala reminds us that identifying the correct ‘problems’ are critical for effective design of partnerships and over reliance on pre designed solutions may not work.
Availability of data and materials
Data are available upon reasonable request. Data collected for the study, including individual de-identified participant data and a data dictionary defining each field in the set, study protocol, informed consent forms will be made available to others for a period of three years from the date of publication of the article, with a signed data access agreement and on due approval from the institutional ethics committee of Amity University, India, on submission of request to the principal investigator explaining the purpose for which the data will be used along with other relevant supporting documents.
References
World Health Organization (WHO) country Office for India. Standards for TB Care in India. WHO; 2014. [Accessed March 1, 2023]. Available from: https://apps.who.int/iris/bitstream/handle/10665/208894/stci_book.pdf
Indian Council of Medical Research. National TB prevalence survey 2019–2021. ICMR;2022[Accessed March 1 2023]. Available from: https://tbcindia.gov.in/showfile.php?lid=3659
Arinaminpathy N, Batra D, Khaparde S. The number of privately treated tuberculosis cases in India: an estimation from drug sales data. Lancet Infect Dis. 2016;16(11):1255–60.
Stallworthy G, Dias HM, Pai M. Quality of tuberculosis care in the private health sector. J Clin Tuberc Other Mycobact Dis. 2020;20:100171.
Kwan A, Daniels B, Saria V. Variations in the quality of tuberculosis care in urban India: a cross-sectional, standardized patient study in two cities. PLoS Med. 2018;15(9):e1002653.
Rupani MP, Shah CJ, Dave JD, Trivedi AV, Mehta KG. ‘We are not aware of notification of tuberculosis’: A mixed-methods study among private practitioners from western India. Int J Health Plann Manag. 2021;36(4):1052–68.
Satyanarayana S, Subbaraman R, Shete P, et al. Quality of tuberculosis care in India: a systematic review. Int J Tuberc Lung Dis. 2015;19(7):751–63.
Government of India. Ministry of health and family welfare (MOHFW). Central TB Division. National Strategic Plan for tuberculosis elimination 2017–2025. MOHFW; 2017. [Accessed March 1, 2023]. Available from: https://tbcindia.gov.in/WriteReadData/NSP%20Draft%2020.02.2017%201.pdf
Ministry of Health and Family Welfare. India TB Report 2022.CTD. [Accessed January 10,2023]. Available from: https://tbcindia.gov.in/WriteReadData/IndiaTBReport2022/TBAnnaulReport2022.pdf
Government of India. Ministry of Health and Family Welfare. Gazette of India notification G.S.R. 588(E). 2013. Drugs and cosmetics (fourth amendment) rules, 2013 [Accessed January 1, 2023].Available from: https://thehealthmaster.com/wp-content/uploads/2020/10/GSR-No.-588E-Dt-30-08-2013-Schedule-H1-Drugs-DC-fourth-Amendment-Rules-2013.pdf
Government of India. Ministry of Health and Family Welfare. National Tuberculosis Elimination Programme. NIKSHAY. [Accessed March 1, 2023]. Available from: https://www.nikshay.in/
Government of India. Ministry of Health and Family Welfare. Direct Benet Transfer Manual for National Tuberculosis Elimination Programme. [Accessed March 1, 2023]. Available from: https://tbcindia.gov.in/WriteReadData/l892s/23294204DBTManualForNTEP.pdf
Government of India. Ministry of health and family welfare. Gazette of India notification GSR 588(E). 2013. [Accessed March 1, 2023] https://thehealthmaster.com/wp-content/uploads/2020/10/GSR-No.-588E-Dt-30-08-2013-Schedule-H1-Drugs-DC-fourth-Amendment-Rules-2013.pdf
Government of India. Ministry of health & family welfare. Guidance document on partnerships 2019. [Accessed March 1, 2023] Available from: https://tbcindia.gov.in/WriteReadData/l892s/9531588006Guidance%20Doucument%20on%20Partnerships%20RNTCP%202019.pdf
Government of India, Ministry of Health & Family Welfare (MOHFW), Central TB Division. Report of the joint monitoring Mission. Revised National Tuberculosis Control Programme November 2019. MOHFW; 2019. [Accessed March 5, 2023]. Available from: https://tbcindia.gov.in/showfile.php?lid=3536
Government of Kerala Department of health and family welfare. Making the SDG a reality. Government of Kerala; 2021. [Accessed March 1, 2023]. https://www.keralahealthconference.in/e-Book.pdf
Government of Kerala. Kerala Health Conference-Making the SDG A reality—moving towards TB elimination—4 march 2021. [Video Recording]. Thiruvananthapuram: GOK. 2021. [Accessed March 4, 2023]. Available from: https://www.youtube.com/watch?v=C4Yr_FTMdgQ&t=3452s
Jeyashree K, Thangaraj J, Rade K, Modi B, Selvaraju S, Velusamy S, et al. Subnational TB claims verification group. Estimation of tuberculosis incidence at subnational level using three methods to monitor progress towards ending TB in India, 2015-2020. BMJ Open. 2022;12(7):e060197. https://doi.org/10.1136/bmjopen-2021-060197.
George LS, Rakesh PS, Sunilkumar M, Vijayakumar K, Kunoor A, Kumar VA. TB patient support systems in Kerala: A qualitative analysis. Indian J Tuberc. 2021;68(1):9–15. https://doi.org/10.1016/j.ijtb.2020.11.005. Epub 2020 Nov 7
Manju R Nair, Ravi Prasad Varma. Availability, distribution and utilisation of health care services in Kerala. Thiruvananthapuram. 2021. [Accessed March 7, 2023] Available from: https://spb.kerala.gov.in/sites/default/files/inline-files/AvailDistribUtilisationHSKerala.pdf
World Health Organisation. The private health sector: an operational definition. Geneva. 2020. [Accessed on March 7, 2023]. Available from: https://www.who.int/docs/default-source/health-system-governance/private-health-sector-an-operational-definition.pdf
Kumar MK, Dewan PK, Nair PK, et al. Improved tuberculosis case detection through public-private partnership and laboratory-based surveillance, Kannur District, Kerala, India, 2001–2002. Int J Tuberc Lung Dis. 2005;9(8):870–6.
World Health Organization (WHO). Public–Private Mix for DOTS Global Progress. Report of the Second Meeting of the PPM Subgroup for DOTS Expansion. WHO; 2004. [Accessed April 17, 2023].Available from: https://apps.who.int/iris/handle/10665/68619
Ferroussier O, Kumar MK, Dewan PK, Nair PK, Sahu S, Wares DF, et al. Cost and cost-effectiveness of a public-private mix project in Kannur District, Kerala, India, 2001-2002. Int J Tuberc Lung Dis. 2007 Jul;11(7):755–61.
Greaves F, Ouyang H, Pefole M, MacCarthy S, Cash RA. Compliance with DOTS diagnosis and treatment recommendations by private practitioners in Kerala, India. Int J Tuberc Lung Dis. 2007;11(1):110–2.
Chugh S. IMA GFATM RNTCP PPM project: milestones in sight one year after. J Indian Med Assoc. 2008;106(7):454–8.
Rakesh PS, Balakrishnan S, Jayasankar S, Asokan RV. TB management by private practitioners – is it bad everywhere? Indian J Tuberc. 2016;63(4):251–4. https://doi.org/10.1016/j.ijtb.2016.09.009.
Ps R, Balakrishnan S, Ramachandran R, Nandhan S, Samuel NI, Pp P, et al. Using a pharmacy-based surveillance system to improve standards for TB Care in Kerala. India Glob Health Sci Pract. 2021;9(4):846–54. https://doi.org/10.9745/GHSP-D-21-00346.
Government of Kerala. Kerala TB Elimination Mission. August 2017. [Accessed on March 2, 2023] Available online: https://dhs.kerala.gov.in/wp-content/uploads/2021/01/KeralaTB-Elimination-Mission_Strategy-activity-plan-and-budget..pdf.
Balakrishnan S, Rakesh PS, Sunilkumar M, Sankar B, Ramachandran R, Ameer KA, et al. STEPS: A solution for ensuring standards of TB Care for Patients Reaching Private Hospitals in India. Glob Health Sci Pract. 2021;9(2):286–95. https://doi.org/10.9745/GHSP-D-20-00449.
Rakesh PS, Balakrishnan S, Sunilkumar M, Alexander KG, Vijayan S, Roddawar V, et al. STEPS - a patient centric and low-cost solution to ensure standards of TB care to patients reaching private sector in India. BMC Health Serv Res. 2022;2(1):2. https://doi.org/10.1186/s12913-021-07342-y.
Rakesh PS, Nair S, Philip S, Varma RP. Barriers for involvement of private doctors in RNTCP – qualitative study from Kerala, India. J Family Med Prim Care. 2019;8(1):160–5. https://doi.org/10.4103/jfmpc.jfmpc_208_18.
Philip S, Isaakidis P, Sagili KD, Meharunnisa A, Mrithyunjayan S, Kumar AM. "They know, they agree, but they don't do"--the paradox of tuberculosis case notification by private practitioners in Alappuzha district, Kerala, India. PLoS One. 2015;10(4):e0123286. https://doi.org/10.1371/journal.pone.0123286.
Kunoor A, James PT, Raj M, Rajesh CT, Nair P, Rakesh PS. Outcomes of patients treated with individualised anti-tuberculosis regimens in a tertiary care center in India. Public Health Action. 2017;7(4):308. https://doi.org/10.5588/pha.17.0062.
Nair P, James PT, Kunoor A, Rakesh PS. How we ensured 100% TB notification: experiences from a private tertiary care hospital in India. Public Health Action. 2017;7(2):179–80. https://doi.org/10.5588/pha.16.0128.
Khobragade RN, Kelkar RU, Sunilkumar M, Cency B, Murthy N, Surendran D, et al. Health system resilience: ensuring TB services during COVID-19 pandemic in Kerala. India Indian J Tuberc. 2022;69(4):427–31. https://doi.org/10.1016/j.ijtb.2021.10.004. Epub 2021 Oct 13y
Government of India, Ministry of Health & family welfare, National Tuberculosis Elimination Programme (NTEP). Universal access to TB care (UATBC): concurrent assessment report. NTEP; 2016. [Accessed March 9, 2021]. Available from: https://tbcindia.gov.in/index1.php?sublinkid=4711&level=3&lid=3265&lang=1.
Shibu V, Daksha S, Rishabh C, Sunil K, Devesh G, Lal S, et al. Tapping private health sector for public health program? Findings of a novel intervention to tackle TB in Mumbai. India Indian J Tuberc. 2020;67(2):189–201.
World Health Organisation. Engaging the private health service delivery sector through governance in mixed health systems: strategy report of the WHO advisory group on the governance of the private sector for universal health coverage. Geneva: WHO; 2020. [Accessed on Feb 3,2023]. Available from: https://www.who.int/activities/strengthening-private-sector-engagement-for-uhc
Initiative for Promoting Affordable and Quality TB Tests (IPAQT). [Online] Available at: https://healthmarketinnovations.org/program/initiative-promoting-affordable-and-quality-tb-tests-ipaqt
Central TB Division. Training modules (5-9) for programme managers & medical officers. New Delhi July 2020. [Accessed on March 3, 2023] Available from: https://tbcindia.gov.in/WriteReadData/NTEPTrainingModules5to9.pdf
Acknowledgements
Nil
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
PSR & MS have substantial participation in the conception, design, collection of data, analysis and interpretation of the data. PSR wrote the manuscript, MS reviewed and edited it. Both approved the final version of the paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study involves human participants. The study was approved by institutional review board and ethics committee of Amity University, Noida, India. Participants gave written informed consent to participate in the study before taking part.
Consent for publication
Not Applicable as no personal information regarding participants are revealed.
Competing interests
PS Rakesh was closely associated with the state TB Elimination program, Kerala in multiple roles such as WHO consultant & State Technical consultant for IMA-GFATM-RNTCP-PPM Project and was part of all major recent initiatives for private sector engagement. He also contributed to most of the studies and evaluations regarding private sector engagement for TB care in the state, which were mentioned in the current study. This could be a potential personal conflict of interest as his views and ideologies can influence this research.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Material 1.
Abstract in Malayalam.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rakesh, P.S., Shannawaz, M. Ensuring universal access to quality care for persons with presumed tuberculosis reaching the private sector: lessons from Kerala. Int J Equity Health 23, 101 (2024). https://doi.org/10.1186/s12939-024-02151-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12939-024-02151-1